Case Report, J Clin Image Case Rep Vol: 5 Issue: 10
ECG Lead Reversal- is it Anterior or Inferior Wall Myocardial Infarction?
Mayank Yadav*
Department of Advanced Cardiac Center, PGIMER, Sector 12 Chandigarh, India
*Corresponding Author: Mayank Yadav
Department of Advanced Cardiac Center, PGIMER, sector 12 Chandigarh, India, 160012
E-mail: mayank001.my@gmail.com
Received: September 29, 2021 Accepted: October 14, 2021 Published: October 21, 2021
Citation: Yadav M (2021) ECG Lead Reversal- is it Anterior or Inferior Wall Myocardial Infarction?. J Clin Image Case Re 5(10): 184.
Keywords: Electrocardiogram, Myocardial Infarction
Introduction
Electrocardiogram (ECG) is an inexpensive, easily available tool for the diagnosis of a number of cardiac and noncardiac conditions in emergency as well as in nonemergency settings. It is integral part of the modern medicine for initial evaluation of patient presenting with cardiac complaints. So, it is very important to record ECG properly to ensure accurate diagnosis and appropriate treatment. ECG recorded with incorrect electrode placement can mimic as myocardial ischemia or rhythm disturbances [1]. Erroneous interpretation of inaccurately recorded ECG can result in delivering of wrong treatment to the patients. Incidence of improperly recoded ECG ranges from 0.4-4% in different clinical scenario [2]. So, physicians must be aware of these changes occur due to misplacements of ECG electrodes to ensure proper diagnosis and treatment.
Clinical Record
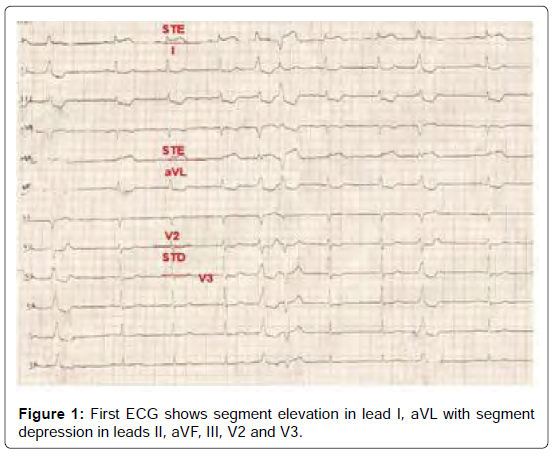
An 83-year-old male presented to emergency department with complain of chest pain for 3 hours. Chest pain was more toward left side of chest associated with excessive sweating and 3 to 4 episodes of vomiting. Patient was a known hypertensive without known previous cardiac conditions. Patient first went to near by hospital from there he was referred to our center with ECG (Figure 1).
At presentation patient was hemodynamically stable with heart rate of 60/min and blood pressure 138/78 mmHg. first 12 lead ECG (Figure 1) done in another center shows normal sinus rhythm with ST segment elevation(>1mm) in lead I and aVL with reciprocal ST segment depression and T wave inversion in leads II, III, aVF and subtle ST segment depression in lead V2, V3. There are few premature ventricle beats are present in between.
So, when patient arrived to emergency department with ECG diagnosis of acute coronary syndrome myocardial infarction of high lateral wall was made due to block in first diagonal branch of left anterior descending artery (LAD) [3].
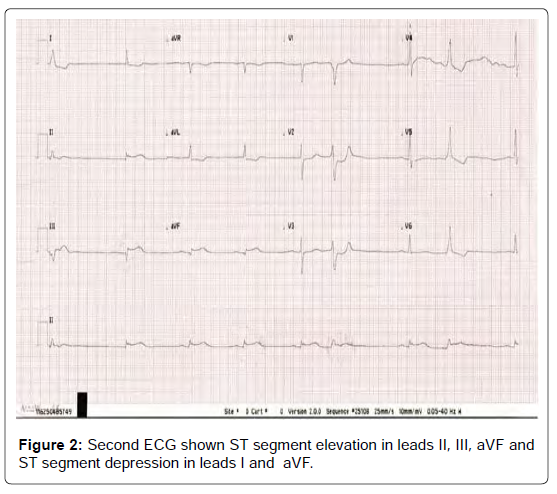
ECG was repeated (Figure 2) upon arrival in our hospital. ECG findings were different from first ECG. Second ECG shows sinus bradycardia with ST segment elevation in leads II, aVF, III (III>II) with few premature ventricular complexes. So, second ECG suggestive of inferior myocardial infarction due to blockage of right coronary artery. So, these two ECG shows myocardial infarction in 2 different territories.
Discussion
This difference in two ECG occurred due to misplacement of leads while recording the first ECG (Figure 1). On comparing both the ECG it is clear that it is due to reversal of limb lead of left arm (LA) and left leg (LL).
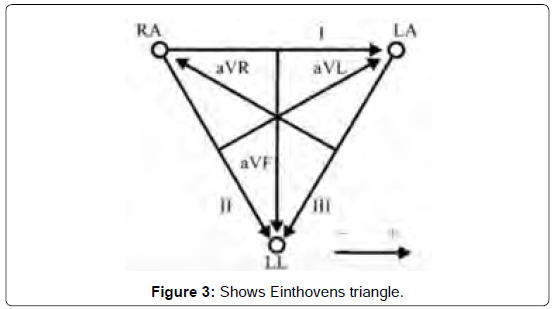
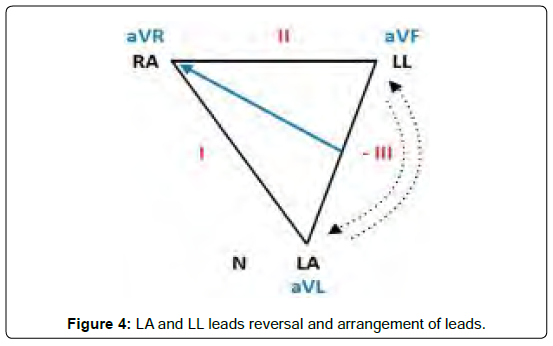
It can be better understood with the help of Einthoven’s triangle (Figure 3) and triangle with reversal of LA and LL leads. Misplacing the left arm (LA) lead with left leg (LL) lead causes reversal of Einthoven’s triangle rotating around the aVR axis (Figure 4) [4]. This results in following changes.
• Lead III becomes inverted.
• Leads I and II switch places.
• Leads aVL and aVF switch places.
• Lead aVR remains unchanged.
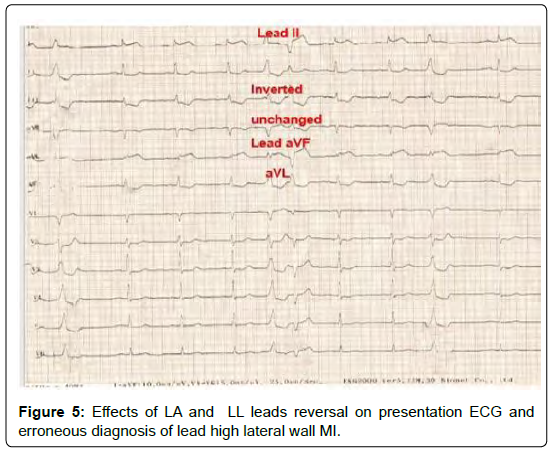
Comparing first ECG (Figure 1) with second ECG (Figure 2), Lead aVR remains unchanged (Figure 5), lead I is now representing lead II and vice versa (ST elevation in I), lead aVL now representing lead aVF and vice versa (ST elevation in aVL), Lead III is inverted showing ST depression. So, after confirming diagnosis of inferior wall myocardial infarction with probable posterior wall infarction, patient was treated with thrombolytics and anticoagulants. Post thrombolysis ECG was repeated showing resolution of ST elevation in inferior leads (Figure 6). After successful thrombolysis patient was chest pain free and put on optimal medical treatment.
Conclusion
It is concluded that patient was having inferior wall myocardial infarction with possible posterior wall infarction but due to misplacement of LA lead with LL lead ECG was giving false appearance of high lateral wall myocardial infarction due to first diagonal D1. However, treatment plan is similar in both the types myocardial infarction in most part but they have different mechanism and approach for treatment of hypotension and in terms of prognosis. So, it is important for physicians to interpretate the ECG with context of history and clinical examination and must know the abnormal ECG findings occur due to common ECG leads placement errors.
References
- Baranchuk A, Shaw C, Alanazi H, Campbell D, Bally K, et al. (2009) Electrocardiography pitfalls and artifacts: the 10 commandments. Crit Care Nurse 29(1): 67–73.
- Batchvarov VN, Malik M, Camm AJ (2007) Incorrect electrode cable connection during electrocardiographic recording. Europace 9(11): 1081–90.
- Elsayed YMH (2019) High Lateral Myocardial Infarction; the Smallest but the Most Painful Infarction – A Case Report. Asclepius Med Res Reviews 2(2): 4.
- Rosen A, Koppikar S, Shaw C, Baranchuk A (2014) Common ECG Lead Placement Errors. Part I: Limb lead Reversals. Int J Med Stud 2(3): 92–8.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi