Research Article, J Clin Exp Oncol Vol: 4 Issue: 1
Early Changes in 2D-Speckle-Tracking Echocardiography May Predict a Decrease in Left Ventricular Ejection Fraction in Lymphoma Patients Undergoing Anthracycline Chemotherapy: A Pilot Study
Yali Xu1,4, Joerg Herrmann1, Patricia A Pellikka1, Stephen M. Ansell2, Stephen S Cha3 and Hector R Villarraga1*
1Division of Cardiovascular Diseases, Mayo Clinic, Rochester, Minnesota, USA
2Division of Hematology, Mayo Clinic, Rochester, Minnesota, USA
3Division of Biomedical Statistics and Informatics, Mayo Clinic, Rochester, Minnesota, USA
4Xinqiao Hospital, The Third Military Medical University, Chongqing, China
Corresponding author : Hector R Villarraga, MD
Division of Cardiovascular Diseases, Mayo Clinic, Rochester, Minnesota, USA
Tel: +507 284 9601
E-mail: villarraga.hector@mayo.edu
Received: November 27, 2014 Accepted: March 23, 2015 Published: March 30, 2015
Citation: Xu Y, Herrmann J, Pellikka PA, Ansell SM, Villarraga HR et al. (2015) Early Changes in 2D-Speckle-Tracking Echocardiography may Predict a Decrease in Left Ventricular Ejection Fraction in Lymphoma Patients Undergoing Anthracycline Chemotherapy: A Pilot Study. J Clin Exp Oncol 4:1. doi: 10.4172/2324-9110.1000134
Abstract
Background: Two-dimensional speckle-tracking echocardiography (2D-STE) may detect early changes in cardiac mechanics in patients with normal left ventricular ejection fraction (LVEF). We aimed to evaluate whether changes in strain or strain rate, as measured by 2D-STE, precede a decrease in LVEF in patients with lymphoma undergoing anthracycline-based chemotherapy (AC).
Methods: We studied patients with lymphoma who underwent 2D-STE before and after starting AC. A cardiotoxicity “event” was defined as a decrease in LVEF by ≥10% or to <50%. Standard echocardiographic and strain indices were analyzed.
Results: A total of 46 patients with lymphoma (54% men; mean (SD) age, 64 (14) years) were included. An event occurred in 12 patients after starting AC. Abnormalities were detected in global longitudinal strain (GLS), peak systolic global longitudinal strain rate (GLSRs), and global circumferential strain rate (GCSR) at <6 months and in global longitudinal early diastolic strain rate (GLSRe) at 6-12 months before a decrease in LVEF (GLS odds ratio (OR) (95% CI) 1.86 (1.28-2.91), P<0.001; global circumferential strain OR (95% CI) 1.47(1.13-1.97), P=0.005; GLSRs OR (95% CI) 1.31 (1.10-1.61), P=0.002; and GCSR OR (95% CI) 1.08 (1.00-1.19), P=0.0495).
Conclusions: GLS and GLSRs were the earliest and most predictive echocardiographic strain parameters for AC-induced cardiomyopathy in this pilot study. These parameters may be incorporated into cardiotoxicity surveillance protocols for patients undergoing AC.
Keywords: Anthracycline; Cardiotoxicity; LVEF; Lymphoma; Speckle-tracking echocardiography, 2D; Strain
Abbreviations
A: Peak Mitral Inflow Velocity at Late Diastole; AC: Anthracycline-Based Chemotherapy; AUC: Area Under the Curve; CHF: Congestive Heart Failure; 2D-STE:2D-Speckle-Tracking Echocardiography; E: Peak Mitral Inflow Velocity at Early Diastole; GCS: Global Circumferential Strain; GCSR: Global Circumferential Strain Rate; GCSRe: Global Circumferential Strain Rate at Early Diastole; GLS: Global Longitudinal Strain; GLSRe: Global Longitudinal Strain Rate at Early Diastole; GLSRs: Global Longitudinal Strain Rate at Peak Systole; GRS: Global Systolic Radial Strain; GRSR: Global Systolic Radial Strain Rate; LV:Left Ventricular; LVEF: Left Ventricular Ejection Fraction; OR:Odds Ratio; ROC: Receiver Operating Characteristic; S/SR: Strain and Strain Rate; SR: Strain Rate
Introduction
Since anthracyclines were introduced in the treatment of non- Hodgkin lymphoma in the late 1960s, they have been acknowledged as a cornerstone in the management of cancer; however, anthracyclineinduced cardiotoxicity eventually results in congestive heart failure (CHF) in 4% to 20% of recipients and is associated with a poor prognosis [1-3]. Because of this poor prognosis and because of the increasing number of long-term cancer survivors, chemotherapyinduced cardiotoxicity is increasingly recognized as an area of concern. Early changes in myocardial mechanics due to anthracycline-based chemotherapy (AC) have not been systematically studied in patients with lymphoma. In many cancer survivors the mortality risk from cardiac disease is equal to or even greater than that from a recurrent malignancy [4,5]. Early detection of AC-induced myocardial dysfunction is essential and could help to decrease the risk of CHF and improve clinical outcomes in lymphoma survivors.
Left ventricular ejection fraction (LVEF) as measured by conventional echocardiography is the most common method for monitoring left ventricular systolic function in patients undergoing chemotherapy; however, this method may not accurately identify the onset of cardiotoxicity in patients undergoing AC [6‑9]. Other limitations of this method are that it is influenced by contractility and preload/afterload effects; it relies on geometric assumptions for its calculation; and it is a measure of global function that is unable to determine regional abnormalities. 2D speckle-tracking echocardiography (2D-STE) may offer greater advantages over traditional techniques because it provides a multidimensional evaluation of myocardial mechanics from longitudinal, radial, and circumferential vectors. The aim of our study was to evaluate whether 2D-STE can detect early changes in myocardial mechanics in patients with lymphoma undergoing AC before a decrease in LVEF occurs.
Methods
Subjects
The subject group was retrospectively identified from our patient database from among all patients with Hodgkin and non- Hodgkin lymphoma that were referred to Mayo Clinic, Rochester, Minnesota, underwent AC, and had echocardiography from January 2004 to December 2010. Patients at baseline with an LVEF less than 50%, symptomatic CHF, serious arrhythmias, severe valvular heart disease, or history of cardiac surgery, as well as those without serial digital echocardiograms, were excluded. All patients had baseline echocardiography, designated T0, and follow-up echocardiography at least once after starting AC. Time frames for follow-up echocardiography were at less than 6 months (T1), within 6 to 12 months (T2), and at more than 12 months (T3) after the initiation of AC. An “event” of cardiotoxicity was defined as a decrease in LVEF by 10% or more or to less than 50% [9-11]. The study was approved by the Mayo Clinic Institutional Review Board, and consent was obtained from all participants.
Demographic data
Age, sex, body surface area, body mass index, heart rate, and blood pressure were obtained from the patients’ medical records. Medical history of hypertension, hyperlipidemia, smoking, obesity, and diabetes mellitus were recorded at baseline. Total dosage of doxorubicin and the occurrence of CHF based on Framingham criteria [12] were recorded. Major criteria include paroxysmal nocturnal dyspnea or orthopnea, neck vein distention, cardiomegaly, acute pulmonary edema, S3 gallop, and hepatojugular reflux principally; minor criteria are ankle edema, night cough, dyspnea on exertion, hepatomegaly, pleural effusion, and tachycardia. To establish a diagnosis of CHF, 2 major or 1 major and 2 minor criteria must be present.
Conventional echocardiography
Echocardiography was performed with Sequoia (Siemens Medical Solutions USA, Inc.), iE33 (Philips Medical Systems) and Vivid 7 (GE Vingmed Ultrasound AS) systems following a standard echocardiographic imaging protocol by a Registered Diagnostic Cardiac Sonographer. LVEF was measured by M-mode or 2D method using a parasternal long-axis view. End-diastolic septal thickness, end-diastolic left ventricular (LV) wall thickness, LV end-diastolic diameter, LV mass, LV mass index, and stroke volume (calculated from end-diastolic and end-systolic volumes or from the time velocity integral and LV outflow tract diameter) were measured. Left atrial volume index was measured from apical 2- and 4-chamber views. Pulsed-wave Doppler echocardiography was performed to obtain peak mitral inflow velocities at early (E) and late (A) diastole, E/A ratio, and deceleration time. Tissue Doppler echocardiography was performed with the sample volume positioned at the mitral annular junction to obtain tissue velocities (i.e., ratio of E to medial early diastolic mitral annular velocity).
LV deformation parameters by 2D-STE
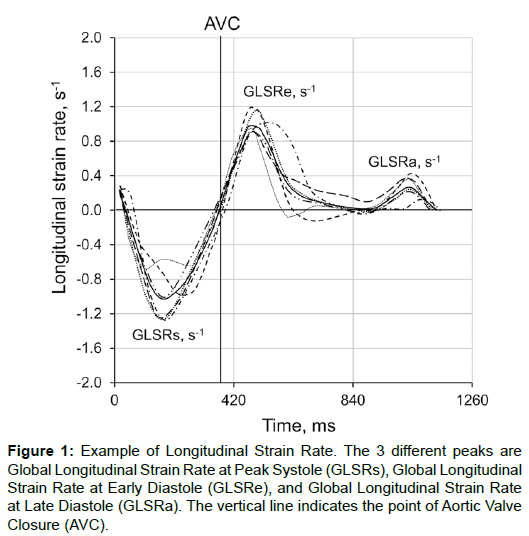
Frame rates were optimized at acquisition times between 40 and 90 frames per second. Standard 2D images of the LV in the parasternal short-axis view at midpapillary level and in the apical 4-, 2-, and 3-chamber views were acquired at baseline and follow-up and stored for offline measurement with Syngo VVI software Version 2.5 (Siemens Medical Solutions). Segmental LV myocardial strain was assessed in 16 segments (6 basal, 6 mid, and 4 apical segments) following the American Society of Echocardiography’s 16-segment model [13]. Segmental longitudinal strain at peak systole and strain rate (SR) at peak systole and early diastole were measured from 3 longitudinal views in 16 segments (Figure 1). Circumferential and radial strain and SR (S/SR) were analyzed at the mid short-axis view for 6 segments. Global S/SR was averaged from the values of 16 segments (longitudinal) and 6 segments at the papillary short-axis view (circumferential and radial). Images with persistently unacceptable tracking quality (more than 2 segments) were excluded from the final analysis. Ten patients with longitudinal, circumferential, and radial strain measurements were randomly selected for calculation of interobserver and intraobserver variability.
Figure 1: Example of Longitudinal Strain Rate. The 3 different peaks are Global Longitudinal Strain Rate at Peak Systole (GLSRs), Global Longitudinal Strain Rate at Early Diastole (GLSRe), and Global Longitudinal Strain Rate at Late Diastole (GLSRa). The vertical line indicates the point of Aortic Valve Closure (AVC).
Statistical analysis
Data were summarized with mean (SD) for continuous variables and frequency (percentage) for categorical variables. Comparisons of variables from baseline to sequential time points after AC were analyzed with one-way ANOVA. Cutpoints for strain variables were obtained using receiver operating characteristic (ROC) analysis. The intraclass or interclass correlation coefficient was calculated to quantify the interobserver and intraobserver reliability and variability. All statistical analyses were performed by JMP (Version 10.1) and SAS (Version 9.3, SAS Institute Inc) software. All P values less than 0.05 were considered statistically significant.
Results
Clinical characteristics
A total of 46 patients met all the inclusion criteria and were included in this study. Mean (SD) age of the patients was 64 (14) years (41 [89%] were older than 50 years), and 25 (54%) were men. Comorbid conditions included hypertension in 24 patients (52%), diabetes mellitus in 10 (22%), obesity (body mass index >30 kg/m2) in 26 (57%), hyperlipidemia in 29 (63%), coronary artery disease in 3 (7%), and cigarette smoking in 9 (20%). Clinical data of these patients for all time points are provided in Table 1. No significant differences were noted in body surface area, body mass index, heart rate, or blood pressure between baseline and sequential time points after AC.
| Time Pointa | |||||
|---|---|---|---|---|---|
| Parameter | T0 (n=46) | T1 (n=26) | T2 (n=21) | T3 (n=12) | P |
| BSA, m2 | 1.9 (0.2) | 1.9 (0.2) | 1.9 (0.3) | 1.9 (0.4) | 0.91 |
| BMI, kg/m2 | 28.9 (5.0) | 27.9 (5.2 ) | 26.9 (4.7) | 29.1 (7.0) | 0.73 |
| HR, beats/min | 81 (20) | 81 (29) | 80 (14) | 82 (17) | 0.77 |
| SBP, mm Hg | 123 (25) | 121 (18) | 115 (17) | 122 (18) | 0.46 |
| DBP, mm Hg | 73 (13) | 67 (10) | 68 (10) | 76 (14) | 0.09 |
Note: a Values are mean (SD) value for the group.
Table 1: Clinical Data Before and After Anthracycline Therapy.
A total of 44 patients (2 patients had missing data) had an average total dose of 573 (122) mg of AC (range, 200-810 mg). The median duration of chemotherapy was 113 days, with a mean of 130 (69) days.
Standard echocardiographic analysis
All 46 patients underwent baseline (T0) echocardiography. After starting AC, all patients had at least 1 follow-up echocardiogram, which was at T1 for 26 patients, T2 for 21 patients, and T3 for 12 patients (some patients had more than 1 follow-up echocardiogram). In the observational cohort, follow-up conventional echocardiography was performed at the discretion of the clinician. One event (2%) of a decrease in LVEF occurred at T1, 5 (11%) occurred at T2, and 6 (13%) at T3, for a total of 12 events (26%). Standard echocardiographic parameters of systolic and diastolic function before and after AC are shown in Table 2. There were no significant differences in conventional echocardiographic variables of end-diastolic values of septal thickness, LV wall thickness, and LV diameter and LV mass and mass index between T1, T2, T3, and T0. A significant decrease in LVEF (P<0.001), as well as in stroke volume (P=0.04), was seen between T3 and T0. There were no significant changes in LV diastolic function parameters.
| Time Pointa | |||||
|---|---|---|---|---|---|
| T0 (n=46) | T1 (n=26) | T2 (n=21) | T3 (n=12) | Feasibilityb | |
| 2D Echo | |||||
| EDST, mm | 10.2 (1.7) | 10.5 (1.2) | 9.8 (1.3) | 9.9 (1.5) | 105 (100) |
| EDLVWT, mm | 9.9 (1.7) | 10 (1.4) | 10.1 (1.6) | 9.6 (1.3) | 105 (100) |
| LVEDD, mm | 46 (5) | 48 (4) | 48 (5) | 47 (9) | 105 (100) |
| LVEF, % | 65 (5) | 62 (5) | 62 (7) | 55 (14)c | 105 (100) |
| LAVI, mL/m2 | 33 (13) | 42 (16) | 32 (12) | 33 (12) | 81 (77) |
| LVM, g | 163 (43) | 175 (33) | 170 (51) | 165 (68) | 105 (100) |
| LVMI, g/m2 | 86 (21) | 94 (16) | 91 (18) | 86 (22) | 105 (100) |
| SV, mL | 91 (19) | 82 (15) | 83 (20) | 75 (21)d | 103 (98) |
| Mitral Inflow Doppler | |||||
| E, cm/s | 0.8 (0.2) | 0.7 (0.2) | 0.7 (0.2) | 0.87 (0.2) | 97 (92) |
| A, cm/s | 0.8 (0.3) | 0.8 (0.2) | 0.8 (0.2) | 0.8 (0.2) | 88 (84) |
| E/A | 1.1 (0.4) | 0.9 (0.4) | 0.9 (0.3) | 0.9 (0.3) | 91 (87) |
| DT, ms | 203 (50) | 231 (42) | 208 (47) | 187 (58) | 83 (79) |
| Medial E/e′ | 10.9 (5.5) | 10.5 (4.2) | 11.3 (4.0) | 13.4 (5.7) | 95 (90) |
Note: a Values are mean (SD) value for the group.
bNo. (%) of all 105 examinations for which the data could be obtained.
cP<0.001.
dP=0.04; T1, T2, T3, vs T0.
Table 2: Standard Echocardiographic Parameters Before and After AnthracyclineTherapy.
Measurement of strain variables
Comparisons of S/SR before and after AC are shown in Table 3. In contrast to LVEF, abnormalities in global longitudinal strain (GLS) and global longitudinal strain rate at peak systole (GLSRs) were evident by 2D-STE in all 26 participants evaluated at T1 (57% of the total) and in early diastolic GLSR (GLSRe) in all 21 patients evaluated at T2 (46% of the total). There were significant differences between post-AC (T1, T2, and T3, respectively) and baseline (T0) values of GLS (P=0.02, P=0.04, P<0.001), GLSRs (P<0.001, P=0.03, P<0.001), and GLSRe (P<0.001 [T2], P<0.001 [T3]). A significant difference was noted in global circumferential strain rate (GCSR) between T1 and T0 (P=0.03), but not in other circumferential strain parameters or in global systolic radial strain (GRS) and SR (GRSR).
| Time Pointb | ||||
|---|---|---|---|---|
| T0 (n=46) | T1 (n=26) | T2 (n=21) | T3 (n=12) | |
| GLS, % | –17.5 (2.9) | –15.3 (3.2)c | –15.4 (2.8)c | –12.6 (2.8)d |
| GLSRs,s-1 | –1.1 (0.2) | –0.9 (0.2)d | –1.0 (0.2)c | –0.8 (0.2)d |
| GLSRe,s-1 | 1.0 (0.3) | 0.9 (0.2) | 0.8 (0.2)d | 0.7 (0.2)d |
| GCS, % | –21.8 (4.4) | –19.8 (4.7) | –20.2 (4.8) | –19.5 (7.3) |
| GCSR,s-1 | –1.6 (0.5) | –1.3 (0.4)c | –1.4 (0.4) | –1.3 (0.6) |
| GCSRe, s-1 | 1.5 (0.4) | 1.2 (0.3) | 1.2 (0.5) | 1.3 (0.6) |
| GRS, % | 38.1 (14.3) | 37.1 (15.5) | 37.1 (13.2) | 38.4 (11.4) |
| GRSR, % | 2.4 (1.0) | 2.0 (0.7) | 2.1 (0.7) | 2.4 (0.8) |
Note : a Feasibility of measuring strain and strain rate for echo examinations (N=105 total) was 98% (n=103) for longitudinal, 97% (n=102) for circumferential, and 97% (n=102) for radial measurements.
b Values are mean (SD) value for the group.
c P<0.05; T1, T2, T3, vs T0.
d P<0.01
Table 3: Serial Strain Variables Before and After Anthracycline Therapya.
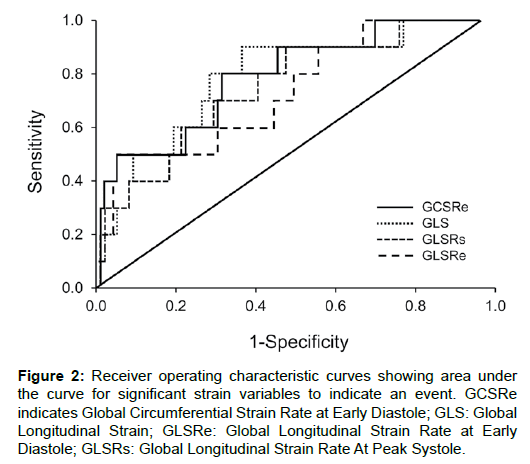
ROC analysis was performed to indicate an event of decrease in LVEF (Figure 2). The areas under the curve (AUCs) for GLS, GLSRs, GLSRe, global circumferential strain (GCS), GCSR, and global circumferential strain rate at early diastole (GCSRe) were 0.79, 0.76, 0.77, 0.70, 0.64, and 0.78, respectively,with sensitivities of 92%, 75%, 58%, 60%, 60%, and 80%, and specificities of 63%, 70%, 95%, 83%, 86%, and 67%, respectively. The most optimal cutoff values were –15.88% for GLS, −0.92 s-1 for GLSRs, 0.61 s-1 for GLSRe, –17.18% for GCS, –1.05 s-1 for GCSR, and 1.17 s-1 for GCSRe (Figure 2). A sensitivity of 80% and a specificity of 84%, with an AUC of 0.82, were obtained when a GLS of greater than –15.88% and a GCSRe of less than 1.17 s-1 were combined. The odds ratios (ORs) of detecting cardiotoxicity by a 2% difference in GLS (%) and GCS (%) were 1.86 (95% CI, 1.28-2.91) and 1.47 (95% CI, 1.13-1.97). The ORs of detecting cardiotoxicity by a 0.2 difference in GLSRs (s-1) and GCSR (s-1) were 1.31 (95% CI, 1.10-1.61) and 1.08 (95% CI, 1.00-1.19).
Figure 2: Receiver operating characteristic curves showing area under the curve for significant strain variables to indicate an event. GCSRe indicates Global Circumferential Strain Rate at Early Diastole; GLS: Global Longitudinal Strain; GLSRe: Global Longitudinal Strain Rate at Early Diastole; GLSRs: Global Longitudinal Strain Rate At Peak Systole.
Three patients met the criteria of the Framingham study [12] for symptomatic CHF after AC, all of whom had an event.Because of the small number of cases, however, statistical analysis was not possible,so they were not described and analyzed as a subgroup.
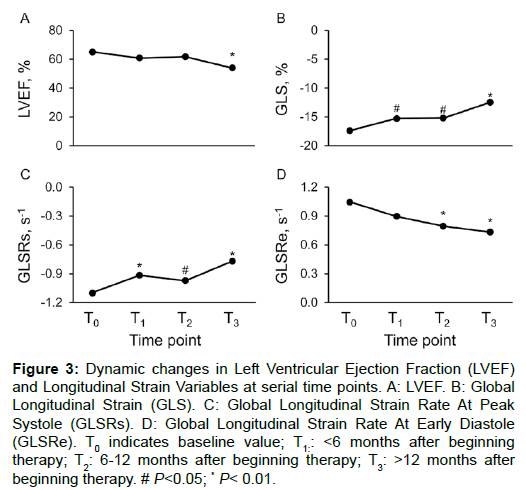
LV Dysfunction during and after AC
There were dynamic changes in LVEF and longitudinal strain parameters from baseline (T0) to subsequent follow-up times (Figure 3). LVEF decreased slightly at T1 (P>0.05), remained almost unchanged at T2, and was significantly decreased at T3compared with T0(P<0.001). A significant decrease in function was seen by GLS at T1(P=0.02), with a slight recovery at T2 (P=0.04), and an even greater decrease at T3 (P<0.001). A more significant decrease in function was also noted by GLSRs at T1 (P<0.001), with a remarkable recovery at T2 (P=0.03), and an even more prominent decrease at T3 (P<0.001). A steady decrease in GLSRe was seen without any recovery during and after AC (Figure 3).
Figure 3: Dynamic changes in Left Ventricular Ejection Fraction (LVEF) and Longitudinal Strain Variables at serial time points. A: LVEF. B: Global Longitudinal Strain (GLS). C: Global Longitudinal Strain Rate At Peak Systole (GLSRs). D: Global Longitudinal Strain Rate At Early Diastole (GLSRe). T0 indicates baseline value; T1: <6 months after beginning therapy; T2: 6-12 months after beginning therapy; T3: >12 months after beginning therapy. # P<0.05; * P< 0.01.
Interobserver and intraobserver variability
Table 4 shows the results of interobserver and intraobserver variability and reliability analysis. Longitudinal S/SR had the highest reliability and the least variability in both interobserver and intraobserver analysis.
| ICC (95% CI) | ||
|---|---|---|
| Variables | Intraobserver variability | Interobserver variability |
| GLS, % | 0.989 (0.957-0.997) | 0.943 (0.755-0.985) |
| GLSRs, s-1 | 0.922 (0.711-0.982) | 0.843 (0.392-0.962) |
| GCS, % | 0.903 (0.645-0.978) | 0.962 (0.856-0.991) |
| GCSR, s-1 | 0.862 (0.478-0.968) | 0.872 (0.452-0.966) |
| GRS, % | 0.668 (–0.436-0.911) | 0.794 (–0.211-0.925) |
| GRSR, s-1 | 0.396 (–4.079-0.687) | –0.236 (–4.765-0.644) |
Table 4: Intraobserver and Interobserver Correlation Coefficient (ICC).
Discussion
To our knowledge, this is the first study on the use of 2D-STE for the detection of AC-induced cardiotoxicity in adult patients with lymphoma. The present study shows that changes in GLS, GLSRs, and GLSRe precede a decrease in LVEF in patients soon after completion of AC; the median duration of chemotherapy in our study was 113 days, so most patients had finished AC at T1. Both longitudinal and circumferential S/SR can identify a decrease in LVEF by 10% or to less than 50%. Longitudinal S/SR is a better indicator than circumferential strain for the detection of AC-induced cardiotoxicity. Both longitudinal and circumferential SR at early diastole is potentially valuable in the detection of AC-induced myocardial dysfunction.
Anthracyclines remain one of the most effective drug classes in cancer therapy and yet one of the most cardiotoxic. Up to 20% of patients may have development of CHF in the decades that follow curative therapy, and some additional patients will have clinically asymptomatic cardiomyopathy [14,15]. It has been demonstrated that institution of heart failure therapy within the first 6 months of onset of cardiomyopathy is crucial for recovery of systolic function. This very fact provides a strong impetus for early detection of changes in LV mechanical function in patients undergoing potentially cardiotoxic chemotherapy, such as those with lymphoma. Current standard modes of monitoring, however, rely on clinical symptoms more than anything else, and knowledge regarding the best surveillance strategies for cancer patients receiving anthracyclines remains limited. 2D-STE has emerged as an imaging technique that could potentially revolutionize post chemotherapy modes of surveillance.
Changes in strain variables after AC
Currently, resting LVEF assessed with conventional echocardiography is a key parameter used to identify and monitor AC-related myocardial dysfunction; however, change in LVEF is commonly a late finding. For this reason, other parameters of systolic and diastolic function in addition to LVEF are sought to detect asymptomatic myocardial mechanical dysfunction [16,17]. 2D-STE is an accurate, angle-independent modality that can be used to quantify LV function, and it shows to be promising in the early identification of LV abnormalities before a decrease in LVEF in patients with cancer undergoing AC. Several studies have shown that conventional echocardiography–derived S/SR was more sensitive than LVEF in the detection of AC-related LV dysfunction in breast cancer patients [6,9,11,18-21]. Poterucha et al. [6] showed that a change in LV longitudinal peak systolic strain precedes a decrease in LVEF in pediatric cancer patients 4 and 8 months after AC and concluded that strain imaging was more sensitive in the monitoring of cardiotoxicity. Stoodley et al. [11] found that a decrease in LV systolic strain was detected before a change in LVEF 1 week after completion of AC for breast cancer. Our results show that abnormalities could be detected at T1 (within 6 months of starting AC) by GLS and GLSRs in 26 participants (100% of those tested; 57% of the total) and by GLSRe at T2 (6-12 months after starting AC) in 21 patients (100% of those tested; 46% of the total) before a remarkable decrease in LVEF occurred. This study thereby confirms that longitudinal strain variables indicate subtle myocardial changes and precede a noticeable decrease in LVEF in adult patients with lymphoma after AC.
Changes in diastolic SR after AC
More than 50% of patients with heart failure have normal diastolic function when measured with traditional methods. Because myocardial lengthening is associated with the onset of mitral inflow into the LV, changes in global SR may be an early marker of global diastolic function [22]. Early diastolic SR is shown to be useful in identifying abnormalities in the early diastolic phase [23] but is not well studied in AC-induced cardiotoxicity. Our study found that abnormalities were noted in GLSRe at T2 and T3, and GCSRe was a good parameter to indicate a decrease in LVEF. However, no statistical differences were present in traditional diastolic variables of left atrial volume index, deceleration time, E/A ratio, and ratio of E to medial early diastolic mitral annular velocity between baseline and serial echocardiograms after AC. Based on these results, we can conclude that changes in GLSRe precede traditional parameters in the detection of diastolic dysfunction in patients with lymphoma who underwent AC. GCSRe was also indicative of AC-induced diastolic dysfunction. Both GLSRe and GCSRe were potentially valuable in the detection of AC-induced LV diastolic dysfunction, whereas traditional echocardiographic variables were not affected by AC (Table 2).
S/SR vs.circumferential strain after AC
Historically,LV dysfunction has been defined by serial changes in LVEF, and a decrease in LVEF by a certain degree has been considered a safety end point. International oncologic guidelines define cardiotoxicity as an absolute decrease in LVEF by 10 percent units, associated with a decrease below its normal limit of 50% [24]. In our study, the event (a decrease in LVEF by ≥10% or to <50%) occurrence rate was 1 (2%) at T1, 5 (11%) at T2, and 6 (13%) at T3, for a total of 12 (26%) events, which is similar to an occurrence of 28% of subclinical cardiomyopathy with fractional shortening less than 25% in lymphoma patients [15]. In our study, cardiotoxicity was detected in 12 patients (26%) by both global longitudinal and circumferential S/SR, especially by longitudinal strain variables before a decrease in LVEF was seen.
Since differences of 2% by strain and 0.2 s-1 by SR are more clinically relevant and are above the levels of interobserver and intraobserver variability, we calculated the OR for both longitudinal and circumferential S/SR using these values. To detect a 2% difference in strain, the OR was higher for GLS than GCS (1.86 vs 1.47); to detect 0.2 difference in SR, the OR was higher for GLSRs than GCSR (1.31 vs 1.08). GLS was more indicative of cardiotoxicity (AUC, 0.79; sensitivity, 92%; specificity, 63%; P<0.001) than GCS (AUC, 0.70; sensitivity, 60%; specificity, 83%; P=0.003). Similarly, GLSRs (AUC, 0.76; sensitivity, 75%; specificity, 70%; P=0.001) was a better indicator than GCSR (AUC, 0.64; sensitivity, 60%; specificity, 86%; P=0.048). The cutoff by GLS (−15.88%) to detect AC cardiotoxicity is close to that of Wang et al. [25], who found a cutoff of–16% in GLS with a high sensitivity (95%) and specificity (95%) to indicate LV diastolic dysfunction. When a GLS of greater than −15.88% and GCSRe of less than 1.17 s-1 were combined to detect an event, a higher AUC of 0.82 with a sensitivity of 80% and a specificity of 84% was obtained, which is more meaningful in the identification of cardiotoxicity.
No significant differences were detected, however, in radial S/ SR after receiving AC in our cohort study. Ho et al. [19] also did not find diagnostic value in 2D radial strain for the detection of AC cardiotoxicity. In contrast, Sawaya et al. [7] and Stoodley et al. [11] both reported significant decreases in radial strain, as well as in longitudinal strain, after AC, probably due to different follow-up time (Sawaya et al. [7] at 3 months and Stoodley et al. [11] at 1 week), different software (both Sawaya et al. and Stoodley et al. [7,11] used Echo-Pac, GE Healthcare), and a relatively great variability in radial S/SR. The merit of radial strain variables for the detection of ACinduced myocardial injury requires further studies.
Mechanism of changes in LV dysfunction
Dynamic changes in LVEF and longitudinal strain parameters were detected between baseline (T0) and subsequent follow-up times. On the basis of the present study, a significant decrease in GLS (P=0.02) and more prominent decrease in GLSRs (P<0.001) was shown at T1, followed by a slight increase by GLS (P=0.04) and a prominent recovery by GLSRs at T2(P=0.03). The lowest levels of both GLS and GLSRs occurred at T3. The dynamic trend indicated that GLSRs probably was more sensitive than GLS in the detection of AC-induced cardiotoxicity.
There is a close relationship between early structural damage and later sequential changes in myocardial mechanics manifested as cardiac dysfunction [26]. The potential cause of the dynamic changes in these parameters may be related to the duration of chemotherapy in this cohort, mean 130 (69) days, which meant that most patients with lymphoma had completed chemotherapy at T1, and it is a great threat to the cardiovascular system when anthracyclines reach the peak cumulative dose at that time. An important mechanism of AC cardiotoxicity is that the anthracycline can form a complex with iron, which catalyzes free-radical production and leads to membrane disruption, widespread cellular dysfunction, and cell death [27] and consequently causes mechanical changes in the contractility of the myocardium. A recovery, with an improvement of GLS and GLSRs, was shown at T2 because most of the lymphoma patients had finished AC at that time, the cardiac system was no longer exposed to AC directly, and a self-recovery mechanism was probably initiated. A similar trend was detected in systolic strain by Poterucha et al. [6], who revealed that segmental motion of longitudinal peak systolic strain was decreased at 4 months and recovered at 8 months. Interestingly, the present study showed a steady decrease in GLSRe, which has a different trend compared with longitudinal systolic S/SR after starting AC, so we presume that diastolic SR is less affected by direct exposure to AC than systolic S/SR and hard to recover by dosage control in these patients.
Limitations
Limitations of the study include that this was a pilot and retrospective study. The sample size was small, the follow-up time was not very long, and close monitoring very early (1 and 3 months) after starting AC was not included. Some of the patients’ echocardiograms were missing during the follow-up after receiving AC. Biomarkers such as NT-pro-BNP and cardiac troponin were not measured in the present study. Only 3 patients had CHF after chemotherapy, so analysis was not feasible due to the small number. A larger prospective cohort with longer and closer follow-up should be sought.
Conclusions
Myocardial mechanical parameters assessed with 2D-STE are more sensitive than LVEF and conventional diastolic echocardiographic variables for identifying the development of LV dysfunction in patients with lymphoma who undergo AC and can indicate the occurrence of cardiotoxicity defined as a decrease in LVEF by 10% or more or to less than 50%. 2D-based strain imaging appears to be a promising tool to identify abnormalities in global myocardial impairment during and after AC.
Acknowledgement
This publication [or project] was supported by Grant Number UL1 TR002377 from the National Center for Advancing Translational Sciences (NCATS). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
References
- Cardinale D, Colombo A, Lamantia G, Colombo N, Civelli M, De Giacomi G, et al. (2010) Anthracycline-induced cardiomyopathy: clinical relevance and response to pharmacologic therapy. J Am Coll Cardiol 55: 213-220.
- Yeh ET, Tong AT, Lenihan DJ, Yusuf SW, Swafford J, et al. (2004) Cardiovascular complications of cancer therapy: diagnosis, pathogenesis, and management. Circulation 109: 3122-3131.
- Felker GM, Thompson RE, Hare JM, Hruban RH, Clemetson DE, et al. (2000) Underlying causes and long-term survival in patients with initially unexplained cardiomyopathy. N Engl J Med 342: 1077-1084.
- Hanrahan EO, Gonzalez-Angulo AM, Giordano SH, Rouzier R, Broglio KR, et al. (2007) Overall survival and cause-specific mortality of patients with stage T1a, bN0M0 breast carcinoma. J Clin Oncol 25: 4952-4960.
- Schultz PN, Beck ML, Stava C, Vassilopoulou-Selli R (2003) Health profiles in 5836 long-term cancer survivors. Int J Cancer 104: 488-495.
- Poterucha JT, Kutty S, Lindquist RK, Li L, Eidem BW, et al. (2012) Changes in left ventricular longitudinal strain with anthracycline chemotherapy in adolescents precede subsequent decreased left ventricular ejection fraction. J Am Soc Echocardiogr 25: 733-740.
- Sawaya H, Sebag IA, Plana JC, Januzzi JL, Ky B, et al. (2012) Assessment of echocardiography and biomarkers for the extended prediction of cardiotoxicity in patients treated with anthracyclines, taxanes, and trastuzumab. Circ Cardiovasc Imaging 5: 596-603.
- Eidem BW (2008) Identification of anthracycline cardiotoxicity: left ventricular ejection fraction is not enough. J Am Soc Echocardiogr 21: 1290-1292.
- Villarraga HR, Herrmann J, Nkomo VT (2014) Cardio-oncology: role of echocardiography. Prog Cardiovasc Dis 57: 10-18.
- Perez EA, Suman VJ, Davidson NE, Kaufman PA, Martino S, et al. (2004) Effect of doxorubicin plus cyclophosphamide on left ventricular ejection fraction in patients with breast cancer in the North Central Cancer Treatment Group N9831 Intergroup Adjuvant Trial. J Clin Oncol 22: 3700-3704.
- Stoodley PW, Richards DA, Hui R, Boyd A, Harnett PR, et al. (2011) Two-dimensional myocardial strain imaging detects changes in left ventricular systolic function immediately after anthracycline chemotherapy. Eur J Echocardiogr 945-952.
- McKee PA, Castelli WP, McNamara PM, Kannel WB (1971) The natural history of congestive heart failure: the Framingham study. N Engl J Med 285: 1441-1446.
- Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, et al. (2005) Chamber Quantification Writing Group; American Society of Echocardiography’s Guidelines and Standards Committee; European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 1440-1463.
- Steinherz LJ, Steinherz PG, Tan CT, Heller G, Murphy ML (1991) Cardiac toxicity 4 to 20 years after completing anthracycline therapy. JAMA 266: 1672-1677.
- Hequet O, Le QH, Moullet I, Pauli E, Salles G, et al. (2004) Subclinical late cardiomyopathy after doxorubicin therapy for lymphoma in adults. J Clin Oncol 22: 1864-1871.
- Wells QS, Lenihan DJ (2010) Reversibility of left ventricular dysfunction resulting from chemotherapy: can this be expected? Prog Cardiovasc Dis 53: 140-148.
- Saini J, Rich MW, Lyss AP (1987) Reversibility of severe left ventricular dysfunction due to doxorubicin cardiotoxicity: report of three cases. Ann Intern Med 106: 814-816.
- Migrino RQ, Aggarwal D, Konorev E, Brahmbhatt T, Bright M, et al. (2007) Early detection of doxorubicin cardiomyopathy using two-dimensional strain echocardiography. Ultrasound Med Biol 34(2):208-214.
- Ho E, Brown A, Barrett P, Morgan RB, King G, et al. (2010) Subclinical anthracycline- and trastuzumab-induced cardiotoxicity in the long-term follow-up of asymptomatic breast cancer survivors: a speckle tracking echocardiographic study. Heart 96: 701-707.
- Plana JC, Galderisi M, Barac A, Ewer MS, Ky B, Scherrer-Crosbie M, et al. (2014) Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 27: 911-939.
- Herrmann J, Lerman A, Sandhu NP, Villarraga HR, Mulvagh SL, et al. (2014) Evaluation and management of patients with heart disease and cancer: cardio-oncology. Mayo Clin Proc 89: 1287-1306.
- Perry R, De Pasquale CG, Chew DP, Joseph MX (2008) Assessment of early diastolic left ventricular function by two-dimensional echocardiographic speckle tracking. Eur J Echocardiogr 9: 791-795.
- Stoylen A, Slordahl S, Skjelvan GK, Heimdal A, Skjaerpe T, et al. (2001) Strain rate imaging in normal and reduced diastolic function: comparison with pulsed Doppler tissue imaging of the mitral annulus. J Am Soc Echocardiogr 14: 264-274.
- Cardinale D, Colombo A, Sandri MT, Lamantia G, Colombo N, et al. (2006) Prevention of high-dose chemotherapy-induced cardiotoxicity in high-risk patients by angiotensin-converting enzyme inhibition. Circulation 114: 2474-2481.
- Wang J, Khoury DS, Yue Y, Torre-Amione G, Nagueh SF, et al. (2008) Preserved left ventricular twist and circumferential deformation, but depressed longitudinal and radial deformation in patients with diastolic heart failure. Eur Heart J 29: 1283-1289.
- Ewer MS, Ewer SM (2010) Cardiotoxicity of anticancer treatments: what the cardiologist needs to know. Nat Rev Cardiol 7: 564-575.
- Kang YJ, Chen Y, Epstein PN (1996) Suppression of doxorubicin cardiotoxicity by overexpression of catalase in the heart of transgenic mice. J Biol Chem 271: 12610-12616.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi