Case Report, J Clin Image Case Rep Vol: 5 Issue: 8
Diabetic Keto Acidosis and Hyperosmolar Hyperglycemic State, Diagnosis and Management Challenges at Regional Referral Hospitals, A Case Series from umbi Regional Referral Hospital, Pwani, Tanzania
Gembe A*, Bilaro E
Department of Internal Medicine Tumbi Regional Referral Hospital, Tanzania
*Corresponding Author: Adam Gembe
Department of Internal Medicine, Tumbi Regional Referral Hospital, Tanzania
Tel: 0716009131
E-mail: dr.adamgembe@gmail.com
Received: June 26, 2021 Accepted: July 28, 2021 Published: August 04, 2021
Citation: Gembe A, Bilaro E (2021) Diabetic Keto Acidosis and Hyperosmolar Hyperglycemic State, Diagnosis and Management Challenges at Regional Referral Hospitals, A Case Series from Tumbi Regional Referral Hospital, Pwani, Tanzania. J Clin Image Case Rep 5:8.
Abstract
Acute hyperglycemic syndromes are among common emergency department presentations in diabetic patients. In the developing world, still there are challenges in the diagnosis, management and monitoring of these cases hence high morbidity and mortality. A one-month case series is presented here, from Pwani region Tanzania, to demonstrate the encountered challenges.
Keywords: Diabetic ketoacidosis; Hyperglycaemia; Insulin; Diabetes Mellitus
Introduction
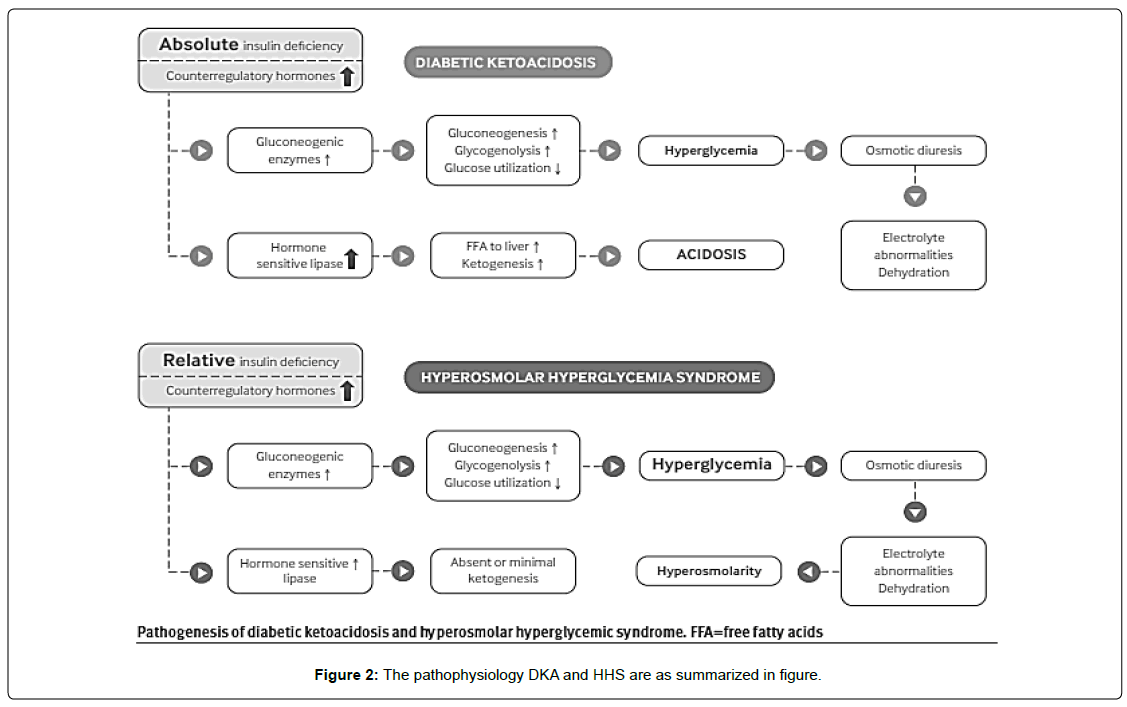
Diabetic ketoacidosis (DKA) is an acute complication of diabetes mellitus (DM) characterized by the triad of hyperglycaemia, ketosis, and metabolic acidosis. This is due to a relative or absolute deficiency of insulin and an excess of counter-regulatory hormones including glucagon, cortisol, catecholamines and growth hormones, leading to hyperglycaemia, glycosuria, dehydration, and hyper-osmolality of varying severity [1].
On the other hand, hyperosmolar hyperglycemic state (HHS) is another acute DM complication characterized by high osmolality often >320 mOsm/kg, high blood glucose usually >30 mmol/L and severe dehydration [2].
The pathophysiology DKA and HHS are as summarized in Figures 1 and 2 below [3].
The prevalence of the two grave complications of DM (DKA and HHS) displays a variable pattern across the globe.
In the United States, DKA is more common than HHS. Most patients with DKA are young adults aged 18-44 years as well as adults with type 1 DM. In contrast, HHS patients were middle aged adults 45-64 years along with adults with type 2 DM [4]. Similar findings were observed in Ethiopia and South Africa where DKA was more prevalent than HHS [5-7]. Dissimilarly, HHS was more common than DKA in studies done in Benin and Nigeria [8].
The diabetic hyperglycemic crises are associated with significant mortality up to 30%. HHS is associated with higher mortality than DKA due to the fact that most patients are old age coupled with the presence of hyper-osmolality [7, 9,10].
Despite presence of well stipulated clinical oriented guidelines in managing these acute DM complications, still there are challenges in diagnosis and appropriate management in most primary health care facilities and regional referral hospitals at large in Tanzania.
A one-month case series is presented here from Tumbi Regional Referral Hospital (TRRH), Pwani, Tanzania to reflect the challenges faced in most regional hospitals.
Case 1
A 20 years old male referred from one of the satellite primary health facility with a diagnosis of diabetes mellitus for further management. The patient presented with a 2 days history of confusion that was preceded by polyuria, polydipsia and significant weight loss few weeks prior to hospital presentation. Furthermore, the informant (father) denied history of fever, convulsions, chronic medication use or a family history of diabetes. Examination findings the patient had a respiratory rate of 24 breath/min, weak pulse with a rate of 120 beats/ min, blood pressure 100/60 mmHg, temperature 36.80C, saturating at 96% in room air and Glasgow coma score of 14/15, wasted, no signs of meninges, equal pupils reacting to light. Other systemic examinations were unremarkable. Laboratory findings were as summarized in Table 1 below.
| Investigation | Results |
|---|---|
| Andom blood glucose | High |
| Arterial blood gases | Unavailable |
| Urinalysis | Ketones 3+, Negative leukocytes and nitrate, other parameters were normal |
| Malaria rapid diagnostic test | Negative |
| Full blood count | Normal |
| C-reactive protein | Unavailable |
| Electrolytes -Sodium -Others; Potassium, calcium, chloride, phosphate |
141 mmol/L Reagents out of stock |
| Renal function test -Creatinine -Urea |
69.9 µmol/L 3.62 mmol/L |
| Glycosylated hemoglobin | Reagents out of stock |
| Chest radiograph | Normal |
Table 1: Laboratory and Radiological findings of case 1.
The patient was diagnosed with diabetes with diabetes ketoacidosis admitted in our ICU where he was started on fluids and actrapid 6IU/hour via an infusion pump with progressive decreased in plasma glucose and improvement on his level of consciousness. Day 2 the patient was able to feed on his own and changed to a twice daily insulin therapy (mixterd insulin) 30IU in the morning and 16IU in the evening. Day 3 the family and the patients were given dietary education and counselled on means of administering insulin at home as well as their due date to come for follow up then they were discharged home on the 4th day.
Case 2
A 47 years old male diabetic and non-hypertensive on erratic use of metformin 500mg twice daily was referred from feeding satellite primary health facilities with a diagnosis of diabetes mellitus with acute hyperglycaemia. Upon arrival at our facility he had a 3days history of confusion and a day history of tonic clonic convulsions. No history of fever, headache, vomiting/diarrhoea prior the hospital presentation. On examination the patient was agitated, saturating at 88% in room air, temperature 37.80C, tachycardia with a pulse rate of 110 beats/minute and blood pressure 125/78. Systemic examination no meningeal signs, skin and appendages he had pustules on the right hand extending to the forearm with no features of active inflammation on the surrounding skin, dry skin on both feet and a bruise interdigital between the big toe and second toe. Respiratory system coarse crackles infrascapular bilaterally. Other systems were essential normal. Laboratory findings were as follows in Table 2 below.
| Investigation | Results |
|---|---|
| Random blood glucose | High |
| Arterial blood gases | Unavailable |
| Urinalysis | Ketones negative, Negative leukocytes and nitrate, other parameters were normal |
| Malaria rapid diagnostic test | Negative |
| Full blood count | Leukocytosis of 12.5 predominant neutrophils 9400, normocytic anemia of 8.5g/dl and normal platelet count |
| C-reactive protein | Unavailable |
| Electrolytes -Sodium -Others; Potassium, calcium, chloride, phosphate |
Reagents out of stock at this admission |
| Renal function test -Creatinine -Urea |
461 µmol/L 22 mmol/L |
| Glycosylated hemoglobin | Reagents out of stock |
| Chest radiograph | Pneumonia (see Figure 1) |
| Kidney, ureter and bladder ultrasound | Poor corticomedullary differentiation |
Table 2: Laboratory and Radiological findings of case 2.
The patient was started on short acting insulin at a rate of 7IU/ hour on day 1, fluid resuscitation and antibiotics (amoxicillin + clavunate) for the folliculitis and pneumonia. On day 3 fasting blood glucose was 6.5mmol/L and the patient had normal high centre examination findings. He was started on twice daily insulin regime. Day 4, the patient was referred to a nephrologist at the national hospital to continue with renal clinic and further management.
Case 3
A 26 years female, diabetic with poorly controlled recorded blood glucose on her primary health care facility card, on erratic use of metformin, referred from a primary health facility with a referral diagnosis of diabetes mellitus with coma. Upon arrival to our facility she had a 3-month history of amenorrhea, polyuria, and polydipsia associated with general body weakness and significant weight loss. 3-days prior referral, the patient had confusion that was letter followed by loss of consciousness. At admission the GCS was 10/15, random blood glucose 31 mmol/L, tachycardia of 110 beats/min, SPO2 92% in room air and blood pressure of 100/60 mmHg. Further neurological exam no meningeal signs. Laboratory and radiological findings were as follows in Table 3 below.
| Investigation | Results |
|---|---|
| Random blood glucose | 31mmol/L |
| Arterial blood gases | Unavailable |
| Urinalysis | Ketones 4+, Negative leukocytes and nitrate, other parameters were normal |
| Urine pregnancy test | Positive |
| Malaria rapid diagnostic test | Negative |
| Full blood count | Leukocytosis of 13.1 predominant neutrophils 8400, Normocytic anemia HB 9.4g/dl and thrombocytosis of 500 |
| C-reactive protein | Unavailable |
| Electrolytes -Sodium -Others; Potassium, calcium, chloride, phosphate |
Reagents out of stock at this admission |
| Renal function test -Creatinine -Urea |
102 µmol/L 13 mmol/L |
| Glycosylated hemoglobin | Reagents out of stock |
| Chest radiograph | Normal |
| Pelvic Ultrasound | Non-viable fetus |
Table 3: Laboratory and Radiological findings of case 3.
The patient was admitted into the ICU where short acting insulin at a rate of 6IU/hour, fluid resuscitation and a broad spectrum antibiotic were started. Day 2, the patient random blood glucose was 8mmol/L and she had an improved GCS 14/15, evacuation of the foetus was done and the patient was taken back to ICU. Day 3, she was fully conscious, transferred out of ICU and a twice daily insulin regime was initiated. Diabetic counselling to the family and patient was carried by the hospital nutritionist. The patient completed a 7-days antibiotic course and discharged home with twice daily insulin therapy.
Discussion
This case series describes three patients who were admitted at Tumbi RRH with acute hyperglycemic complications of diabetes. In an ideal setting, the diagnosis of DKA and HHS requires both clinical symptoms and supporting laboratory investigations.
The following should be evaluated: plasma levels of electrolyte, anion gap, plasma glucose (PG), creatinine, osmolality and betahydroxybutyric acid (beta-OHB) (if available), blood gases, serum and urine ketones, fluid balance, level of consciousness, precipitating factors and complications [11].
With regard to the case series presented above, still DKA and HHS diagnosis formulation based on clinical symptoms poses a great challenge in many primary health care facilities., The diagnosis of DKA and HHS, at regional referral hospital level, is clinical based with a few available laboratory investigations. Exemplified by the above presented clinical cases, the absence of essential laboratory investigations, inability to afford investigation costs (by patients) and frequent reagent stock outs are the utmost tabled reasons. These findings were reflected in most of the studies in Sub Saharan Africa where mortality due to DKA and HHS was reported higher than developed world. This has been attributed to delayed diagnosis and inadequate monitoring of patients [12].
Unavailability of Blood Gases and other investigations poses a challenge on the clinical decisions especially on proper time to stop fixed rate insulin infusion, and starting twice a day insulin doses, similarly some early predictors of serious complications may be missed [11].
Patient with conditions like, pregnant women, elderly, and those with serious co morbidities like chronic kidney disease are at a far greater risk of complications and deserve special consideration when presenting with acute hyperglycaemia, early detection of these cases will prevent these complications through rising community and first line health care workers awareness.
Our case series also emphasizes on the importance of patient education on prevention of the acute hyperglycemic complications, as it has been reported in other studies, the most common precipitant is missed medications for diabetes [12]. More counselling is still needed at primary health facilities to reduce admissions.
Conclusion
With reference to the foretasted case series, it will be correct to extrapolate from the above findings and argue that, acute hyperglycemic syndromes management remains inadequately addressed at health care facility setup, in our region, hence leading to increased morbidity and mortality.
Therefore, it will be appropriate, at this time, to execute outreach programs to satellite health care facilities to empower clinicians with abilities to promptly diagnose these acute hyperglycemic syndromes and provide initial management before transferring these patients to facilities where adequate management can be provided.
Diagnostic tools such as ketone blood meters or urine deep sticks should be made available at primary health facilities. It is crucial too to ensure sustainable reagents availability at regional referral hospital level to enable adequate diagnosis and patient monitoring.
References
- Tran TTT, Pease A, Wood AJ, Zajac JD, Mårtensson J, et al. (2017) Review of evidence for Adult Diabetic Ketoacidosis Management Protocols.1–13.
- Topics C (2015) The management of the hyperosmolar hyperglycaemic state in adults with diabetes: a summary of a report from the Joint British Diabetes Societies for Inpatient Care. 15(2): 89–93.
- French EK, Donihi AC, Korytkowski MT, (2019) Diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome: review of acute decompensated diabetes in adult patients.365: I1114.
- Benoit SR, Hora I, Pasquel FJ, Gregg EW, Albright AL, et al. (2020) Trends in Emergency Department Visits and Inpatient Admissions for Hyperglycemic Crises in Adults With Diabetes United States. 43(5): 1057-1064.
- Bedaso A, Oltaye Z, Geja E, Ayalew M (2019) Diabetic ketoacidosis among adult patients with diabetes mellitus admitted to emergency unit of Hawassa university comprehensive specialized hospital. BMC Res Notes,12(1): 137.
- Syndrome M, Negera GZ, Weldegebriel B, Fekadu G (2020) Acute Complications of Diabetes and its Predictors among Adult Diabetic Patients at Jimma Medical Center Southwest Ethiopia. 13: 1237–1242.
- Ekpebegh CO, Akinrinmade A, Badri M, Levitt NS (2010) O RIGINAL A RTICLES Hyperglycaemic crisis in the Eastern Cape province of South Africa: High mortality and association of hyperosmolar ketoacidosis with a new diagnosis of diabetes.100(12): 822–826.
- Hospital T, Uche G, Iloh P, Amadi AN (2018) Epidemiology of Diabetic Emergencies in the Adult Emergency Department of a Epidemiology of Diabetic Emergencies in the Adult Emergency Department of a Tertiary Hospital in South-Eastern Nigeria.
- Pasquel FJ, Umpierrez GE (2014) Hyperosmolar Hyperglycemic State: A Historic Review of the Clinical Presentation Diagnosis and Treatment. 37(11): 3124–3131.
- Macisaac RJ, Lee LY, Mcneil KJ, Tsalamandris C, Jerums G, et al. (2002) Influence of age on the presentation and outcome of acidotic and hyperosmolar diabetic emergencies. 32(8): 379-385.
- Suwarto S, Sutrisna B, Herdiman PT(2014) Predictors of Five Days Mortality in Diabetic Ketoacidosis Patients: a Prospective Cohort Study.46(1): 18-23.
- Abdus S, Aftab S, Alotaibi MS, Alghamdi ALIA (2011) Clinico-laboratory characteristics of diabetic keto acidosis in adults in a.15(10): 1202–1206.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi