Research Article, J Physiother Rehabil Vol: 1 Issue: 1
Effect of Pelvic Floor Muscle Training on the Quality of Life and Sexual Dysfunction in Stress Incontinence Women
Najwa Alfarra* and Waleed Altawee
Department of Physical Therapy Faisal specialist hospital and research center, Riyadh, Saudi Arabia
*Corresponding Author : Najwa Alfarra
Department of Physical Therapy, Faisal Specialist Hospital and Research center, Riyadh 11211, Saudi Arabia
Tel: 966504441988
E-mail: mohm@hotmail.com
Received: October 09, 2017 Accepted: October 30, 2017 Published: November 03, 2017
Citation: Alfarra N, Altawee W (2017) Effect of Pelvic Floor Muscle Training on the Quality of Life and Sexual Dysfunction in Stress Incontinence Women. J Physiother Rehabil 1:1.
Abstract
Introduction: Urinary incontinence is defined by the International Continence Society (ICS) as the complain of any involuntary leakage of urine. The most common type of urinary incontinence in women is stress urinary incontinence (SUI), defined as the complaint of involuntary leakage on effort or when the body engages in physical motions like running, coughing, heavy lifting or sneezing exertion. This problem is common among women and when it happens in public, it can be very embarrassing and demoralizing. Most women with urinary incontinence have limitations in participating in social activities such as sports and even working in conditions that demand too much energy and most of them complained of various forms of sexual dysfunction. Pelvic floor muscle training is defined as the ability to perform a correct contraction, meaning a squeeze around vaginal openings and an inward movement of the pelvic floor.
Objective: The objective of the study was to evaluate the impact of the pelvic floor muscle training on the quality of life and sexual dysfunction in stress incontinence women.
Methods: Twenty women complaining of stress urinary incontinence were evaluated by voiding diary, muscle power (oxford scale), UDI- 6 Questionnaires and with FSFI before and after 6 months of the exercises. All had an urogynecologic evaluation and urodynamic study.
Main outcome measures: In the voiding diary the women reported the urinary frequency, and episodes of urgency and urine leakage. The domain scores of the FSFI, including desire, arousal, lubrication, orgasm, satisfaction, and pain, were calculated together with domain scores of UDI-6 questionnaires. The supervised Pelvic Floor Muscle Training (PFMT) was conducted for 15-30 min. twice a week for 2 months, once/week for another month (total of three months were supervised PFM), and follow up once/month for another three months to review and check the compliance with the exercises. (Total treatment 6 months since the patient started their treatment until the last session).
Results: After the six months of PFMT only three out of twenty patients were completely cured, eight complain of leakage with strong sneezing, if the bladder is full, three had leakage with strong coughing and six had leakage with coughing and sneezing. One of the twenty patients had pain with intercourse VAS 2/10 and one decreased interest in intercourse.
Keywords: Musculature strength; Pelvic floor exercises; Urinary incontinence; Stress incontinence; Female sexual dysfunction
Introduction
The prevalence of urinary incontinence in women is about 20% and increases to 35% among women more than 60 years old [1-8]. The urinary incontinence does not pose a direct risk to the individuals who are affected; it affects the quality of their life in a variety of aspects [2]. These aspects include physical, social, sexual, and psychological aspects. According to the U.S department of Health and Social Services Clinical Guidelines Panel, “the initial treatment of urinary incontinence should not to be very invasive, with few side-effects and avoiding future approaches” [9]. Several conservative treatment options are available for the management of UI, such as physical therapies, behavioral modifications, and pharmaceutical interventions. Among physical therapies, pelvic floor muscles exercises are the mainstays of the conservative treatment and prevention of UI. Recently, there are a lot of publications that indicate an improvement in the quality of life on the women who undergo conservative treatment and use the PFMT [10,11].
Methods
This is a prospective study done in a primary care setting within a tertiary referral hospital. The prospective cohort study was meant to assess 20 women, who were aged 20-55 years old with sexual dysfunction in stress incontinence confirmed by patient history and urodynamic study. The participants included married, non-pregnant, with grade 1-2 cystocele or rectocele or both, stress incontinence confirmed by urodynamic and individual women who had not undergone any major pelvic floor or post-delivery surgical procedures within the past 6 months to the instigation of the study. Those excluded were women with neuromuscular diseases, cardiac pacemaker, urinary tract infection, and genitourinary surgery during the previous 6 months, and patients under medication for urinary incontinence in the past two months those using hormone replacement therapies and additionally women with prolapse stage III and IV. The study took exactly 6 months.
All patients had physical therapy evaluation, which included history, physical examination, PFM strength examined by PFX2 which also measured the force and duration of each contraction. The registered muscle strength was graded by the modified Oxford Grading Scale by La-cock: grades 0-1 if patients were not able to contract their PFMS; grade 2 if patients performed only an insufficient contraction; and grades 3-4 if patients were able to contract their PFMs properly. All muscles of the pelvic floor were investigated. Therapeutic exercises were performed for 15-30 minutes, The supervised Pelvic Floor Muscle Training (PFMT) was conducted for 15-30 min. twice a week for 2 months, once/week for another month (total of three months were supervised PFMT), and follow up once/month for another three months to review and check their compliance with the exercises total of 15 sessions over six months.
Proper methods were used to teach the patients the proper PFM contraction such as: first one, clinical observation; observation of a correct PFM contraction as squeeze around the urethral, vaginal, and anal openings and an inward lift that could be observed at the perineum. Second, vaginal palpation: this technique was described by Kegel as a method to evaluate PFM function .By placing one finger in the distal one third of the vagina and asked the woman to lift inward and squeeze around the finger. Kegel did not use this method to measure PFM strength. He used vaginal palpation to teach women how to contract their PFM and classified the contraction qualitatively as correct or not correct [12].
Main outcome measures
The subjective outcomes: The voiding diary recorded the urinary frequency, episodes of urine leakage; number of pads per day, this diary was completed at the beginning and at the end of the treatment. All the women completed the Female Sexual Function Index (FSFI) Arabic validate version by Anis [13] and Urogenital Distress Inventory (UDI-6) Arabic validated version by Waleed [18]. These questions were answered by the patients before commencing the treatment and after six months of completing the treatment, and each domain score, including desire, arousal, lubrication, orgasm, satisfaction, pain, and the quality of life was calculated.
Objective outcomes: The pelvic floor muscles strength were measured by PFX2 which also measured the duration of each contraction, and urodynamic evaluation was done in a standardized way.
Results
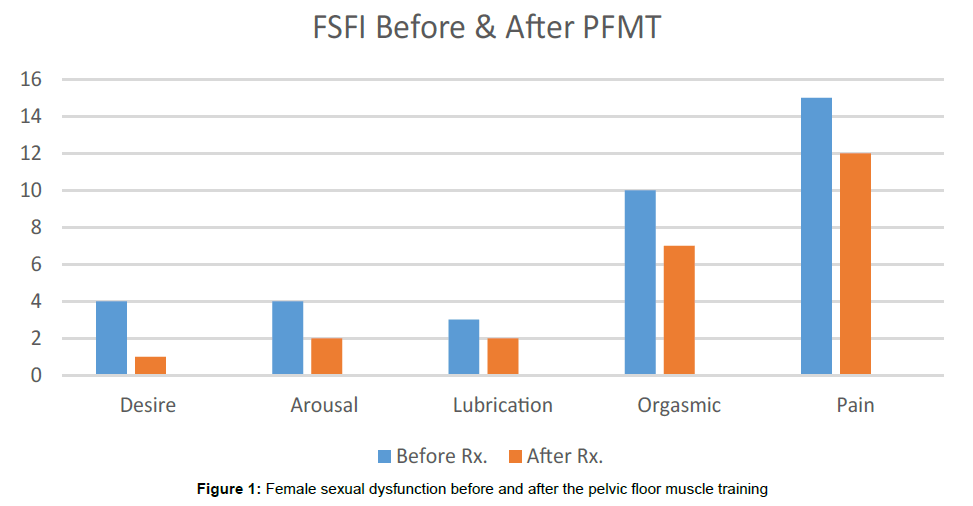
Results of the FSFI questionnaire showed that 10 (50%) of the women had female sexual dysfunction. We identified four sexual disorders: of desire, of arousal, of orgasm, and of sexual pain as proposed in the classification of the International Consensus Conference of Female Sexual Dysfunction [14]. Sexual pain disorder was diagnosed in fifteen women (75%), hypoactive sexual desire disorder in four (20%), four women had sexual arousal disorder (20%), three women had difficulty to maintain lubrication during the intercourse ((15%), and orgasmic phase disorder in ten (50%). The quality of life UDI-6 questionnaire showed 17 (85%) of the women had SUI, while 3 of them cured. After six months of PFMT a comparison of the voiding diary completed before and after treatment showed a minor changes reduction in the number of total voids, number of leakage episodes, and pads used per day (Tables 1 and 2). The bladder volume during cough test was measured at three levels 200 ml, 250 ml, and 300 ml, followed (Young, 19). The cough test was positive before the treatment in the twenty women at two levels 250 ml and 300 ml while after the treatment the cough test was positive on 17 women (85%) at the same levels 250 ml. and 300 ml. Three women were cured from the SUI. Muscle power of the PFM was measured before and after the treatment (Table 3). The FSFI and UDI- 6 questionnaires completed before and after the treatment showed improvement only in three women. It is evident that Pelvic Floor Muscle Training does not have much effect on improving the quality of life on women with stress incontinence and sexual dysfunction. After the training, most of the women still experienced involuntary urination especially when they had a strong cough, sneezing, while laughing, and while carrying heavy things. However, improvement was only realized on three patients who had experienced the problem during sexual intercourse. For instance in case number 3, 4 & 7 they do not seem to complain about incontinence during sexual intercourse or with coughing, the pain during intercourse completely resolved, the sexual desire improved, the arousal with the lubrication improved, and the orgasmic improved as it shown in Figure 1. It also seemed to work on patient case number 3 who had a vaginal muscle spasm and kidney transparent where she reported that the leakage had drastically stopped.
| Case # | Complain | No. of pads/day | Cystocele/Rectocele | Frequency of voiding | # of parity | Pat. age |
|---|---|---|---|---|---|---|
| Case 1 | leakage with sneezing, coughing and laughing, urgency | no | Cystocele grade 2 | 15/day | 4 | 55yrs. |
| Case 2 | leakage with sneezing and 4/10 pain scale with intercourse vaginal muscle spasm | no | Cystocele grade 2 | 12/day | 2 | 35yrs. |
| Case 3 | kidney transplant Leakage with coughing Leakage with intercourse, Pain with intercourse 3/10 | 2/day | None | 12/day | 10 | 48yrs. |
| Case 4 | leakage with coughing and sneezing, sometimes with intercourse, pain with intercourse 2/10 | no | None | 12/day | 3 | 47yrs. |
| Case 5 | leakage with coughing and sneezing, pain with intercourse 2/ 10 | no | None | 10/day | 3 | 37 yrs. |
| Case 6 | leakage with laughing, coughing and sneezing, pain with intercourse 5/10 | no | None | 14/day | 0 | 50 yrs. |
| Case 7 | leakage with coughing and sneezing, pain with intercourse 3/10 | no | None | 12/day | 3 | 55yrs. |
| Case 8 | leakage of coughing Sneezing and laughing, Urgency, decrease interest in intercourse, pain with intercourse 1/10 |
no | None | 11/day | 4 | 55yrs. |
| Case 9 | leakage with coughing and sneezing, pain with intercourse 2/10 | no | None | 10/day | 3 | 54yrs. |
| Case 10 | leakage with laughing and sneezing, pain with intercourse 4/10 | no | None | 11/day | 4 | 55yrs. |
| Case 11 | leakage with coughing and sneezing, urgency, pain with intercourse 5/10 |
no | None | 16/day | 2 | 43 yrs. |
| Case 12 | leakage with sneezing, coughing and when carrying heavy object pain with intercourse 1/10 | no | Cystocele | 12/day | 10 | 48 yrs. |
| Case 13 | Leakage with sneezing and aerobic exercise, pain with intercourse 2/10 | no | None | 12/day | 2 | 41 yrs. |
| Case 14 | Leakage with coughing, sneezing and pain with intercourse 3/10 | 3/day | Rectocele and cystocele grade 2 | 12/day | 2 | 55 yrs. |
| Case 15 | Leakage with coughing and Sneezing, pain with Intercourse 1/10 | no | None | 13/day | 4 | 53yrs. |
| Case 16 | Leakage with coughing and Sneezing, pain with Intercourse 4/10 | no | None | 10/day | 3 | 55yrs. |
| Case 17 | Leakage with strong sneezing | 9/day | None | 9/day | 3 | 35 yrs. |
| Case 18 | Minor leakage with coughing | no | Rectocele and cystocele grade 2 | 10/day | 0 | 55 yrs. |
| Case 19 | Leakage with coughing, sneezing | 3/day | Rectocele and cystocele grade 2 | 12/day | 7 | 55 yrs. |
| Case 20 | Leakage during coughing, sneezing | no | None | 14/day | 4 | 41 yrs. |
Table 1: Patient assessment before the treatment.
| Case # | Complain | No. of pads/day | Cystocele/Rectocele | Frequency of voiding | # of parity | Pat. age |
|---|---|---|---|---|---|---|
| Case 1 | leakage with sneezing only if the bladder is full | no | Cystocele grade l | 12/day | 4 | 55yrs. |
| Case 2 | leakage with sneezing and coughing and 2/10 pain scale with intercourse | no | Cystocele grade l | 11/day | 2 | 35yrs. |
| Case 3 | no leakage with coughing and sneezing no pain with intercourse | no | None | 8/day | 10 | 48yrs. |
| Case 4 | no leakage with coughing,no pain with intercourse |
no | None | 9/day | 3 | 47yrs. |
| Case 5 | leakage with strong sneezing ,pain with intercourse 2/10 | no | None | 9/day | 3 | 37 yrs. |
| Case 6 | leakage with sneezing, Pain with intercourse 4/10 | no | None | 13/day | 0 | 50 yrs. |
| Case 7 | no leakage, no pain with intercourse | no | None | 12/day | 3 | 55yrs. |
| case 8 | leakage of coughing ,Sneezing and laughing, decrease, interest in intercourse, pain with intercourse 1/10 | no | None | 11/days | 4 | 55yrs. |
| case 9 | leakage with strong coughing, Pain with intercourse 2/10 | no | none | 10/days | 3 | 54yrs. |
| Case 10 | leakage with sneezing if the bladder is full , pain with intercourse 3/10 | no | None | 11/day | 4 | 55yrs. |
| Case 11 | minimal leakage with sneezing, pain with intercourse 4/10 | no | None | 14/day | 2 | 43 yrs. |
| Case 12 | minor leakage with strong cough ,pain with intercourse 1/10 | no | None | 11/day | 10 | 48 yrs. |
| Case 13 | Leakage with sneezing , pain with Intercourse 2/10 | No | None | 11/day | 2 | 41 yrs. |
| Case 14 | Leakage with coughing, sneezing and when carry heavy object, pain with intercourse 3/10 | 3/day | Rectocele and cystocele | 12/day | 2 | 55 yrs. |
| Case 15 | Leakage with coughing and Sneezing, pain with intercourse 1/10 | No | None | 13/day | 4 | 53yrs. |
| Case 16 | Leakage with coughing and Sneezing, pain with intercourse 4/10 | No | None | 10/day | 3 | 55yrs. |
| Case 17 | Leakage with strong sneezing | No | None | 9/day | 3 | 35 yrs. |
| Case 18 | Minor leakage with coughing | No | Rectocele | 10/day | 0 | 55 yrs. |
| Case 19 | Leakage with coughing, sneezing, carry heavy thing , urgency | 3 | Rectocele and | 12/day | 7 | 55 yrs. |
| Case 20 | Leakage during laughing, sneezing, urgency | No | cystocele None | 14/day | 4 | 41 yrs. |
Table 2: Patient assessment after the treatment.
| Case # | MP. Before the treatment | MP. After the treatment |
|---|---|---|
| Case 1 | 2/5 | 2+/5 |
| Case 2 | 2/5 | 2+/5 |
| Case 3 | 2/5 | 3/5 |
| Case 4 | 2+/5 | 2+/5 |
| Case 5 | 2/5 | 3/5 |
| Case 6 | 2/5 | 2/5 |
| Case 7 | 2/5 | 3/5 |
| Case 8 | 2/5 | 2/5 |
| Case 9 | 2/5 | 2/5 |
| Case 10 | 2/5 | 2+/5 |
| Case 11 | 2-/5 | 2+/5 |
| Case 12 | 2/5 | 3/5 |
| Case 13 | 2/5 | 2+/5 |
| Case 14 | 1+/5 | 1+/5 |
| Case 15 | 2/5 | 2/5 |
| Case 16 | 2/5 | 2/5 |
| Case 17 | 2/5 | 2/5 |
| Case 18 | 2/5 | 2/5 |
| Case 19 | 1/5 | 2/5 |
| Case 20 | 2+/5 | 2+/5 |
Table 3: A comparison of the pelvic floor muscle power before and after the treatment.
Discussion
According to our results, women with stress incontinence reported a higher prevalence of female sexual dysfunction. There are several reasons for the increase in sexual dysfunction in incontinent women, such as dyspareunia resulting from urinary dermatitis. Depression and decreased libido, with a consequent reduction of interest in sexual activity, is mainly due to embarrassment and fear of urinary incontinence occurring during intercourse [15-17]. All patients treated with PFMT showed minor improvement in their urinary incontinence and sexual dysfunction. Only three of them were cured, this could be contributed to their compliance with their home exercise program and their younger age 25-35 years old. As we focused on the impact of stress incontinence on sexual life and how the resolution of urinary leakage or the improvement of urinary symptoms had a positive effect on sexual dysfunction, we can only suppose a direct beneficial effect of PFMT on sexual function only, because it acts on multiple neurological components of the pelvic floor (i.e. Sacral and pudendal nerves) [18,19]. Furthermore, we cannot actually ensure the possible impact of PFMT on sexual function independent of the improvement on stress incontinence, which can be investigated in more specific trial.
Conclusion
Urinary incontinence significantly reduces sexual function in sexually active women. Basing on the results, pelvic floor muscle training showed minor improvement in the symptoms of stress Incontinence patients. According to the Tables 1 and 2 shown above, only three women significantly improved. Therefore, counseling measures should be carried out on individual patients, such as checking their compliance with the exercise program. Furthermore, we noticed that the usage of PFMT in treating urinary symptoms in elderly women is not favorable, the patients looked for quick and easy result that does not required a lot of effort from their side.
References
- Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, et al. (2002) The standardization of terminology of lower urinary tract function: report from the standardization sub-committee of the International Continence Society. Neurourol Urodyn 21: 167-178.
- Fox N, Hunn A, Matters N (2009) National Institute for Health Research. The NIHR design service sampling and sample size calculation.
- Mørkved S, Bø K (2012) Effect of pelvic floor muscle training during pregnancy and after childbirth on prevention and treatment of urinary incontinence: a systematic review. Br J Sports Med 48.
- Kegel AH (1948) Progressive resistance exercise in the functional restoration of the perineal muscles. Am J Obstet Gynecol 56: 238-249.
- Nissenkorn I, Shalev M, Radzisewski P, Dobronski P, Borkowski A, et al. (2004) Patient-adjusted intermittent electrostimulation for treating stress and urge urinary incontinence. BJU Int 94: 105-109.
- Shaw C (2002) A systematic review of the literature on the prevalence of sexual impairment in women with urinary incontinence and the prevalence of urinary leakage during sexual activity. Eur Urol 42: 432-440.
- Maral I, Ozardes H, Peskiscioglu L, Bumin AM (2001) Prevalence of stress urinary incontinence in both sexes at or after age 15 years. A cross sectional study. J Urol 165: 408- 412.
- Temml C, Haidinger G, Scmidbauer J (2000) Urinary incontinence in both sexes: Prevalence rates and impact on quality of life and sexual life. Neurourol Urodyn 19: 259-71.
- U.S Department of Health and Human and Human Services. Urinary incontinence in adults. Acute and chronic management. Guidelines Report. Publication no. 96-0682.1996.
- Bø K, Talseth T, Vinsnes A (2000) Randomized controlled trial on the effect of pelvic floor muscle training on quality of life and sexual problems in genuine stress incontinent women. Acta Obstet Gynecol Scand 79: 598-603.
- Zahariou A, Karamouti M, Papaioannou P, Panagiotacopoulos V (2007) 733The effect of pelvic floor muscle training on sexual life of women with urinary incontinence. Eur Urol Suppl 6: 206.
- Mørkved S, Bø K (2013) Effect of pelvic floor muscle training during pregnancy and after childbirth on prevention and treatment of urinary incontinence: a systematic review. Br J Sports Med 48.
- Anis TH, Gheit SA, Saied HS. Alkherbas SA (2011) Arabic translation of female sexual dysfunction index validation in an Egyption population. J Sex Med 8: 3370-3378.
- Yamanishi T, Yasuda K, Sakaibara R, Hattori T, Suda S (2000) Randomized double study of electrical stimulation for urinary incontinence due to detrusor over activity. Urology 55: 353-357.
- Giuseppe PG, Pace G, Vicentini C (2007) Sexual function in women with urinary incontinence treated by pelvic floor transvaginal electrical stimulation. J Sex Med 4: 702-707.
- Chiverton PA, Wells TJ, Brink CA, Mayer R (1996) Psychological factors associated with urinary incontinence. Clin Nurse Spec 10: 229-233.
- Hannestad YS, Rortveit G, Sandvik H, Hunskaar S (2000) A community-based epidemiological survey of female urinary incontinence: The Norwegian EPICONT Study. J Clin Epidemiol 53: 1150-1157.
- Altaweel W, Seyam R, Mokhtar A, Kumar P, Hanash K (2009) Arabic version of the short form of Urogeital Distress Inventory (UDI-6) Questionnaier. Neurol Urodyn 28: 330-334.
- Seo YH, Kim SO, Song YH, Kwon D (2016) Leak point pressure at different bladder volumes in stress urinary incontinence in women: Comparison between Valsalva and cough-induced leak point pressure. Can Urol Assoc J 10: 1-2.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi