Research Article, J Spine Neurosurg Vol: 9 Issue: 3
Epidural steroid injection for low back pain and lumbosacral radiculopathy; experience from a neurosurgery center in a developing country
Saqib Kamran Bakhshi1, Kaynat Siddiqui2 and Aneela Darbar1*
Section of Neurosurgery, Department of Surgery, Aga Khan University Hospital, Karachi, Pakistan
Jinnah Sindh Medical University, Karachi, Pakistan
*Corresponding : Aneela Darbar
Consultant Neurosurgeon, Section of Neurosurgery
Department of Surgery, Aga Khan University Hospital, Karachi, Pakistan
E-mail: aneela.darbar@aku.edu
Received: April 10, 2020 Accepted: April 27, 2020 Published: May 05, 2020
Citation: Bakhshi SK, Siddiqui K, Darbar A (2020) Epidural Steroid Injection for Low Back Pain and Lumbosacral Radiculopathy; Experience from a Neurosurgery Center in a Developing Country. J Spine Neurosurg 9:4.
Abstract
Background: Epidural steroid injections (ESI) have been in use for management of low back pain and radiculopathy, however, there is still variation in literature regarding their utility and effectiveness. We wanted to study the usefulness of ESI for pain relief in a developing country where resource constraints are a challenge in seeking surgical care.
Methods: It was a retrospective review of patients’ records between 2013 and 2017 (5 year period). After obtaining ethical exemption data, including demographics, symptoms, number of injections, extent of pain relief and duration of relief were recorded on a performa. All patients had been administered ESI with local anesthetic Bupivacaine by a single neurosurgeon in the operating room under fluoroscopy guidance.
Results: Sixty three patients were included in the study. Low back pain was common symptom in all patients and Forty nine patients (77.8%) had radicular symptoms as well, most commonly in the L5 distribution. Forty five patients (71.4%) had significant relief in pain after ESI. The median duration of symptom relief was 7 months. Only two patients had complained of headaches requiring medical attention following injections. We did not find any significant predictors of pain relief after ESI in our study.
Conclusion: We recommend ESI as an effective tool of pain management for low back pain and radiculopathy. It can be offered to patients who are not willing for surgery or have significant medical ailments increasing general anesthesia risks, and also for patients in low- and middle-income countries as a cost-effective treatment.
Keywords: Epidural steroid injection; Low back pain; Radicular pain
Introduction
Low back pain (LBP), with or without radiculopathy, is a leading cause of disability worldwide, and one of the commonest reasons for visit to neurosurgery clinic. LBP has a lifetime prevalence ranging between 40% and 70% [1]. Degenerative changes in the spine involving disc herniation, and facet joint arthropathy, spondylolisthesis or spinal canal stenosis by bone or surrounding soft tissue have been attributed to be the foremost cause of these symptoms [2-5].
Diagnosing the cause and treating LBP and lumbar radiculopathy can be a difficult task particularly in young patients. Various treatment modalities including conservative approaches with analgesics and physiotherapy, interventions such as epidural steroid injections (ESI) and surgical treatment options have been used for this condition [4-8]. ESI are the only treatment option for patients who do not respond to conservative measures or develop side effects of prolonged oral antiinflammatory drugs, and are not fit for surgery, or those with mild to moderate stenosis [9-11].
The advantage of nerve root injections, is to reduce pain faster and quicker than any other modality, though the duration of symptom relief is highly variable [12]. Inter-laminar approach is most commonly applied for ESI followed by caudal injections and transforaminal approach. An important advantage of this intervention is its cost-effectiveness, particularly in low to middle income countries like Pakistan, where the cost of regular oral analgesics and narcotics is a serious socioeconomic burden. Few studies conducted in Pakistan have reported good outcomes with regards to symptom relief in patients who are administered ESI [13-15].
Despite frequent use, the efficacy of this treatment modality is still controversially reported in different studies and is still a subject of ongoing research [16]. We aimed to study the indications, outcomes and duration of pain relief after ESI for back pain and lumbosacral radiculopathy administered by a single neurosurgeon at our hospital.
Methods
It was a retrospective cohort study, conducted at Aga Khan University hospital. Ethical exemption was obtained from the institutional review board. Patients’ medical records were retrieved using ICD 9 coding system. We included all patients; irrespective of age and gender, who were administered ESI for low back pain or lumbosacral radiculopathy, by a single surgeon (principle investigator) between January 2013 and December 2017. Patients with incomplete records were excluded. Data was collected on a pre-structured questionnaire which included demographic details, symptoms, duration of complains, nerve roots involved, number of epidural injections administered, extent of pain relief, complications and follow-up.
Statistical analysis was done using SPSS version 21. Data was not normally distributed so non-parametric tests were applied. Continuous data has been presented as median with interquartile range (IQR). Categorical data has been presented as frequency and proportion. Chi-square test has been used to compare categorical data. P-value of < 0.05 was taken as statistically significant.
Pain relief was assessed on a scale of 0 to 10, with 0 being no relief and 10 being complete relief in pain. Patients who reported score of 0 to 2 were included in the no relief category, those with scores of 3 to 7 were included in the partial relief category, and those with scores of 8 to 10 were included in the significant relief group.
Procedure of epidural injection
All procedures were performed in the operating room. After taking informed consent, patients were positioned in left lateral position and relevant interlaminar space was marked using C-arm Fluoroscopy machine. Using 25G long needle, 10 ml of 1% plain xylocaine was locally injected. A 20G or 22G lumbar puncture needle was then advanced in the interlaminar space under image guidance upto the epidural space, and 1 ml of 0.5% plain Bupivacaine with 80mg Methylprednisolone was injected. Patients who were diabetic were administered a lower dose of Methylprednisolone (40 mg). Needle was flushed with 2 ml of 0.9% normal saline and then withdrawn. Patients were observed in operating room recovery for 2 hours and were then discharged.
Results
Sixty three patients were included in the study. Median age was 55 years and number of female patients was slightly higher than males (n=37; 58.7%). Around one-third of the patients were morbidly obese (n=23; 36.5%). All patients had complain of low back pain, while 49 patients (77.8%) complained of radicular symptoms as well. Radicular pain was most common in L5 dermatome (n=42; 85.7%), so L4-L5 inter-laminar epidural space was most commonly negotiated for injection (Table 1).
Table 1: Demographics and clinical characteristics.
More than half of the patients (71.4%) had significant relief in pain after first injection. Out of these, seven patients (11.1%) had a second epidural injection and 2 patients (3.2%) had a third epidural injected at irregular intervals. Two patients (3.2%) had complained of prolonged headache that required medical treatment, and 1 patient (1.6%) had pain at injection site. None of the patients had acquired injection site meningitis, cellulitis or meningitis after the procedure (Table 2 and Figure 1).
Table 2: Patient characteristics and pain relief.
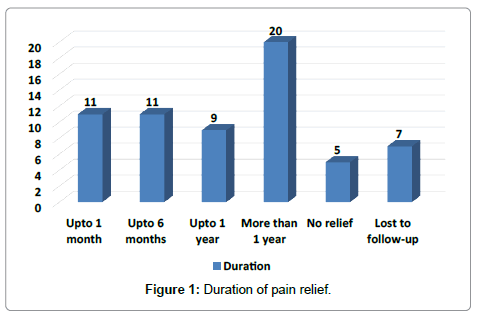
Figure 1: Duration of pain relief.
Discussion
It is not yet entirely known how ESI cause reduction in pain intensity, however, the anti-inflammatory properties of steroids have been postulated to cause relief from noxious stimuli [17-20] Several cohort studies, trials and reviews have reported conflicting results on the role of ESI for chronic LBP and lower extremity pain. Our study found significant relief in LBP and radicular symptoms in most of the patients after ESI which was effective for an average of 7 months. Laiq et al. had conducted a case control study comparing use of epidural steroids with conservative treatment for lumbar radiculopathy and had administered 80mg methylprednisolone with 2% plain xylocaine to half of their patients (n=25). They reported statistically significant relief in pain in the steroid group as compared to the control group which had received oral NSAIDS [13]. They had reported no major complications and only 4 patients (16%) had reported short-term headaches.[13] Most of their patients (68%) had pain relief upto 6 months after the procedure and our observation of 7 months of pain relief is comparable.
Muhammad et al. [15] had conducted a prospective cohort study on role of ESI for chronic LBP with sciatica. They had included 75 patients in their study and an anesthetist had administered 2ml of methylprednisolone and 2ml of bupivacaine to the patients in the epidural space. They had reported upto 80% relief in pain severity in 49 (65%) patients at 6 weeks and these patients were administered a second ESI at 3 months and a third ESI at 6 months which resulted in sustained relief in pain We have found 100% relief in pain in 71.4% patients at last follow-up and only 14.3% of these had a second or third ESI at irregular intervals. Sherafgan et al. reported a case series of 50 patients who were administered caudal steroid injection at the Orthopedics unit of their hospital. Their outcome measure was improvement in patients’ functional outcomes after injection. It was reported in their study that at 3 months follow-up, 20% patients had excellent outcomes and 48% had good outcomes according to Macnab’s criteria [14]. Meng et al. had conducted a meta-analysis of 13 trials regarding epidural injections with or without steroids for chronic LBP due to spinal stenosis. The analysis involved 1465 patients and they reported significant reduction in pain in 53.7% patients who were given ESI and 56.4% patients who were administered local anesthetic alone [21]. Significant functional improvement was also reported in around two-thirds of patients. They had recommended use of epidural injections for pain relief, however, inclusion of steroids did not add any additional benefit in terms of degree and duration of pain relief [21]. The trials included in this meta-analysis were heterogenous in terms of dosage of drugs, follow-up time and injection frequency. The approach for injection was also not homogenous and 3 trials had a sample size of less than 50 patients [21].
In another meta-analysis of 10 trials, Zhai et al. [22] had reported significant reduction in pain in 41.7% patients after ESI with local anesthetic and in 40.2% patients who were administered local anesthetic only.They had concluded that average time of pain relief was 31.67 weeks with 3.68 procedures in ESI with local anesthetic cluster and 32.64 weeks with 3.68 procedures in the local anesthetic–only cluster [22].Their analysis established that there was no significant advantage of ESI with local anesthetic over local anesthetic alone in patients with chronic low back pain and lower extremity pain [22].
In a recently publishes case series, Shrestha et al. assessed the effectiveness of trans-foraminal epidural steroid injection in 67 patients with low back pain and radiculopathy. They reported statistically significant pain relief in around 75% of these patients at 3 months from the procedure and recommended it to be a safe modality for pain relief [23]. An important aspect associated with inadequate pain relief after ESI is performing the procedure blindly, which can result in incorrect localization of the target in up to 30% cases. In recent years, use of fluoroscopic and computed tomography guidance has resulted in better outcomes in terms of pain relief, likely due to more accurate injection of the anesthetic agents [24].
We did not find any significant predictors of pain relief in our population, likely due to smaller sample size. We did not study the impact of dose of Methylprednisolone on the duration of pain relief, which can be an interesting fact for further research.
Conclusion
We recommend that administration of ESI with local anesthetic likely has a significant impact in relieving chronic low back pain and radicular pain. ESI can be offered to patients who are not willing to undergo surgical procedures upfront, or who have significant co-morbid conditions as around 3 quarters of all patients in our study reported complete relief in pain for an average of 7 months. The ambiguity in literature will remain unless a standard protocol is devised for the administration of ESI, as rising costs of surgery will make more patients inclined towards this minimally invasive procedure.
References
- Cohen SP, Bicket MC, Jamison D, Wilkinson I, Rathmell JP (2013) Epidural steroids: a comprehensive, evidence-based review. Reg Anesth Pain Med 38: 175-200.
- Haig AJ, Tomkins CC (2010) Diagnosis and management of lumbar spinal stenosis. JAMA 303: 71-72.
- Tosteson AN, Tosteson TD, Lurie JD, Abdu W, Herkowitz H, et al. (2011) Comparative effectiveness evidence from the spine patient outcomes research trial: surgical versus nonoperative care for spinal stenosis, degenerative spondylolisthesis, and intervertebral disc herniation. Spine 36: 2061-2068.
- Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, et al. (2010) Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 303: 1259-1265.
- Chen E, Tong KB, Laouri M (2010) Surgical treatment patterns among Medicare beneficiaries newly diagnosed with lumbar spinal stenosis. Spine J 10: 588-594.
- Tosteson AN, Lurie JD, Tosteson TD (2008) Surgical treatment of spinal stenosis with and without degenerative spondylolisthesis: cost-effectiveness after 2 years. Ann Intern Med 149: 845-853.
- Manchikanti L, Cash KA, McManus CD, Pampati V, Fellows B (2012) Fluoroscopic caudal epidural injections with or without steroids in managing pain of lumbar spinal stenosis: one-year results of randomized, double-blind, active-controlled trial. J Spinal Disord Tech 25: 226-234.
- Manchikanti L, Cash KA, McManus CD, Damron KS, Pampati V, et al. (2012) Lumbar interlaminar epidural injections in central spinal stenosis: preliminary results of a randomized, double-blind, active control trial. Pain Physician 15: 51-63.
- Manchikanti L, Helm Ii S, Singh V, Hirsch JA (2013) Accountable interventional pain management: a collaboration among practitioners, patients, payers, and government. Pain Physician 16: E635-E670.
- Manchikanti L, Pampati V, Falco FJ, Hirsch JA (2013) Assessment of the growth of epidural injections in the medicare population from 2000 to 2011. Pain Physician 16: E349-E364.
- Manchikanti L, Pampati V, Falco FJ, Hirsch JA (2013) Growth of spinal interventional pain management techniques: analysis of utilization trends and medicare expenditures 2000 to 2008. Spine (Phila Pa 1976) 38: 157-168.
- Benditz A, Brunner M, Zeman F, Greimel F, Florian V, et al. (2017) Effectiveness of a multimodal pain management concept for patients with cervical radiculopathy with focus on cervical epidural injections. Sci Rep 1:7866.
- Laiq N, Khan MN, Iqbal MJ, Khan S (2009) Comparison of epidural steroid injections with conservative management in patients with lumbar radiculopathy. J Coll Physicians Surg Pak 19: 539-543.
- Sherafgan, Ahmad MI, Saeed R, Khalid O (2014) Improved Functional Outcome in Patients with Lumbar Disc Prolapse Treated with Caudal Epidural Steroid Injections. Journal of Pakistan Orthopaedic Association 26: 4.
- Muhammad T, Kumar M, Hashmi IA, Khatri MY (2016) Lumbar interlaminar epidural injections in managing chronic low back pain with sciatica without using fluoroscopy. J Surg Pakistan 21:45- 48.
- Benyamin RM, Manchikanti L, Parr AT, Diwan S, Singh V, et al. (2012) The effectiveness of lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain. Pain Phys 4: E363-E404.
- Manchikanti L (2002) Role of neuraxial steroids in interventional pain management. Pain Physician 5: 182-199.
- Byrod G, Otani K, Brisby H, Rydevik B, Olmarker K (2000) Methylprednisolone reduces the early vascular permeability increase in spinal nerve roots induced by epidural nucleus pulposus application. J Orthop Res 18: 983-987.
- Lundin A, Magnuson A, Axelsson K, Nilsson O, Samuelsson L (2005) Corticosteroids peroperatively diminishes damage to the C-fibers in microscopic lumbar disc surgery. Spine 30(21): 2362-2367.
- Hayashi N, Weinstein JN, Meller ST, Lee HM, Spratt KF, et al. (1998) The effect of epidural injection of betamethasone or bupivacaine in a rat model of lumbar radiculopathy. Spine 23: 877-885.
- Meng H, Fei Q, Wang B, Yang Y, Li D, et al. (2015) Epidural injections with or without steroids in managing chronic low back pain secondary to lumbar spinal stenosis: a meta-analysis of 13 randomized controlled trials. Drug Des Devel Ther 9: 4657-4667.
- Zhai J, Zhang L, Li M, Tian Y, Zheng W, et al. (2015) Epidural injection with or without steroid in managing chronic low back and lower extremity pain: ameta-analysis of ten randomized controlled trials. Am J Ther 8: 8304-8316.
- Shrestha P, Subba L, Agrawal P, Lohani S (2020) Outcome of transforaminal epidural steroid injection for lumbar radiculopathy: initial three-year experience at Upendra Devkota Memorial-National Institute of Neurological and Allied Sciences, Nepal. Chinese Neurosurgical Journal 6: 6.
- Sung MS (2006) Epidural steroid injection for lumbosacral radiculopathy. Korean J Radiol 7: 77-79.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi 
