Review Article, J Physiother Rehab Vol: 6 Issue: 5
Effectiveness of Physiotherapy Interventions in the Management of Impotence: A Systematic Review
Caleb Ademola Omuwa Gbiri* and Akumabor Joy Chukwumhua
Department of Physiotherapy, College of Medicine, University of Lagos, Lagos, Nigeria
*Corresponding Author: Mitera Caleb Ademola Omuwa Gbiri, Department of Physiotherapy, College of Medicine, University of Lagos, Lagos, Nigeria, Tel: +234803359802; E-mail: cgbiri@unilag.edu.ng
Received date: 24 March, 2022, Manuscript No. JPTR-22-58288;
Editor assigned date: 25 March, 2022, PreQC No. JPTR-22-58288 (PQ);
Reviewed date: 08 April, 2022, QC No. JPTR-22-58288;
Revised date: 24 May, 2022, Manuscript No. JPTR-22-58288 (R);
Published date: 31 May, 2022, DOI: 10.4172/JPTR.1000107
Citation: Gbiri CAO, Chukwumhua AJ (2022) Effectiveness of Physiotherapy Interventions in the Management of Impotence: A Systematic Review. J Physiother Rehab 6:5.
Abstract
Background: Impotence, common but less reported disorder with consequential psychological, emotional and physical complications. Efforts are being directed at non-pharmacological approaches in addressing this disorder, but efficacy of approaches are yet to be synchronized for clinical application. This study explored efficacy of physiotherapy for impotence and the determinants of the clinical protocol used.
Materials and nethods: Electronic search of the databases of PubMed, Physiotherapy Evidence Database (PEDro), cochrane central and Google scholar were conducted. Clinical trials were searched from inception till July 2021 with search words including impotence and Physiotherapy further refined to erectile dysfunction, premature ejaculation, exercises, electrical stimulation and biofeedback. Search strategy included expansion via medical subject headings (MeSH) and truncation of key words. Boolean operators 'AND' and 'OR' were utilized.
Results: Thirteen trials were included for review. Pelvic floor muscle exercises with or without other physiotherapeutic modalities are the common approach to the management of impotence. There was statistically significant (0.0001 ≤ p ≤ 0.05) and clinical improvement in erectile dysfunction after the interventions as compared to the controls. The approaches were more effective on erectile dysfunction of vascular origin. There were comparative improvement rates and in overall cures in premature ejaculation. Although treatment protocols varied significantly in time, protocols, contact, frequency and intensity, none of these determined their efficacy.
Conclusion: Physiotherapy is effective in the management of impotence alone or with other treatment. It is effective as first line of treatment for individuals with impotence for non-invasive options of treatment.
Keywords: Erectile dysfunction; Sexual disorder; Premature ejaculation; Physiotherapy interventions; Male sexual functioning
Introduction
Impotence constitutes a global burden in males resulting from repeated inability to achieve normal copulation including premature copulation climax, retrograded/retarded or inhibited climax, erectile dysfunction, reduced libido, orgasmic disorder and failure of detumescence and climacturia which often occurs due to pelvic floor muscle dysfunction. Erectile dysfunction and premature copulation climax in males are high, occurring in 30% to 52% of general population [1]. Reduction in the tone of the pelvic floor muscles and alterations in contractile patterns may directly impact erectile strength and climax process as a result of atrophy of the ischiocarvenosus muscles have been said to partly contribute to erectile dysfunction [2].
Despite the inherent pelvic floor muscular dysfunction, traditional management of impotence have focused on lifestyle modifications and pharmaceutical prescriptions with less focus on addressing the underlying pelvic floor dysfunction. This has led to the new paradigm involving different interventions to manage impotence. These approaches include pelvic floor muscle exercises alone or in combination with other modalities [3-6].
Although major lifestyle factors (cigarette smoking, alcohol intake, physical activity etc.) have been associated with major impotences (erectile dysfunction and premature ejaculation), moderate to high physical activity reduces risk [7]. Nevertheless, pelvic floor exercises have been found to be very satisfactory for people who refused surgery for treatments of erectile dysfunction. Pelvic floor muscle exercises with or without other physiotherapeutic modalities have been shown to be of a remarkable prospect in the management of impotence. However, it is not yet known which patients are the best candidates for it. Hence, there is need for a study that will explicitly explore the efficacy of each of the approaches and clearly delineate the best approach for each of the types of impotence. This will help in clinical decision making and clinical reasoning in the choice of most effective approach when there is need to manage a patient with impotence. Since these approaches are non-invasive and could be self-administered when well taught, the outcome of such a study will provide a better choice for individuals with impotence as well as the clinicians for most effective outcomes. Hence, this study determined the effectiveness of physiotherapy interventions and factors guiding the choice of clinical protocol in the management of impotence with specific interest in answering vital questions such as: What physiotherapy interventions are being used to manage impotence? What are the factors that determine the choice of protocol/approach for the management of impotence? What is the effectiveness of the physiotherapy interventions for the management of impotence? What factors are related/associated to the outcomes of intervention in the management of impotence? What are the determinants of the effectiveness of the choice outcome intervention in the management of impotence?
Literature Review
Methodology
This systematic review was developed and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines and protocols. The review question interrogated the determinants of the effectiveness of physiotherapy interventions and clinical protocols used in the management of impotences?
Data search and identification and selection of studies
A computerized/electronic literature search of the following databases was undertaken for relevant literature: PubMed, Physiotherapy Evidence Database (PEDro), Cochrane central and Google scholar. The search was carried out between June and July 2021 and the databases were searched from inception till July 2021. The electronic search was supplemented by a hand search of relevant references in the selected studies and previous reviews were also checked for additional references. The search strategy encompassed two key concepts from the research question: dysfunction (impotence, erectile dysfunction, pelvic floor muscle dysfunction) and intervention (physiotherapy, pelvic floor exercises, electrical stimulation, biofeedback and physical activity). The search strategy included expansion via Medical Subject Headings (MeSH) and truncation of key words. Boolean operators 'AND' and 'OR' were also utilized.
The selection criteria were based on randomized controlled trials, and randomized crossover trials and the use of one or a combination of the following physiotherapy interventions: pelvic floor muscle exercises, electrical stimulation, biofeedback, physical activity with specific focus on studies that used at least one of the following outcomes for erectile function: International Index of Erectile Function (IIEF) or the 5-item abridged version (IIEF-5), Intravaginal Ejaculatory Latency Time (IELT) and Premature Ejaculation Diagnostic Tool (PEDT). However, studies involving impotence from Multiple sclerosis, Parkinson's disease, stroke, or spinal cord injury were excluded.
Literature search
The literature search was conducted by one reviewer. After excluding duplicates of the selected articles, two reviewers then independently screened the title and abstracts of identified papers in the initial search strategy to identify eligible studies according to the inclusion and exclusion criteria. Potentially relevant studies were then retrieved for independent full text evaluation. Their references were also checked for additional relevant studies. Any discrepancies/disagreements between reviewers were discussed until a consensus was reached.
Data extraction and analysis
Data was extracted into Microsoft Word. The study features extracted from each study include publication details, study design, participants demographics, sample size, interventions (including frequency, intensity, time and type), attrition rates, number of patients randomized to control and intervention groups, mean or range age of participants, follow-up duration, a description of the intervention and control groups, mean baseline erectile function score, method of ascertainment of outcome and a summary of the primary study outcome.
Key characteristics such as sample size, age of participants, quantitative and qualitative intervention characteristics relevant to the aim of the review were summarized in Tables. These were extracted by one reviewer and consolidated by a second reviewer to ensure accuracy. Authors of the studies included for review were also contacted for necessary information that could not be accessed in the full text of the articles. Due to considerable heterogeneity in the interventions, duration and intensity, controls and results of the included studies, a narrative review of the evidence was undertaken.
Methodological quality assessment
This was assessed using the PEDro Scale. Factors considered include adequate sequence generation, allocation sequence concealment and blinding and incomplete outcome data. The PEDro Scale was developed by the physiotherapy evidence database to assess the methodological quality of a clinical trial. It is used to determine clinical trials that are likely to be internally valid and have sufficient statistical information to guide clinical decision making. There are 11 items, but each trial report is given a total PEDro score which ranges from 0 to 10. This is because the eligibility criteria are not added to the score.
Results
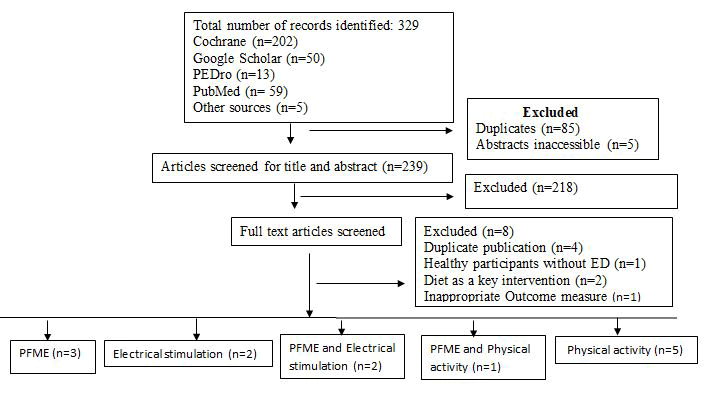
Electronic searches of databases and manual searching of reference lists of included studies and similar systematic reviews identified 329 potential studies. A total of 85 duplicates were removed and the abstracts/full texts of 5 studies were not accessible. 239 studies were screened by title and abstract and 21 of these were assessed in full text. Of these 21 studies, 13 eligible trials were identified and included in the review. The flow of studies through the review and the reasons for exclusion of studies are presented in Figure 1.
Continental spread of the studies
The studies included in the review were performed in four continents: one in Asia [8], two in Africa [9,10], three in South America [11-13], seven in Europe [14-18].
Duration and coverage periods of the studies
The study duration ranged from 10 months to 34 months and follow-up period ranged from 6 weeks to 15 months. The studies were carried out from June 2000 to October 2019, while the articles were published between November 2004 and November 2020.
Type of impotence and study design
Out of the thirteen included trials, ten trials focused on erectile dysfunction one study focused on erectile dysfunction with climacturia while the other two focused on premature ejaculation. The selected studies included three cross-over studies, one sham-controlled study, one parallel study and one independent group design. The rest were described by the authors as simply randomized controlled trials. A summary of the participants and study characteristics is given in Table 1.
| Authors | Diagnosis | AGE | INT/CON | PEDro Score | Study Design |
|---|---|---|---|---|---|
| Begot et al. 2015 | ED | 40-70 years | 41/15 | 08-Oct | RCT |
| Carboni et al. 2018 | ED | 40-65 years | 11-Nov | 09-Oct | RCT |
| Dorey et al. 2004 | ED | 22-72 years | 28/27 | 06-Oct | RCT (crossover) |
| Geraerts et al. 2015 | ED, Climacturia | ≥ 18 years | 16/17 | 06-Oct | RCT (crossover) |
| Kalka et al. 2013 | ED | ≥ 18 years | 103/35 | 04-Oct | RCT |
| Kilinc et al. 2017 | PE | 18-45 years | 35/35/35 | 05-Oct | RCT (sham control) |
| Lamina et al. 2019 | ED | 50-70 years | 25/25 | 06-Oct | RCT |
| Lin et al. 2012 | ED | 52-79 years | 41/31 | 07-Oct | RCT (crossover) |
| Palm et al. 2019 | ED | ≥18 years | 75/79 | 08-Oct | RCT |
| Pastore et al. 2012 | PE | 19-51 years | 19/21 | 05-Oct | RCT |
| Prota et al. 2012 | ED | ≥ 18 years | 26/26 | 04-Oct | RCT |
| Rislanu et al. 2020 | ED | 25-65 years | 15/15 | 08-Oct | RCT (parallel) |
| Yuksel et al. 2014 | ED | 32-83 years | 30/30 | 05-Oct | RCT |
ED=Erectile dysfunction; PE=Premature ejaculation; RCT=randomized controlled trial; Int=number in intervention group; Con=number in control group
Table 1: Participants and study characteristics.
Methodological quality assessment
There were variations in the methodological quality of the included trials with PEDro scores ranging from 4/10 to 9/10. The lower scores were attributed to a lack of blinding of the participants, therapists and assessors, and inadequate allocation concealment in some studies (Table 2).
| Authors | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Begot et al. 2015 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No |
| Carboni et al. 2018 | No | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Dorey et al. 2004 | Yes | Yes | Yes | No | No | No | No | Yes | Yes | Yes | Yes |
| Geraerts et al. 2015 | Yes | Yes | No | No | No | No | Yes | Yes | Yes | Yes | Yes |
| Kalka et al. 2013 | No | Yes | No | No | No | No | No | Yes | Yes | No | Yes |
| Kilinc et al. 2017 | Yes | Yes | No | No | No | No | No | Yes | Yes | Yes | Yes |
| Lamina et al. 2009 | Yes | Yes | No | Yes | No | No | No | Yes | Yes | Yes | Yes |
| Lin et al. 2012 | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | Yes | Yes |
| Palm et al. 2019 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes |
| Pastore et al. 2012 | Yes | Yes | No | Yes | No | No | No | No | Yes | Yes | Yes |
| Prota et al. 2012 | Yes | Yes | No | Yes | No | No | No | No | No | Yes | Yes |
| Rislanu et al. 2020 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Yes |
| Yuksel et al. 2014 | Yes | Yes | No | No | No | No | No | Yes | Yes | Yes | Yes |
1=Eligibility criteria specified; 2=random allocation of subjects; 3=allocation was concealed; 4=group similarity; 5= blinding of subjects; 6= blinding of therapists; 7=blinding of assessors; 8=outcome obtained; 9=treatment given; 10=between group comparisons; 11=point measures and measures of variability.
Table 2: The physiotherapy evidence database score of each of the studies.
Sociodemographic and clinical characteristics of the participants in the studies
A total of 912 participants were randomized from the 13 included studies: 472 to the intervention group and 440 to the control group. 79 participants dropped out during the studies and were excluded from statistical analysis. The age of participants ranged from 19 to 83 years. The underlying causes for participants identifying as having erectile dysfunction included radical prostatectomy, myocardial infarction, hypertension, ischaemic heart disease, venous occlusion, arterial insufficiency and psychogenic causes. Participants with premature ejaculation were identified as having lifelong premature ejaculation. Severity of erectile dysfunction in all the studies was mild to severe. Erectile dysfunction had lasted between 6-360 months in most participants in the studies.
Outcome measures for assessment of erectile Function
Erectile dysfunction: All eleven studies utilized the gold standard International Index of Erectile Function (IIEF) or the abridged 5-item version of the International Index of Erectile Function (IIEF-5) as the primary outcome. Other measures of sexual function included Manometric measurements and digital anal pressure measurements erectile function was assessed at baseline and at the follow up period which ranged from 6 weeks to 15 months. Erectile dysfunction was taken as a score of ≤ 20 IIEF ≤ 25.
Premature ejaculation: The two trials that investigated premature ejaculation used the Intravaginal Ejaculatory Latency Time (IELT) as an outcome. The Premature Ejaculation Diagnostic Tool (PEDT) was also reported in the one trial. One study lasted for 30 days, while the other was done over a 12 weeks period. Both studies did not report any follow-up period. Premature ejaculation was taken as IELT ≤ 60 seconds.
Physiotherapy interventions: Out of the eleven clinical trials erectile dysfunction, one study compared with placebo while one other study compared electrical stimulation to physical activity. The remaining nine studies compared the interventions to usual care. The two clinical trials on premature ejaculation compared the intervention to pharmacological intervention from prescribed Dapoxetine (a Selective Serotonin Reuptake Inhibitor (SSRI)). Three studies reported that the interventions were supervised by a physiotherapist. While the others did not specify who supervised the interventions. Frequency of physiotherapist supervision of interventions ranged from 9 to 20 sessions, with intervention lengths ranging from between 6 and 12 weeks. Interventions used in the studies include pelvic floor exercises (with or without biofeedback), electrical stimulation, aerobic exercises (walking, moderate running, bicycle ergometer, treadmill) and resistance training.
Determinants of the protocol of choice: The reviewed studies did not give details on the factors that informed the choice of intervention in each study. The following were however identified as some of the reasons the trials were carried out. Scarcity of studies on the use of the intervention of choice in impotence. No previous randomized controlled trial using the intervention of choice. Exploring the effectiveness of the intervention in erectile dysfunction after it has been used in another related condition. To determine how the intervention of choice may influence the association between the two variables being investigated.
Effectiveness of interventions: Two trials used Pelvic Floor Muscle Exercises (PFME) alone; one used PFME, electrical stimulation and biofeedback and one used PFME and biofeedback. One study used electrical stimulation alone and one used PFME and physical activity. Four trials used physical activity alone and one compared electrical stimulation to aerobic activity.
The intensity of pelvic floor muscle contractions was similar throughout the studies. Three ten-seconds’ maximal contractions were used, followed by 10 seconds relaxations, twice or thrice daily in three different positions (sitting, lying and standing). Pelvic floor muscle exercises were also incorporated in daily activities and carried out as home exercise programme.
The current type and parameters used for electrical stimulation differed. One study applied functional electrical stimulation with a frequency of 50 Hz and pulse width of 500 μs, 15 minutes, twice weekly for 4 weeks. The other study applied electrical stimulation with a frequency of 5 Hz and 150 μs pulse width, 30 minutes each, twice weekly for 6 weeks. The duration of physical activity ranged from 30 minutes to 75 minutes, carried out between two to five times a weeks (Table 3).
| Study | Intervention | Intensity | Results | Conclusion |
|---|---|---|---|---|
| Begot et al., 2015 | Home-based walking programme | 4 days a week for 1 month | 71% decrease in ED in the walking group | Better improvement in sexual function |
| Carboni et al., 2018 | Functional electrical | 15 minutes, twice a week for 4 weeks | Increase in IIEF scores in IG | FES for ED is feasible and beneficial |
| stimulation | ||||
| Dorey et al., 2004 | PFME+BFB+HEP | 3 10 sec maximal contractions, twice daily in 3 positions | 40% of participants regained normal function | PFMEs are effective for some men with ED |
| Geraerts et al., 2015 | PFME+ES | 10 mins for ES, PFME once a week for 6 weeks, alternate weekly for another 6 weeks | 6 out of 14 in the IG became potent | PFME improved ED and climacturia |
| Kalka et al., 2013 | Cycle ergometer, resistance training, indoor and outdoor exercises | 45 mins per session, 5 days a week for 6 months. | Better erection quality with higher exercise tolerance | Exercise training has a positive effect on erection quality |
| Kilinc et al., 2017 | Running and walking | 30 mins daily for 30 days | Improved IELT scores | Moderate PA had similar effects with dapoxetine |
| Lamina et al., 2019 | Aerobic exercise (bicycle ergometer) | 45-60 mins, thrice weekly for 8 weeks | 11.50 ± 5.30 vs 15.14 ± 4.92 pre and post in IG | Aerobic exercise has a significant effect on ED |
| Lin et al., 2012 | PFME+HEP | 3 10 sec contractions twice daily in 3 positions | t = 2.30, p= 0.28 at 6 months. t=2.59, p=0.14 at 12 months | PFME is effective in post prostatectomy patients |
| Palm et al., 2019 | Aerobic exercises and PFMEs | 60 mins, 3 sessions a week for 12 weeks | Mean difference in IIEF scores from p<0.0003 to p<0.0002 | Sexual rehab has a beneficial effect on erectile function |
| Pastore et al., 2012 | Physiokinesitherapy + BFB+ ES | 3 60 min sessions weekly for 12 weeks | 51% of IG improved IELT | PFME is effective for premature ejaculation |
| Prota et al, 2012 | PFME+HEP | Once weekly 30 -min sessions for 12 weeks | 47.1% potency rate in the treatment group | Early PFME has a significant impact on EF |
| Rislanu et al, 2020 | Electrical stimulation | 30 mins, 2 sessions weekly for 6 weeks | 11.17 ± 1.72 vs 20.83 ± 1.83 (p<0.05) | ES is superior to AE in ED management |
| Yuksel et al, 2014 | Aerobic exercises | 75 mins/day, 3 days a week for 6 weeks | SSD in post treatment IIEF scores | PA induces increase in penile oxygenation |
BFB=biofeedback; PFME=pelvic floor muscle exercises; ED=erectile dysfunction; EF=erectile function; FES=functional electrical stimulation; ES=electrical stimulation; HEP=Home exercise programme; IELT=intravaginal ejaculatory latency time.
Table 3: Effect of physiotherapy interventions in impotences.
Pelvic floor muscle exercises: The study by Lin et al. reports severe impotence in the participants at the beginning of the study, with a significant difference in the experimental and control group at 6 months (t=2.30, p=0.28) and 12 months (t=2.59, p=0.14). The sexual function of the intervention group was better than the control group at 6 and 12 months compared to baseline. Baseline mean and standard deviation for intervention group was 5.06 (0.24), at 6 months was 6.34 (3.46) and at 12 months 8.14 (4.86). For the control group, baseline mean, and standard deviation was 5.00 (0.00), 5.00 (0.00) at 6 months and 5.96 (0.98) at 12 months. Prota et al, reports that at 12 months post operation, 47.1% (8 out of 17) participants in the treatment group were potent compared to 12.5% (2 out of 16) participants in the control group.
Pelvic floor muscle exercises and physical activity: In the study by Palm et al. there was a significant improvement in erectile function, orgasmic function, sexual desire and satisfaction following sexual rehabilitation (PFME and aerobic exercises). There was a mean difference in IIEF scores of 6.7, 95% CI, 3.1 to 10.4 (p<0.0003) at 4 months and at 6 months, it was 6.7, 95% CI, 3.2 to 10.1 (p<0.0002).
Electrical stimulation: Carboni, et al. reports a statistically significant difference in erectile function in the intervention and control group pre and post treatment following the application of functional electrical stimulation (p<0.05).
Electrical stimulation and physical activity: Rislanu et al. reported that the post intervention analysis showed that group A, which was the electrical stimulation group had a better treatment effect compared to group B which was the aerobic exercises group. Pre and post intervention scores for both groups were 11.17 ± 1.72 vs. 20.83 ± 1.83 and 10.67 ± 1.63 vs. 14.33 ± 2.07 for the electrical stimulation and aerobic exercises group respectively.
Physical activity on erectile dysfunction: In the study by Begot et al. there was an 84% erectile dysfunction for the overall cohort at discharge. Results after 20 days of intervention however showed a 9% increase in erectile dysfunction in the control group (84% to 93%) while there was a significant 71% reduction (84% to 13%) in the physical activity (walking) group. Lamina et al. reported a significant effect of exercise on erectile dysfunction with differences in the pre and post intervention IIEF scores of both groups. The exercise group had 11.50 ± 5.30 versus 15.14 ± 4.92 while the control group had 8.10 ± 4.02 versus 8.95 ± 3.90. Kalka et al. reported better erection quality with higher exercise tolerance in the intervention group. Reported a statistically significant increase in post treatment IIEF-5 scores.
Physical activity and pelvic floor muscle exercises on premature ejaculation: Two clinical trials were found to have assessed premature ejaculation. One of the study used pelvic floor exercises described as physio-kinesitherapy, biofeedback and electrical stimulation, while the other incorporated physical activities alone as the intervention. The parameters for the electrical stimulation were not stated but the entire interventions were three 60 minutes sessions weekly, for 12 weeks. The physical activity group entailed moderate running for one group and walking for another, at least 30 minutes daily, 5 days a week for 30 days. Kilinc et al. reported a statistically significant difference in IELT scores compared to baseline for each group on the 10th, 20th and 30th day. The PEDT scores on day 30 were significantly smaller than baseline scores in the intervention and control group. Pastore et al., reported that at the end of 12 weeks of PFM rehabilitation, 11 of 19 patients (51%) were able to control the ejaculation reflex, optimizing latency time to ejaculation from the start of intravaginal intercourse. 5 patients did not respond to treatment, 2 improved after the first 20 sessions and opted to drop out of the study. The results of 11 who responded were maintained throughout the follow-up time of 3 months after the end of 12 weeks of treatment.
Factors associated with outcomes of interventions
Correlation and association of the interventions with outcomes were reported in three of the studies. Begot, et al. showed a significant negative correlation was observed between 6 minutes’ walk distance and ED 30 days after hospital discharge (r=-0.71, p<0.01). Lamina et al., found that there was a significant negative correlation between changes in C-reactive protein and IIEF scores (r=-0.588). Kalka, et al. also reported that the cardiac rehabilitation cycle was associated with a relative increase in exercise tolerance by 29.64% and in erection quality by 15.01%. Initial erection quality showed a significant association with age and initial exercise tolerance. Change in erection quality was significantly associated only with age and initial exercise tolerance.
Discussion
This study determined the effectiveness of physiotherapy interventions in the management of impotences through a systematic review. It is obvious that the most common non-invasive and non-pharmacological approach used by physiotherapists is pelvic floor muscle exercises with or without therapeutic adjuncts such as biofeedback, electrical stimulation and physical activity for the management of erectile dysfunction and premature ejaculation. This may have been promised on the fact that the major cause of impotence in male individuals is weak pelvic floor muscles. Previous studies have opined that reduction in the tone of the pelvic floor muscles and inadequacies in contractile properties are directly link to erectile strength and the ejaculatory process. So also atrophy of the ischiocarvenosus muscles has been fingered as principal contributor to erectile dysfunction. Hence, strengthening of the pelvic floor muscle may not serve as antidote to erectile dysfunction and premature ejaculation, the involvement of apparently healthy individuals in these exercises may serve as preventive measure to impotence.
The fact that the various interventions of choice were effective in the management of impotences shows that physiotherapy provides a treatment of choice for impotence. The good thing about this is that these approaches do not have any complication as compared to what is obtainable with either pharmacological or surgical approach. Exercises can be taught and be self-administered. It can also be administered through tele-medicine/physiotherapy. Hence, many patients can be treated even remotely. This provides a treatment of choice that can be administered in less sophisticated environments. Although there was significant heterogeneity such as study design, reporting methods and treatment protocols in the trials and varied with respect to physiotherapist supervision, follow-up period, intervention frequency, intensity and number of sessions which call for caution in the generalization of the results the homogeneity in the report of the efficacies of the approaches is of clinical significance at it have provided an effective treatment of choice with little or no adverse effect when administered as prescribed.
The findings that pelvic floor muscle exercises as primary intervention significantly improved erectile dysfunction shows that pelvic floor exercises alone are a good treatment of choice for adequate results. Hence, physiotherapists should integrate the entire male client to pelvic floor muscles exercises and should also be taught for preventive measure. This discovery will reduce time spent in the clinic for the management of this condition as patients will need to visit the clinic less often when they have mastered the exercises. It is very intriguing to note that the improvement achieved persisted in participants even up to a follow up period of 12 months. This shows the good carry-over effect of the approach and that is last longing.
The results that pelvic floor muscles exercises are effective and had a significant impact on recovery of sexual function following radical prostatectomy shows that the protocol can also be extended to those who have had surgical interventions for fast and comprehensive recovery of sexual functions. This does not undermine the opinion that there is uncertainty if men who have had a radical prostatectomy will benefit from pelvic floor muscles exercises because of the nerve injuries that may have coupling such a surgical intervention [19]. This debate should be a subject for further research. Hence, surgeons should be cautious during radical prostatectomy to limit the possibility of nerve injury. Both types of fibers are recruited during maximum contraction of the pelvic floor muscles. This maximum voluntary effort results in the hypertrophy of muscles and increase in their local blood supply. A combination of maximal (short) and submaximal (long) contractions allows for targeted recruitment of the differing skeletal muscle fibers of the pelvic floor. This in turn allows for the sustained tone required for an erection, as well as the short powerful contractions and reflexive responses necessary for ejaculation.
Dorey, et al. had a similar conclusion with participants in their studies had ED of various aetiology. The best results were however achieved in the group of participants with ED due to venous-occlusive dysfunction. In the study, 15 out of 20 participants with ED caused by venous-occlusive dysfunction reported a return of penile erection to allow satisfactory sexual intercourse. A physiologic explanation for the improvement of erectile dysfunction is a decrease in venous outflow. Contractions of the ischiocavernosus and bulbocavernosus muscles produce an increase in the intracavernous pressure and influence penile rigidity. The bulbocavernosus muscle compresses the deep dorsal vein of the penis to prevent the outflow of blood from an engorged penis.
The study by Pastore et al. reported a 51% improvement in the pelvic floor rehabilitation group at the end of a 12 weeks intervention period. This was evidenced by an ability to control the ejaculation reflex, optimizing latency time to ejaculation from the start of intravaginal intercourse. They compared pelvic floor exercises with on demand dapoxetine which is a selective serotonin reuptake inhibitor. Post intervention IELT was also significant in the trial. Comparing PFME and Setraline alone and as a combination, they reported that with pelvic floor exercise alone, the IELT improvement was significantly higher than that of sertraline alone. However, the amount of statistical, objective, and subjective improvement was significantly higher with sertraline on demand therapy plus pelvic floor exercises, than either of the treatment as a monotherapy. The improvement in IELT made in the Pastore, et al. study persisted by the 3 months follow up time. They however did not have a dapoxetine plus pelvic floor exercise group for comparison of treatment effect.
Carboni and Rislanu, et al. evaluated electrical stimulation for the treatment of ED, with Rislanu, et al. comparing it with aerobic exercise. Carboni, et al. reported a statistically significant difference in erectile function in the intervention group, compared to the control group, post intervention. Rislanu, et al. reported that the electrical stimulation group had a higher mean IIEF score post intervention compared to the aerobic exercise group. It was thus suggested that electrical stimulation was more superior to aerobic exercises in ED management. Also, functional electrical stimulation for ED is feasible and has some beneficial effect on erectile capacity. A limitation to both studies, however, is the small number of participants. A similar finding to both studies on the effect of electrical stimulation on erectile function has been reported by Kayigil, et al. [20]. In their study, transanal pelvic plexus stimulation caused an erection in 57% of the participants.
Electron microscopy studies have shown that ED is often caused by cavernous smooth-muscle degeneration [21,22]. Upon sexual stimulation, penile erection, occurring in response to the activation of pro-erectile autonomic pathways, is greatly dependent on adequate inflow of blood to the erectile tissue and requires coordinated arterial endothelium-dependent vasodilatation and sinusoidal endothelium-dependent cavernously smooth muscle relaxation. Nitric oxide is the principal peripheral pro-erectile neurotransmitter, released both by parasympathetic-nitrergic autonomic nerves and by the sinusoidal endothelium to produce cyclic GMP (cGMP) and relax cavernosal smooth muscle, ultimately resulting in increased intracavernosal pressure.
A 2019 study by Limanjaya, et al, demonstrated the ability of electrical stimulation to restore erectile function after cavernosal nerve injury by inducing nerve regeneration through pericytes [23]. Pericytes are bio-nanoparticle that are distributed in the erectile tissue and play important roles in the regulation of penile erection, including promoting angiogenesis and neurogenesis through interacting with endothelial cells. The increased penile strength and the resulting gain in muscular mass will improve the venous occlusion mechanism leading to required filling of corpus cavernosal bodies with blood [24,25].
The studies by Begot et al, Lamina et al and Kalka et al investigated physical activity as an intervention in ED. The ED in these studies was of cardiovascular aetiology (Acute myocardial infarction, hypertension and ischaemic heart disease). Kilinc, et al. investigated physical activity as a therapy option for PE. Compared with the on demand dapoxetine group, there was a similar effectiveness of moderate physical activity. There was no long term follow up, so there’s no certainty on how long the effect of the intervention was maintained. All studies employed aerobic exercises and Kalka et al. added resistance training. There was a wide variation of the dose of physical activity and training periods. Sessions ranged from 30-75 minutes and were carried out between 3-5 days a week that is 150 to 300 minutes per week. Intensity of the exercises was minimal to moderate intensity. Training period ranged from 30 days to 6 months. All the studies reported an improvement in erectile function with a marked 71% improvement in the Begot et al study. Kilinc, et al. also reported a statistically significant difference in IELT scores in the intervention group and the difference was observed by the 30th day of the intervention.
This is in line with the findings in the systematic review and meta-analysis of Silva, et al. [26]. They reported that physical activity and exercise improved erectile dysfunction symptoms, evidenced by a 3.85 points increase in the erectile function parameter of the IIEF questionnaire.
Their subgroup analyses also suggested that any physical activity and exercise modality is beneficial in patients with increased cardiovascular risk alone, coronary heart disease or radical prostatectomy. Also, both short-term and long-term interventions, whether used alone or with usual care, were associated with a beneficial effect.
In the review by the American Heart Association (AHA) and American College of Cardiology (ACC) Task Force published Grade B recommendations for physical activity for reduction in hypertension, which can be suggested as guidelines for men with ED. They recommend 3–4 sessions of moderate to vigorous intensity physical activity lasting 40 minutes per session corresponding to 160 minutes a week [27]. The range of intensity of physical activity by the studies included in this review fall within this recommendation of the AHA and ACC.
Khoo, et al. indicated that weekly exercise of 200 to 300 minutes of moderate intensity training results in much greater improvement of IIEF score in obese men than 90 to 150 minutes of weekly training. However, because their study group included obese men, they didn’t know if their findings would be applicable to normal-weight men with arterial ED [28]. The study of scheduled 30 participants for 6 weeks of vigorous aerobic exercise program to be carried out for 75 min a day, 3 days a week (a total of 225 minutes per week). This led to a statistically significant increase in post-treatment IIEF scores.
One of the debates on physical activity is related to its duration, with uncertainties relating to the duration and dosage of exercise. Various studies have indicated that based on the body weight, an individual performing an aerobic activity of moderate intensity lasting for 150 minutes or vigorous activity of 75 minutes a week will spend 800 to 1200 kcal (3349 to 5023 kJ) which might be sufficient for an adequate endothelial function [29]. Concluded that physical activity induces increases in both pelvic blood supply and penile oxygenation (improvement in endothelial function), and exercise capacity achieved secondary to weight loss. These all have favorable effects on the maintenance and recovery of penile erectile function. The small number of participants in their study is however a limitation to extrapolate the effect of this study as suggested by Khoo, et al.
According to the World Health Organization, healthy adults should exercise for at least 150 minutes of moderate-intensity aerobic physical activity or 75 minutes of vigorous-intensity physical activity per week. This constitutes slightly lower levels of physical activity than needed to decrease ED according to the results of this review. The recommendations by the WHO to gain additional health effects are to increase the intensity and number of weekly minutes. Thus, by following the general advice regarding physical activity, ED should be decreased.
Kalka, et al. used a combination of aerobic exercise and resistance training (cardiac rehabilitation) which yielded a positive effect on exercise tolerance and erection quality. A possible physiological basis for this could be an improvement in the testosterone concentration in the body since testosterone levels have been reported to rise after resistance training.
The physiological basis of the therapeutic effect of aerobic exercise on ED could be attributed to both immediate and long term changes in the blood vessel walls [30]. The repetitive physical activity-induced increased blood flow and vascular shear stress leads to substantial remodeling of the vascular system [31]. This adaptive response alters the endothelium by increasing the expression of nitric oxide synthase mRNA; resulting in increased synthesis of nitric oxide and improved endothelial function.
Geraerts, et al. investigated a combination of PFME and electrical stimulation with biofeedback in their study. Palm, et al. on the other hand combined PFME and physical activity (sexual rehabilitation). Both studies reported that the intervention group scored significantly better in their IIEF scores, compared to the controls. Van Kampen, et al applied a similar protocol to Geraerts, et al. as both studies used a symmetric biphasic low-frequency current was applied. Pulse frequency was 50 Hz for both studies but the pulse duration was 200 microseconds, 15 minutes and 600 microseconds for 10 minutes respectively. Electrical stimulation was added to improve awareness of the muscles of the pelvic region and to assist the patient in contracting the ischiocavernous and bulbocavernous muscles. The participant’s performance was further enhanced by the use of electromyographic biofeedback in order to visualize and quantify the muscle contractions.
Pastore, et al. (combined PFME and electrical stimulation [32]. The effect may have been beneficial because the addition of electrical stimulation may increase the rate, intensity and synchronization of motor unit firing [33-60]. Thus, through additional motor unit recruitment and altered frequency of firing, corrected patterns of contraction of the bulbocavernosus muscle can occur, allowing greater conscious control of the ejaculatory process [60-74].
Conclusion
Physiotherapy is an effective non-pharmacological and non-invasive intervention in the treatment of erectile male dysfunction and premature ejaculation. Pelvic floor muscle exercises (with or without biofeedback), electrical stimulation and physical activity are currently in use as non-pharmacological interventions for erectile dysfunction and premature ejaculation. These interventions have been shown to be effective either as a monotherapy or combination therapy. Erectile dysfunction of various aetiology has been shown to benefit from these studies, though the intervention seemed to have greater effects on erectile dysfunction of vascular origin. However, due to the wide variability of protocol, it is difficult to draw informed conclusions about respective protocol efficacies and the exact protocol required to achieve the best results. The level of an individual’s physical activity and fitness level has been shown to influence the erectile function and biomarkers of systemic vascular inflammation, leading to an improvement in endothelial function. Physiotherapy interventions could thus be proposed as a first line of treatment for patients with impotences seeking alternate options to medications.
References
- Hatzimouratidis K, Giuliano F, Moncada A, Muneer A, Salonia A, et al. (2016). Guidelines on erectile dysfunction, premature ejaculation, penile curvature and priapism. Arnhem, The Netherlands: EAU Guidelines Office.
- Kannan P, Winser SJ, Ho LC, Hei LC, Kin LC, et al. (2019) Effectiveness of physiotherapy intervention foe improving erectile function and climacturia in men after prostatectomy: A systematic review and meta-analysis of randomized controlled trials. Clin Rehabil 33:1298-1309.
- Dorey G (2000) Conservative treatment of erectile dysfunction. 3: literature review. Br J Nurs 9:859–863.
- Van Kampen M, Geraerts I (2015) Male pelvic floor dysfunctions and evidence-based physical therapy. In: Bo K, Berghmans B, MorkveS, Van Kampen M (eds). Evidence-based physical therapy for the pelvic floor. 2nd ed. New York, NY: Churchill Livingstone; p.271–301.
- Dorey G, Speakman M, Feneley R, Swinkels A, Dunn C, Ewings E (2004) Randomised controlled trial of pelvic floor muscle exercises and manometric biofeedback for erectile dysfunction. Br J Gen Pract 54:819-825.
- Rosenbaum TY (2007) Pelvic floor involvement in male and female sexual dysfunction and the role of pelvic floor rehabilitation in treatment: a literature review. J Sex Med 4:4–13. [Googlescholar]
- Rosenbaum TY, Owens A (2008) The role of pelvic floor physical therapy in the treatment of pelvic and genital pain related sexual dysfunction: Erratum. J Sex Med 5:1513.
- Lin Y, Yu T, Lin V, Wang H, Lu K (2012) Effects of Early Pelvic-Floor Muscle Exercise for Impotence in Radical Prostatectomy Recipients. Cancer Nurs 35:106-114.
- Lamina S, Okoye CG, Dagogo TT (`2009) Therapeutic Effect of an Interval Exercise Training Program in the Management of Erectile Dysfunction in Hypertensive Patients. J Clin Hypertens (Greenwich) 11:125–129.
- Rislanu A, Auwal H, Musa D, Auwal A (2020) Comparative Effectiveness of Electrical Stimulation and Aerobic Exercise in the Management of Erectile Dysfunction: A Randomized Clinical Trial. Ethiop J Health Sci 30:961-970.
- Begot I, Peixoto T, Gonzaga LR, Bolzan DW, Papa V, et al. (2015) A Home-Based Walking Program Improves Erectile Dysfunction in Men With an Acute Myocardial Infarction. Am J Cardiol 115:571-575.
- Carboni C, Fornari A, Bragante K, Averbeck M, da RosaPV, et al. (2018) An initial study on the effect of functional electrical stimulation in erectile dysfunction: a randomized controlled trial. Int J Impot Res 30:97–101.
- Prota C, Gomes CM, Ribeiro LH, Bessa J, Nakano E, et al. (2012) Early postoperative pelvic-floor biofeedback improves erectile function in men undergoing radical prostatectomy: a prospective, randomized, controlled trial. Int J Impot Res 24:174-178.
- Pastore L, Palleschi, G, Leto A, Pacini L, Iori F, et al. (2012) A prospective randomized study to compare pelvic floor rehabilitation and dapoxetine for treatment of lifelong premature ejaculation. Int J Androl 35:528–533.
- Palm P, Zwisler AD, Svendsen JH, Thygesen LC, Giraldi A, et al. (2019) Sexual rehabilitation for cardiac patients with erectile dysfunction: a randomised clinical trial. Heart 105:775–782.
- Kilinc MF, Aydogmus Y, Yildiz Y, Doluoglu OG (2017) Impact of physical activity on patient self-reported outcomes of lifelong premature ejaculation patients: Results of a prospective, randomised, sham-controlled trial. Andrologia e12799.
- Kałka D, Domagała Z, Dworak J, Womperski K, Rusiecki L, et al. (2013) Association between physical exercise and quality of erection in men with ischaemic heart disease and erectile dysfunction subjected to physical training. Kardiol Pol 71:573-580.
- Geraerts I, Van Poppel H, Devoogdt N, De Groef A, Fieuws S, Van Kampen M (2015). Pelvic floor muscle training for erectile dysfunction and climacturia 1 year after nerve sparing radical prostatectomy: a randomized controlled trial. Int J Impot Res 28:9-13.
- Dorey G, Glazener C, Buckley B, Cochran C, Moore K (2009) Developing a pelvic floor muscle training regimen for use in a trial intervention. Physiotherapy 95:199-209.
- Kayigil O, Agras K, Gurdal M, Serefoglu EC, Okulu E, et al. (2007) Effects of transanal pelvic plexus stimulation on penile erection: clinical implications. Int Urol Nephrol 39:1195-1201.
- Jiang J, He Y, Jiang R. (2009). Ultrastructural changes of penile cavernous tissue in multiple sclerotic rats. J Sex Med 6:2206–2214.
- Hatzimouratidis K, Amar E, Eardley I, Giuliano F, Hatzichristou D, Montorsi F, et al (2010). Guidelines on impotence: erectile dysfunction and premature ejaculation. Eur Urol 57:804–14.
- Limanjaya A, Kwon MH, Song KM, Ghatak K, Minh NN, et al. (2019) Pericyte derived exosome promotes cavernous angiogenesis and neural regeneration and rescues erectile function. J Urol 201:e386.
- Sturny M, Karakus S, Fraga-Silva R, Stergiopulos N, BurnettA L (2019) Long-term low intensity electrostimulation of injured cavernosal nerve improves erectile function recovery in a rat model postprostatectomy erectile dysfunction. J Sex Med 16:S13-S14.
- Shafik A (2000) The role of the levator ani muscle in evacuation, sexual performance, andpelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct 11:361–76.
- Silva AB, Sousa N, Azevedo LF, Martins C (2017) Physical activity and exercise for erectile dysfunction: systematic review and meta-analysis. Br J Sports Med 51:1419–1424.
- Eckel RH, Jakicic JM, Ard JD (2013) AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol; 63:2960-2984.
- Khoo J, Tian H, Tan B, Chew K, Ng CS, et al. (2013) Comparing Effects of Low and High-Volume Moderate-Intensity Exercise on Sexual Function and Testosterone in Obese Men. J Sex Med 10:1823–1832.
- O'Donovan G, Blazevich AJ, Boreham C, Cooper AR, Crank H, et al. (2010) The ABC of physical activity for health: A consensus statement from the British Association of Sport and Exercise Sciences. J Sports Sci 28:573-591.
- Lamina S, Agbanusi EC, Nwacha RC (2011) Effects of Aerobic exercise in the management of erectile dysfunction. Ethiop J Health Sci 21:125-129.
- Hawley JA, Hargreaves M, Joyner MJ, Zierath JR (2014) Integrative biology of exercise. Cell. 159:738–749.
- Myers C, Smith M (2019) Pelvic floor muscle training improves erectile dysfunction and premature ejaculation: a systematic review. Physiotherapy 105:235–243.
- Kalka D, Domagala ZA, Kowalewski P, Rusiecki L, Koleda P, et al (2015). Effect of endurance cardiovascular training intensity on erectile dysfunction severity in men with ischemic heart disease. Am J Mens Health 9:360–369.
- Kałka D, Domagała Z, Rusiecki L, Karpiński Ł, Gebala J, et al. (2016) Heart rate recovery, cardiac rehabilitation and erectile dysfunction in males with ischaemic heart disease. Anatol J Cardiol 16:256-263.
- Lue TF, Gleason CA, Brock GB, Carroll PR, Tanagho EA (1995) Intraoperative electrostimulation of the cavernous nerve: technique, results and limitations. J Urol 154:1426–1428.
- Lue TF, Giuliano F, Montorsi F, Rosen CR, Karl-Erik Andersson, et al. (2004). Summary of the recommendations on sexual dysfunctions in men. J Sex Med 1:6–23.
- Peng J, Fang D, Li H, Tang Y, Yuan Y, Cui W, et al. (2020) Efficacy of dapoxetine treatment in Chinese patients with premature ejaculation and possible factors affecting efficacy in the real-world practice. BMC Urol 20:11–16.
- Philippou YA, Jung JH, Steggall MJ (2018) Penile rehabilitation for postprostatectomy erectile dysfunction. Cochrane Database Syst Rev 10:CD012414.
- Prieto D (2008) Physiological regulation of penile arteries and veins. Int J Impot Res 20:17–29
- Raveendran A, Agarwal A (2021) Premature ejaculation current concepts in the management. Int J Reprod Biomed 19:5-22.
- Rebar AL, Stanton R, Geard D, Short C, Duncan MJ, et al. (2015) A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol Rev 9:366–378.
- Rivalta M, Sighinolfi MC, De Stefani S, Micali S, Mofferdin A, et al. (2009) Biofeedback, electrical stimulation, pelvic floor muscle exercises, and vaginal cones: a combined rehabilitative approach for impotence associated with urinary incontinence. J Sex Med 6:1674–1677.
- Rivalta M, Sighinolfi MC, Micali S, De Stefani S, Bianchi G (2010) Sexual function and quality of life in women with urinary incontinence treated by a complete pelvic floor rehabilitation program (biofeedback, functional electrical stimulation, pelvic floor muscles exercises, and vaginal cones). J Sex Med 7:1200–1208.
- Rosen R, Altwein J, Boyle P, Kirby RS, Lucacs B, et al. (2003) Lower urinary tract symptoms and impotence: the multinational survey of the ageing male (MSAM-7). Eur Urol 44:637–649.
- Yoshida M, Matsunaga A, Igawa Y, Fujimura T, Shinoda Y, AizawaN, et al. (2018) May perioperative ultrasound-guided pelvic floor muscle training promote early recover of urinary continence after robot-assisted radical prostatectomy?Neurourol Urodyn38:158-164.
- Siegel AL (2014) Pelvic floor muscle training in males: Practical applications. J Urol 84:1-7.
- Ponholzer A, Temml Ch, Marszalek M, Obermayr R, Madersbacher S (2005) Prevalence and risk factors for erectile dysfunction in 2869 men using a validated questionnaire. Eur Urol 47:80–86.
- Porst H, Burri A (2019) Novel treatment for premature ejaculation in the light of currently used therapies: A review. Sex Med Rev 7:129–140.
- Rosen RC (2001) Measurement of male and female sexual dysfunction. Curr Psychiatry Rep 3:182–187.
- Rosen RC, Cappelleri JC, Smith MD, et al (2001) Development and evaluation of an abridged 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res 11:319-326.
- Rosen RC, Giuliano F, Carson CC (2005) Impotence and lower urinary tract symptoms (LUTS) associated with benign prostatic hyperplasia (BPH). Eur Urol 47:824–837.
- Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, et al. (1997) The International Index of Erectile Function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 49:822–830.
- Schmidt HM, Munder T, Gerger H, Frühauf S, Barth J (2014) Combination of psychological intervention and phosphodiesterase-5 inhibitors for erectile dysfunction: a narrative review and meta-analysis. J Sex Med 11:1376–1391.
- Schouman M, Lacroix P (1991) Apport de la re´e´ducation pelvi-pe´rine´ale au traitement des fuites veino-caverneuses. Ann Urol 25:92–93.
- Serefoglu EC, McMahon CG, Waldinger MD, Althof SE, Shindel A, et al. (2014) An evidence-based unified definition of lifelong and acquired premature ejaculation: Report of the second International Society for Sexual Medicine Ad Hoc Committee for the Definition of Premature Ejaculation. J Sex Med 11:1423–1441.
[Google Scholar] [Crossref] [Indexed]
- Shafik (1996) Extrapelvic cavernous nerve stimulation in erectile dysfunction. Andrologia 28:151–156.
- Shamloul R, Ghanem H (2013) Erectile dysfunction. Lancet 381:153–165.
- Sherburn M, Murphy CA, Carroll S, Allen TJ, Galea MP (2005) Investigation of transabdominal real time ultrasound to visualise the muscles of the pelvic floor. Aust J Physiother 51:167-170.
- Stafford RE, Ashton-Miller JA, Constantinou C, Coughlin G, Lutton NJ, et al. (2006) Pattern of activation of pelvic floor muscles in men differs with verbal instructions. Neurourol Urodyn 35:457–463.
- Strassberg DS, Perelman MA (2009) Impotences. In: Blaney PH, Millon T (eds) Oxford textbook of psychopathology, 2nd edition. Oxford University Press, New York, pp 399–430.
- Tajkarimi K, Burnett AL (2011) The role of genital nerve afferents in the physiology of the sexual response and pelvic floor function. J Sex Med 8:1299–1312.
- Waldinger MD, Quinn P, Dilleen M, Mundayat R, Schweitzer DH, et al. (2005) Ejaculation disorders: A multinational population survey of intravaginal ejaculation latency time. J Sex Med 2:492–497.
- Waldorf M, Erkens N, Vocks S, McCreary DR, Cordes M (2017) A single bout of resistance training improves state body image in male weight-trainers. Sport Exerc Perform Psychol 6:53–69.
- Wang W, Fan J, Huang G, Zhu X, Tian Y, et al. (2017) Meta-analysis of prevalence of erectile dysfunction in mainland China: evidence based on epidemiological surveys. Sex Med 5:19–e30.
- Warburton DE, Bredin SS (2017) Health benefits of physical activity: a systematic review of current systematic reviews. Curr Opin Cardiol 32:541–556.
- Watrelot A, Ruggeri J, Dumoulin S, Lavoisier P, Roy P, Dantony E (2014). Pelvic-Floor Muscle Rehabilitation in Erectile Dysfunction and Premature Ejaculation. Physiotherapy 94:1731-1743.
- Wernbom M, Augustsson J, Thomeé R (2007) The influence of frequency, intensity, volume and mode of strength training on whole muscle cross-sectional area in humans. Sports Med 37:225–264.
- Wespes E, Nogueira MC, Herbaut AG, Caufriez M, Schulman CC (1990) Role of the bulbocavernosus muscles on the mechanism of human erection. Eur Urol 18:45–48.
- Wing R, Rosen RC, Fava JL, Bahnson J, Brancati F, et al (2010) Effects of Weight Loss Intervention on Erectile Function in Older Men with Type 2 Diabetes in the Look AHEAD Trial. J Sex Med. 7:156–165.
- Wong BLK, Malde S (2013) The use of tramadol “on demand” for premature ejaculation: A systematic review. Urol 81:98–103.
- World Health Organization (2021) Global strategy on diet, physical activity and health. Physical activity and adults. Department of Human Health Service.
- Yakubu MT, Akanji MA, Oladiji AT (2007) Impotence and methods used in assessing medicinal plants with aphrodisiac potentials. Phcog Rev 1:49-56.
- Yehuda I (2007) Pelvic floor involvement in male and feimpotence and the role of pelvic floor rehabilitationin treatment: a literature review. J Sex Med 4:4–13.
- Yüksela OH, Memeto˘glub OG, Ürkmeza A, Ilknur A¸ Verit A (2015). The role of physical activity in the treatment of erectile dysfunction. Revista Internacional de Andrologia 13:115-119.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi