Research Article, J Diagn Tech Biomed Anal Vol: 6 Issue: 1
Development of Medical Infrared Imaging Protocol for the Emergency Department
Coats TJ1*, Naseer S1, Charlton M2, Keresztes K3, Hussain S1, Dexter K4, Thompson JP2 and Sims MR3
1Emergency Medicine Academic Group, Department of Cardiovascular Sciences, University of Leicester, UK
2Anaesthesia Critical Care and Pain Management, Department of Cardiovascular Sciences, University of Leicester, UK
3Space Research Centre, Department of Physics and Astronomy, University of Leicester, UK
4Department of Physics and Astronomy, University of Leicester, UK
*Corresponding Author : T.J Coats
Emergency Medicine Academic Group,University of Leicester, Jarvis Building, Leicester Royal Infirmary, Infirmary Square, Leicester, United Kingdom
Tel: +44 (0) 116 258 5965
E-mail: tc61@le.ac.uk
Received: March 20, 2017 Accepted: April 29, 2017 Published: May 03, 2017
Citation: Coats TJ, Naseer S, Charlton M, Keresztes K, Hussain S, et al. (2017) Development of Medical Infrared Imaging Protocol for the Emergency Department. J Diagn Tech Biomed Anal 6:1. doi: 10.4172/2469-5653.1000119
Abstract
Objective: Medical Infrared Imaging (MII) is an investigative method that can be used to non-invasively detect specific heat signatures associated with disease, with a potential to be used in emergency care. There are no existing protocols for the use of MII in the Emergency Department (ED), and it is not known if this procedure is feasible in an ED setting. Methods: To determine the optimum protocol a preliminary study was conducted on 20 healthy volunteers. The right and left arms were imaged in Thermal Infra-Red (TIR), in a series of positions (anterior and posterior surfaces). TIR video recording of both arms held in extension (2 minutes) was also conducted. Results: Gender, side of body and length of time held in extension did not significantly affect the thermal images. There were significant differences between the anterior and posterior views of the arm, so this should be standardised. Conclusions: A standardised, yet practical protocol has been successfully developed. This ‘Leicester ED MII Protocol’ is proposed as the standard for future thermography in emergency care, to allow studies to be comparable, and now requires feasibility testing in the emergency care environment.
Keywords: Thermography, Diagnostic imaging, Emergencies, Diagnostic tests and procedures
Introduction
Thermography is a non- invasive investigational method that uses infrared radiation to detect heat patterns across the skin [1]. The distribution and intensity of heat across the body depends on three factors; (a) Internal heat production or fever, (b) the underlying anatomy of the blood vessels, as movement of blood also moves heat out from the body core, and (c) changes in vasomotor processes, which change the pattern of blood (and therefore heat) distribution around the body. The underlying metabolic and cardiovascular state creates changes in these factors, which in turn give rise to differences in core temperature and the spatial thermal distribution across the body.
Temperature measurement has been a cornerstone of medical diagnosis for more than 100 years [2,3]. Current routine clinical temperature measurements can be made in a number of body locations, each of which has advantages and disadvantages, with oral temperature measurement most accurately correlating to core temperature measured by pulmonary artery catheter or oesophageal probe [4,5]. Tympanic temperature has become routine due to its speed and ease of use, however the temperature measured may be unreliable due to factors such as ear wax and poor technique [6]. Non-contact temperature measurement on the forehead does not correlate well with rectal temperature [7]. More invasive temperature measurement using rectal or bladder thermometers, while more reliable, are not sensitive to rapid fluctuation in temperature.
Recent advances in thermal infra-red (TIR) imaging allow much higher resolutions, (640 by 480 pixels or greater), with increased sensitivity (30-40 mK temperature differences). These advances in technology allow accurate mapping of the heat distribution across the body, which has the potential to give more diagnostic information than the conventional single point measurement of temperature. Medical Infrared Imaging (MII) has been used in the detection of disease states such as breast cancer [8], for measurement of joint inflammation and damage [9], and is widely used to screen for infectious disease in travellers. However there have been no standardised protocols developed for the use of MII in the ED.
Existing MII thermography protocols have been conducted in strictly controlled laboratory-type environments, using mainly healthy volunteers as recruits or using limited numbers of ambulatory patients [10]. However, it is not possible to move acutely unwell patients into a laboratory, and is not possible to create such tightly controlled conditions within an ED. Therefore, before the potential clinical utility of thermography can be explored, a sufficiently standardised, yet practical protocol for imaging has to be developed.
There are a large number of variables that might affect a thermal image. This study performed a series of investigations to determine the best balance between rigour of measurement and the practical constraints of imaging in an Emergency Department. From the beginning it was decided to develop a protocol that only imaged the arm, as many emergency care patients are unable stand up, and imaging from above is not practical. In nearly all ED patients an arm can be easily exposed and imaged while the patient is sitting on a trolley. From the existing literature and a knowledge of the imaging conditions in the ED we chose to evaluate the effect of (a) arm position, (b) surface of the arm (anterior or posterior), (c) left or right arm and (d) the time that the arm was held outstretched, to see if these factors had a significant effect on thermal patterns (and so would have to be controlled for in the final protocol). Our overall objective was to develop a new protocol for MII suitable for testing in the Emergency Department.
Methods
To develop a practical protocol in the ED environment an initial set of studies were conducted on healthy volunteers. The arm was chosen as the region of interest as it seemed to be the most practical option for limb imaging in an Emergency Department, and its temperature distribution was known to change in disease states.
Over a 4-week period (October to November 2012), 20 healthy volunteers were recruited from University of Leicester students and staff. The study was approved by the University of Leicester Research Ethics Committee. Subjects were recruited on the basis of availability and absence of acute illness.
Room temperature was maintained between 20–24˚C and humidity was controlled to ensure a level less than 50%. External light and heat sources were removed via blackout blinds. A forward looking infrared (FLIR) SC620 camera with thermal sensitivity of <0.04°C at 30°C, being operational within a temperature range of -40°C to +500°C was used for imaging. Internal stabilisation of the system was performed by switching on the TIR Imager at least 2 hours before imaging. The imager was directly connected to a standard laptop running FLIR software, enabling real time image monitoring, processing and saving.
Each imaging session lasted 40 minutes. Subjects were asked to expose both arms, from shoulder tip to fingertip, including the removal of jewellery and clothing. There was then a 15-minute acclimatisation period to the new environment. Nine aluminium adhesive markers, 3 mm x 5 mm, were attached to predefined anatomical points on the arm (Table 1). The markers have a lower heat emissivity than skin so reflect ambient air temperature and so appear thermally colder (black in the image thermal range) than the adjacent skin. The markers were used to define regions of interest (ROI’s) for post-processing (data extraction from the images).
| 1 | Acromiclavicular joint |
| 2, 3 | Elbow skin crease anterior medial / lateral |
| 4, 5 | Elbow skin crease posterior medial / lateral |
| 6,7 | Wrist anterior medial / lateral |
| 8, 9 | Wrist posterior medial / lateral |
Table 1: Location of aluminium adhesive markers.
Subjects were asked to sit on a stool and rest their arm on a stand. The armrests, camera tripod and stools were arranged in standardised positions to maintain a fixed distance between the camera and the subject of two meters to allow inter and intra-subject standardisation. The imager was mounted and fixed onto a tripod to standardise the camera angle at which images were acquired. The imager was manually focused and calibrated prior to each image taken.
Both left and right arms were imaged from front and back with the upper arm horizontal and the forearm and hand either (1) pointing up, (2) horizontal or (3) pointing down. The front and back of each arm was imaged in three positions in the same order between volunteers. Each arm then had thermal video recorded for 2 minutes while held in a horizontally extended position. All volunteers completed the protocol without any discomfort.
Analysis
The thermograph images were produced as artificially coloured maps of heat distribution, with each coloured pixel representing a single temperature point measurement. Images were standardised and stored for data extraction. A colour gradient scale bar was produced with each image; a white colour demonstrated warmest areas, whereas a black colour indicated cooler regions.
Data were extracted from the raw images using bespoke IDL (Interactive Data Language) software which removed the background noise and prompted the user to select 5 points – at the fingertip of the middle finger, the midpoint of the base of the middle finger, the midpoints across the wrist, the midpoint of the ante-cubital fossa and a point one third of the distance from the acromio-clavicular joint to the axilla. A straight line, joining all of these points was generated and raw temperature from each pixel along this line was extracted from the image. This line was made up on average, of over 500 point readings for the length of the whole arm (Figure 1). Therefore to enable statistical analysis the line was divided into finger, hand, forearm and upper arm, and the median temperature was calculated for each of these regions.
Analysis was carried out using GraphPad Prism (version 6.0, GraphPad Software, California USA), SPSS (version 20.0, IBM, USA) and Microsoft Excel 2010. Data sets were tested for normality using the Shapiro-Wilks test. Parametric data were compared using either a paired or an unpaired student’s t-test with Bonferroni correction for multiple testing, p<0.01 considered as significant.
Results
Twenty volunteers were recruited with a mean age of 27 years (standard deviation 10 years). Gender distribution was equal, and volunteers were predominantly right handed (85%). The timing of the imaging sessions varied throughout the day (60% took place between 1200-1600 hours).
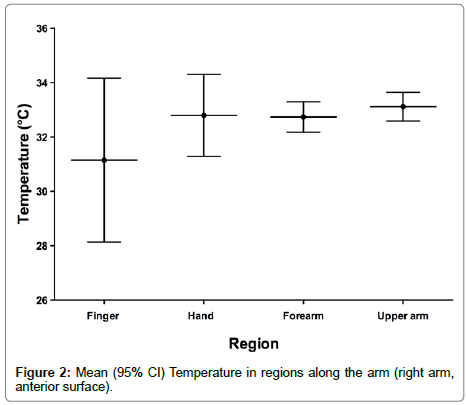
When analysing regional variation, the arm was divided into 4 sections (finger, hand, forearm and upper arm). As expected the fingers tended to be cooler with a larger variation (Figure 2). No statistically significant differences in gender were found, with mean male temperature of whole arm being 31.4°C (SD=3.5°C) compared with 30.9°C (SD 2.5°C) in females (unpaired t-test, p=0.7). No statistically significant inter-gender regional differences were found.
The difference of 1.2°C between the mean temperatures of anterior (32.8°C +/- 0.6°C) and posterior (31.6°C +/- 0.7°C) surface temperature was statistically significant (paired t-test, p<0.0001).
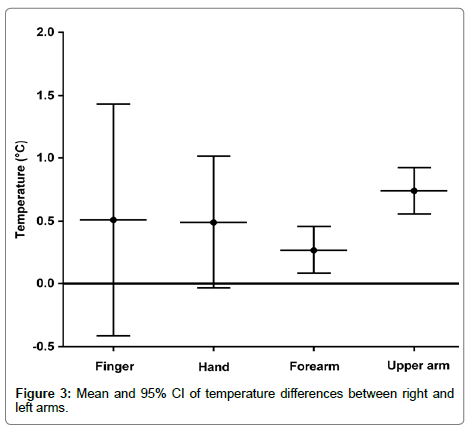
The anterior surface data for each arm was used to calculate a mean temperature along each arm. The mean temperature of the right arm (32.9°C) was warmer than the left arm (32.45°C), but this difference was not statistically significant (paired t-test p=0.04). In every subject, the right arm temperature was warmer than or equal to the left arm temperature. The trend to a warmer right arm of about 0.5°C was present in all areas of the arm (Figure 3).
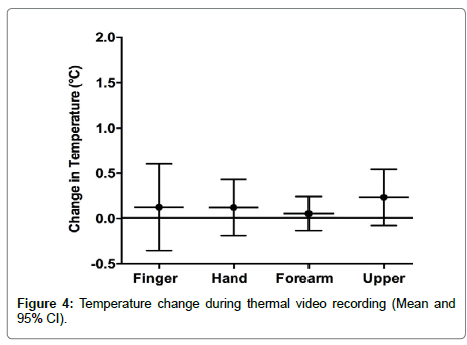
Thermal signature change with arm held in extension
The mean temperatures from each subject’s start and end image were calculated. There was a non-significant trend (0.2°C, or less) in all areas of the arm (Figure 4).
Protocol derived from volunteer study
The volunteer study showed that an Emergency Department Medical Infrared Imaging protocol need not control for gender or side of body (as these factors did not have a large effect), but should image a consistent surface of the arm (as anterior and posterior were different). We chose the anterior view, as this seemed more convenient for an ED patient sitting on a trolley. We found that the arm need not be held in a fixed position prior to imaging (no change during the thermal video). For ease of subsequent data extraction (by edge detection software) we chose a horizontally extended arm position for the standard Leicester ED MII protocol (Box 1).
An additional practical point from this volunteer study was that the initial images had a lot of background ‘noise’ caused by the various equipment present. Hanging a sheet behind the subject eliminated this noise and gave a uniform thermal background, thus enabling cleaner looking images and easier edge detection for the software processing of the images.
Discussion
The main aim of this volunteer study was to derive a practical yet standardised protocol for MII imaging in a clinical setting. The study has shown, for the first time, the gradient of temperature along the length of the arm and defined the variation in normal health. The greatest variation between individuals was in the hand / finger regions as expected, probably simply explained by individual differences in local circulation or differences in the systemic vascular resistance of recruits. This finding was expected from previous thermography studies [11], and is a common clinical observation. Likewise when comparing gender and temperature levels our results seem to correspond with previous literature [3], but absolute differences were small. This implies that future protocols for diagnostic ED MII research may not need to take account of sex differences.
The significant difference between the anterior and posterior surfaces of the arm has not been previously described, and is likely to be related to the anatomical distribution of upper limb blood vessels, with the main arteries, bringing heat from the body core, being anterior. On the posterior surface, the blood vessels are smaller and run below the bone and muscle, so heat signatures are weaker. This illustrates that the anatomy of heat distribution is related to the anatomy of blood flow. The difference between surfaces implies that this is a factor that should be kept constant in future studies. As we think that imaging the anterior surface will be much easier than posterior due to the space confines of an ED cubicle, we suggest that an anterior arm view becomes the future standard.
The small difference in thermal signature between left and right arms might also be related to anatomical variation. The subclavian artery supplies blood to the upper limbs bilaterally, however, the branch to the left arm leaves the aortic arch at a more distal point to that of the right. This difference in temperatures could however be due to chance in our small sample, as some healthy individuals have an inter-arm difference in blood pressure [12], and may also have a difference in flow. There might also be a relationship to hand dominance, as the dominant arm may have a greater muscle mass or blood supply. However differences were small (unlikely to be clinically significant). Only the right side of the body is readily accessible in an ED cubicle (as the clinical convention of examination of the patient from their right hand side means that the patient’s left side is usually against a wall). For these practical reasons we suggest that imaging only the right arm becomes the future standard.
There have been no previous studies about the thermal effect of keeping the arm in an extended position for a certain period of time. We had predicted that keeping the arm outstretched could cause muscle contractions, which could increase temperature. However, the change identified using thermal video was so small that is not a factor that needs to be considered in future.
Given the constraints of the emergency care environment, it will never be possible to fully conform to the laboratory standards set for MII [13,14]. We have standardised as far as possible, but incomplete standardisation may introduce variability or ‘noise,’ which might limit the practical utility of the ‘Leicester ED MII Protocol’ (Box 1). The feasibility of this Protocol needs to be tested in the real emergency care environment.
References
- Jones BF (1998) A reappraisal of the use of infrared thermal image analysis in medicine. IEEE Trans Med Imaging 17: 1019-27.
- Mackowiak PA, Worden G (1994) Carl Reinhold August Wunderlich and the evolution of clinical thermometry. Clin Infect Dis 18: 458-67.
- Mackowiak PA, Wasserman SS, Levine MM (1992) A critical appraisal of 98.6 degrees F the upper limit of the normal body temperature and other legacies of Carl Reinhold August Wunderlich. JAMA 268: 1578-80.
- Hooper V, Andrews J (2006) Accuracy of noninvasive core temperature measurement in acutely ill adults: the state of the science. Biol Res Nurs 8: 24-34.
- Jefferies S (2011) A systematic review of the accuracy of peripheral thermometry in estimating core temperatures among febrile critically ill patients. Crit Care Resusc13: 194-9.
- Barnett BJ, Nunberg S, Tai J, Lesser ML, Fridman V, et al. (2011) Oral and Tympanic Membrane Temperatures Are Inaccurate to Identify Fever in Emergency Department Adults. Western Journal of Emergency Medicine 12: 505-511.
- Fortuna EL, Carney MM, Macy M, Stanley RM, Younger JG, et al. (2010) Accuracy of non-contact infrared thermometry versus rectal thermometry in young children evaluated in the emergency department for fever. J Emerg Nurs 36: 101-104.
- Keyserlingk J (2013) Functional Infrared Imaging of the Breast: Historical Perspectives, Current Applications and Future Considerations, in Medical Infrared Imaging: Principles and Practices, M. Diakides, J. Bronzino, and D. Peterson, Editors., Tayolr & Francis: New York.
- Diakides, MJ, Bronzino, Peterson D (2013) Medical Infra-red Imaging Principles and Practices. CRC Press, Taylor Francis Group.
- Ring E, Ammer K (2000) The Technique of Infrared Imaging in Medicine. Thermology International10: 7-14.
- Zaproudina N, Varmavuo V, Airaksinen O, Närhi M (2008) Reproducibility of infrared thermography measurements in healthy individuals. Physiol Meas 29: 515-24.
- Orme S, Ralph SG, Birchall A, Lawson-Matthew P, McLean K (1999) The normal range for inter-arm differences in blood pressure. Age Ageing 28: 537-542.
- Ring E (2013) New standards for fever screening with thermal imaging systems. Journal of Mechanics in Med and Biol 13: 1350045.
- International Organisation for Standardisation (2009) Medical electrical equipment - Deployment, implementation and operational guidelines for indentifying febrile humans using a screening thermograph.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi