Case Report, J Spine Neurosurg Vol: 10 Issue: 5
Diagnostic Conundrums in Cerebellar Cryptic Arteriovenous Malformations
Victor Kwasi1,2,3*, Ryoko Niwa1, Takayuki Hara1 and RM Damian Holsinger4
1 Department of Neurosurgery, Toranomon Hospital, Tokyo, Japan
2 Department of Japanese Council for Medical Training, Toranomon Hospital, Tokyo, Japan
3 Departments of Surgery, The University of Sydney, NSW, Australia
4 Departments of Pathology, The University of Sydney, NSW, Australia
*Corresponding Author: Dr Victor Kwasi
Department of Surgery, The University
of Sydney, Level 2, Medical Foundation Building, 92-94 Parramatta Road,
Camperdown, 2050, NSW, Australia
E-Mail: victor.kwasi@sydney.edu.au
Received date: April 8, 2021; Accepted date: April 23 2021; Published date: April 30, 2021
Citation: Kwasi V, Niwa R , Hara T, Holsinger RMD (2021) Diagnostic Conundrums in Cerebellar Cryptic Arteriovenous Malformations. J Spine Neurosurg 10:4.
Abstract
Cryptic Arteriovenous Malformations (AVM) have increased risks of re-bleeding but sometimes undetectable on conventional neuroimaging modalities, thus delaying definitive treatment. Bleeding into the confined space of the posterior cranial fossa poses increased risks of mortality due to increasing intracranial pressure and early detection and surgical resolution is of utmost urgency. We present a case of cerebellar cryptic AVM diagnosed using high-resolution cone beam Computerized Tomography angiography (CBCT-A) and three-Dimensional Rotational Angiography (3-DRA), with a definitive diagnosis confirmed on histology. Surgery was performed without complications and the patient resumed normal functioning.
Keywords: Cerebellar haemorrhage; High-resolution cone beam; Computerized tomography angiography; Threedimensional rotational angiography.
Introduction
The posterior cranial fossa is a confined space and an increase in the volume within the cranial cavity may be life-threatening [1].
Accurate diagnosis and timely neurosurgical interventions are important to prevent recurrent haemorrhage and mitigate the risks of increasing intracranial pressure. AVM is suspected when Magnetic Resonance Imaging (MRI) shows abnormal vessels proximal to the haematoma or angiography demonstrates a nidus, brush-like sign or early draining veins [2,3].
However, typical features are not always present and there is a possibility of AVM in acute intracranial bleeding diagnosed as hypertensive haemorrhage (based on radiological investigations showing no abnormalities in vessels). Abnormal vessels may be invisible due to compression by the acute haematoma.
Cryptic AVM were traditionally defined as less than two to three centimetres, clinically asymptomatic and with histological features of AVM. They were invisible on conventional radiological investigations including MRI, MRI angiography and DSA [4]. Currently, cryptic AVM are detectable due to modern advances in radiological imaging techniques and the definition has been evolving over time [5-7].
Advances in radiological techniques have allowed cryptic AVM to be detectable and therefore the definition has been evolving [8-10]. There is no uniformity in describing cryptic AVM10 and AVM not detectable on routine DSA is considered the best description [8].
We report the successful detection of a ruptured cryptic cerebellar AVM on CBCT-A and 3-DRA that permitted surgery to be performed safely in the acute phase.
Case Presentation
A 51-year-old man presented with gradual onset of left-sided temporal headaches. His vital signs were within normal ranges, except for blood pressure of 175/117 mmHg.
Cerebellar signs included mild left-sided dysmetria. He had laparoscopic resection of early stage sigmoid colon cancer nine years prior.
There was no history of anticoagulant use or bleeding tendencies. He was a smoker with above healthy limits alcohol intake but no history of psychoactive agents or illicit drugs usage, including opioids. His mother had a history of hypertension and subarachnoid haemorrhage due to a ruptured intracranial aneurysm aged 81. His father died of colon cancer.
Investigations
Routine lab tests were within normal ranges, including the coagulation profile. Chest X-ray and electrocardiogram were normal.
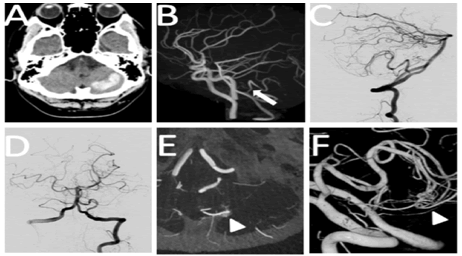
On CT scan there was 8 ml of hyper-dense lesions attributable to acute intracranial haemorrhage on his left cerebellar hemisphere (Figure 1A). Emergency surgery was not prescribed initially because the amount of the haematoma was considered minimal with no evidence of hydrocephalus.
T-2 MRI angiography demonstrated a hyper-intense lesion on the left cerebellar hemisphere consistent with acute haematoma (Figure 1B).
Focal dilatation and stenosis at the proximal segment of the left Posterior Inferior Cerebellar Artery (PICA) was noted.
Angiogram revealed no signs of PICA dissection such as double lumen signs and intimal flaps. Instead, AVM at the distal portion of the left PICA was suspected on CBCT-A and 3-DRA, but DSA imaging failed to depict early draining veins or nidus (Figure 1 (C, D and E))
3-DRA imaging demonstrated left vertebral artery vascular malformation in the middle segment of the left PICA (Figure 1F).
Figure 1: (A) CT scan on admission showing 8 ml of acute haemorrage on the left cerebellar hemisphere. (B) MRI angiography demonstrating focal dilation and stenosis on the proximal portion of left PICA (arrow). C and D: Lateral (C) and anteroposterior (D) views of the left vertebral artery angiogram with no significant findings. (E) High-resolution CBCT-A axial section with left vertebral artery injection demonstrating a brush-border like stain (arrowhead). (F) 3-DRA with left vertebral artery injection showing vascular malformation (arrowhead) at the middle portion of the left PICA.
Differential Diagnosis
Differential diagnoses for posterior cranial fossa haemorrhage include hypertensive haemorrhage, haemorrhagic infarctions, bleeding tumours, cavernous malformations, anticoagulants, arteriovenous fistulae, illicit drugs such as cocaine, amphetamines, heroin and ecstasy and, aneurysmal bleeding.
Surgery
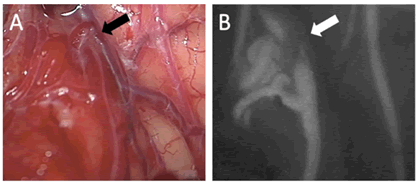
On day three, suboccipital craniotomy was performed and microscopic observation revealed a small nidus on the left caudal surface of the cerebellum. The cerebellar haematoma was evacuated for decompression and to enable better viewing for the AVM excision. Closer inspection showed one of the veins draining from nidus as a ‘red vein’ (Figure 2A). Intravenous indocyanine green injection revealed a 4 ml nidus but with no early draining veins (Figure 2B).
The nidus was safely removed, and gross total excision confirmed with repeat indocyanine green injection. The AVM cavity was connected to the haematoma cavity, which implied that the origin of bleeding was the AVM as opposed to PICA dissection and no further exploration of PICA was considered intra-operatively.
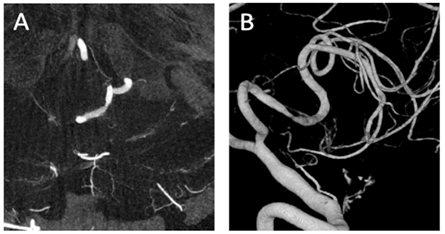
The patient reversed uneventfully from general anaesthesia with no neurological deficits, except for the persistence of dysmetria he presented with pre-operatively. Post-operative angiogram confirmed that there were no residual AVM and no radiological features of PICA dissection (Figures 3 (A and B)).
Results
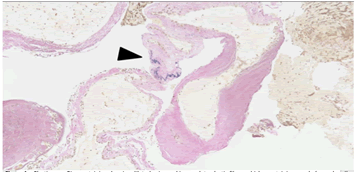
Histological examination using Elastica van Gieson stain revealed abnormal blood vessels. There were abnormally dilated veins with hyalinized and thickened walls but the direct changes from arteries into veins were not identified. One of the veins was noted to contain elastic fibers which a characteristic feature of arteries (Figure 4).
Following continuous lumbar drainage for 11 days due to subcutaneous swelling that was due to cerebrospinal fluid leakage from post-operative day 15, the patient was discharged home on day 31.
Discussion
In a relatively young patient presenting with posterior cranial fossa haemorrhage, a high index of suspicion for cryptic AVM as the underlying cause is important. CBCT-A and 3-DRA are considered useful imaging modalities for delineating cryptic AVM. DSA is the gold standard for diagnosing cryptic AVM. CBCT-A has high sensitivity in for ruptured AVM. MRI angiography is less invasive and radiation-free [2,6-8,10].
The annual re-bleeding risk is approximately 3%. Patients with ruptured cryptic AVM have a two-fold increased likelihood of rebleeding when compared to those with intact cryptic AVM. Risk factors for re-bleeding include history of prior haemorrhage, deeply seated AVM, AVM associated with aneurysms and AVM with exclusively deep venous drainage [3]. Posterior cranial fossa AVM are estimated to account for approximately 5% to 7% of all intracranial AVM, but the incidence of bleeding is relatively higher when compared to supratentorial AVM. Once acute haemorrhage occurs, mortality rate is as high as 13% [3,10]. We postulate that cryptic AVM are underestimated and increasing numbers of patients will be identified and treated appropriately due to higher resolution imaging.
Conclusion
Cerebellar cryptic AVM are important differentials for posterior cranial fossa haemorrhage, especially in younger patients. Higher resolution imaging like CBCT-A and 3-DRA should be considered for timely lifesaving neurosurgical interventions.
Acknowledgements
We would like to thank Dr Shinji Ito for the definitive histopathology diagnosis.
References
- Mokri B (2001) The Monro-Kellie hypothesis: Applications in CSF volume depletion. Neurology 56: 1746-1748.
- Rahal JP, Malek AM (2013) Benefit of cone-beam computed tomography angiography in acute management of angiographically undetectable ruptured arteriovenous malformations. J Neurosurg. 119: 1015-1020.
- Gross BA, Du R (2013) Natural history of cerebral arteriovenous malformations: A meta-analysis. J Neurosurg. 118: 437-443.
- Crawford JV, Russel DS (1956) Cryptic arteriovenous and venous harmatomas of the brain. J NeurolNeurosurg Psychiatry 19: 1-11.
- Dillon WP (1997) Cryptic vascular malformations: controversies in terminology, diagnosis, pathophysiology, and treatment. AJNR Am J Neuroradiol 18:1839-1846.
- Combaz X, Levrier O, Moritz J, Mancini J, Regis JM, et al. (2011) Three-dimensional rotational angiography in the assessment of the angioarchitecture of brain arteriovenous malformations. J Neuroradiol. 38: 167-174.
- Lobato RD, Perez C, Rivas JJ, Cordobes F (1988) Clinical, radiological, and pathological spectrum of angiographically occult intracranial vascular malformations. Analysis of 21 cases and review of the literature. J Neurosurg. 68: 518-531.
- Srinivasan VM, Schafer S, Ghali MG, Arthur A, Duckworth EA (2016) Cone-beam CT angiography (Dyna CT) for intraoperative localization of cerebral arteriovenous malformations. J Neurointerv Surg. 8: 69-74.
- Graf CJ, Perret GE, Torner JC (1983) Bleeding from cerebral arteriovenous malformations as part of their natural history. J Neurosurg 58:331-337.
- van der Bom IMJ, Gounis MJ, Ding L, Kühn AL, Goff D, et al. Target delineation for radiosurgery of a small brain arteriovenous malformation using high-resolution contrast-enhanced cone beam CT. J NeurointervSurg 6:e34.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi