Case Report, J Physiother Rehabil Vol: 1 Issue: 1
Examination and Conservative Management of Shoulder Pain:A Systematic Tissue Specific Approach
S Christopher Owens*
Department of Physical Therapy, Hampton University, Virginia, United States of America
*Corresponding Author : S. Christopher Owens
Associate Professor, Department of Physical Therapy, Hampton University, Virginia, United States of America
Tel: 757 727-5847
E-mail: stephen.owens@hamptonu.edu
Received: October 28, 2017 Accepted: November 10, 2017 Published: November 14, 2017
Citation: Owens SC (2017) Examination and Conservative Management of Shoulder Pain: A Systematic Tissue Specific Approach. J Physiother Rehabil 1:1.
Abstract
The use of examination procedures to identify specific tissue involvement in painful conditions is a critical element in musculoskeletal physical therapy practice. Physical therapists can benefit from this approach to patient examination because it allows them to focus treatments on the specific causes of symptoms. The purpose of this case study is to describe a systematic approach to examination and treatment of shoulder pain through the identification of specific pain generators. The patient presented in this case had a five month onset of left anteriolateral shoulder pain. Based on the examination findings the physical therapy treatment diagnosis was subscapularis tendinopathy with subacromial bursitis. Initial treatment consisted of manual therapy for symptom. The final phase consisted of scapular stabilization activities and eccentric subscapularis exercise. At discharge the patient returned to all activities and stated that she only noticed her shoulder symptoms when she had a particularly busy shift. This case suggests that using a tissue specific examination and treatment approach may be beneficial in achieving a successful outcome in the treatment of patients with shoulder pain
Keywords: Rotator cuff; Tendinopathy; Subscapularis; Manual therapy
Introduction
Shoulder pain is the second most common musculoskeletal reason for seeking medical attention preceded only by knee pain [1]. Throwing and overhead athletes such as pitchers, swimmers, and tennis players are commonly affected. Individuals involved in professions that require frequent reaching, pushing, and pulling are also at increased risk for developing shoulder pain. Leclerc et al found a forty five percent prevalence of shoulder pain in a population of individuals employed in professions requiring repetitive upper extremity work [2]. The muscles and tendons of the rotator cuff are frequently associated with shoulder pain. Browning and Desai reported that rotator cuff pathology was present in thirty nine to sixty percent of cadaveric specimens [3]. The most frequent tendon involved with pathology of the shoulder is the supraspinatus tendon. Tendinopathy often occurs in the area of hypovascularity one centimeter proximal from the insertion of the supraspinatus tendon on the humeral greater tuberosity [4].
The subscapularis is the strongest of the rotator cuff muscles and is critical for anterior stability of the glenohumeral joint [5]. The subscapularis tendon has an abundant vascular supply and as a consequence is a less prevalent site for tendinopathy than the supraspinatus and the infraspinatus tendons [6]. Despite this, clinicians should be aware of the subscapularis as a potential pain generator in the shoulder region. Ferrick described the presence of subscapularis tendinosis as being a cause for anterior shoulder pain. The author reported subcoracoid impingement as being a possible causal factor in the development of this condition [7].
The use of examination procedures to identify specific tissue involvement in painful conditions is a critical element in musculoskeletal physical therapy practice. Cyriax and Cyriax described an approach to clinical diagnosis based on “selective tension testing”, where by clinicians identify a specific pain generating structure through performance of active, passive and resistive testing [8]. Physical therapists can benefit from this approach to patient examination because it allows them to focus treatments on the causes of symptoms. The purpose of this case report is to describe a systematic approach to examination and treatment of shoulder pain through the identification of specific pain generators.
Case Presentation
History
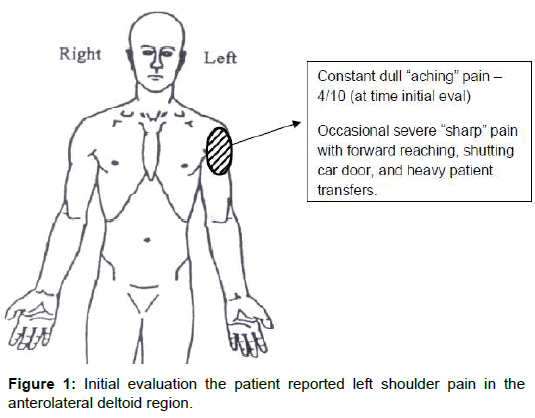
The patient was a thirty six year old female who related the onset of her left shoulder pain to a flu vaccination received five months previously. She was employed as an intensive care unit registered nurse, and was unable to report any other incident of shoulder pain or trauma prior to receiving the flu shot. Her initial physical therapy evaluation took place five months following the initial onset of pain. At the time of initial evaluation the patient reported left shoulder pain in the anterolateral deltoid region (Figure 1) and she described her pain as a dull ache. She rated her pain as being a 4 on a scale of 1-10, with periods of more severe and sharp pain during forward reaching movements. Sharp severe pain was also noticed during shutting her car door and with patient transfers. The patient reported increased pain with work and recreational activities, which included her normal work-out routine. She sought medical attention from her primary care physician because of worsening of her pain symptoms and difficulty with work and recreational activities. Her primary care physician subsequently referred her for physical therapy evaluation and treatment with a diagnosis of right deltoid strain.
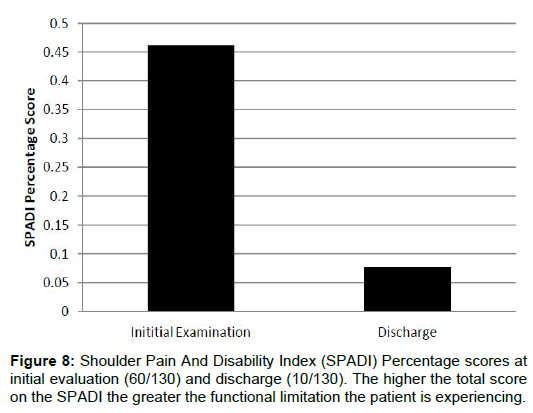
The Shoulder Pain and Disability Index (SPADI) were administered as a part of the intake at the time of the initial evaluation and the patient scored 60 out of 130 points. The higher the total score on the SPADI the greater the functional limitation the patient is experiencing [9].
Examination
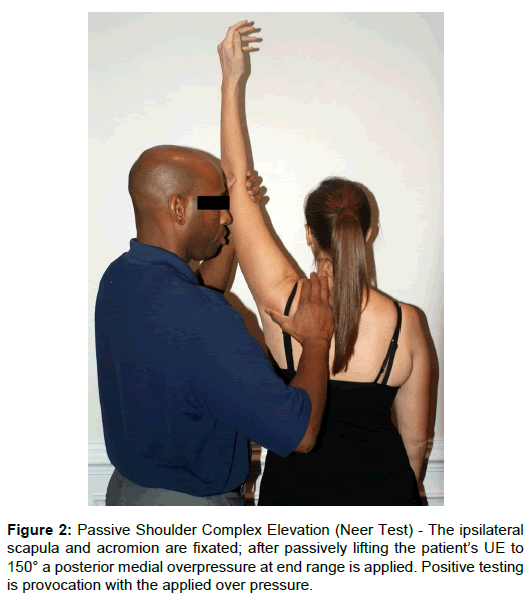
The examination that was performed was based on the tissue specific approach described by Sizer et al. [10]. The findings of the examination were as follows: Cervical spine active range of motion (ROM) was normal and pain free. Active shoulder girdle ROM (elevation, depression, retraction and protraction) was normal and pain free. Shoulder girdle ROM is a combination of movement from scapulothoracic, acromioclavicular and sternoclavicular joints [10]. No abnormal scapular positions or movements were assessed. The patient presented with limited left shoulder complex (glenohumeral joint (GHJ) and shoulder girdle) active elevation 160 degrees left (175 degrees right). Mild left shoulder pain was provoked with this active movement. Passive shoulder complex elevation provoked mild left shoulder pain at end ROM with fixation of the shoulder girdle along with posterior and medial over pressure [10] (Figure 2).
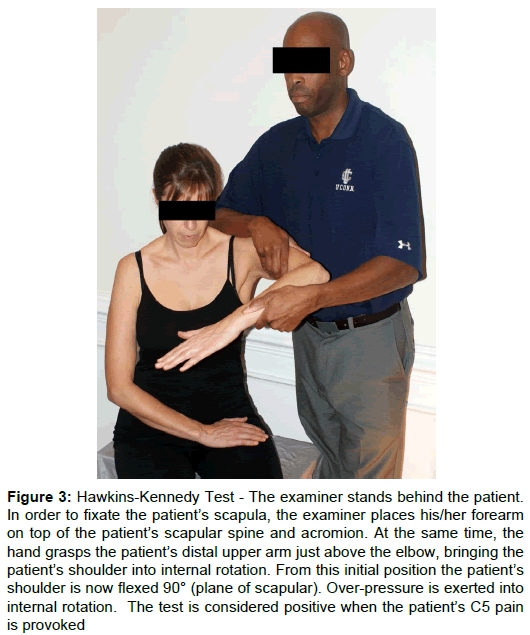
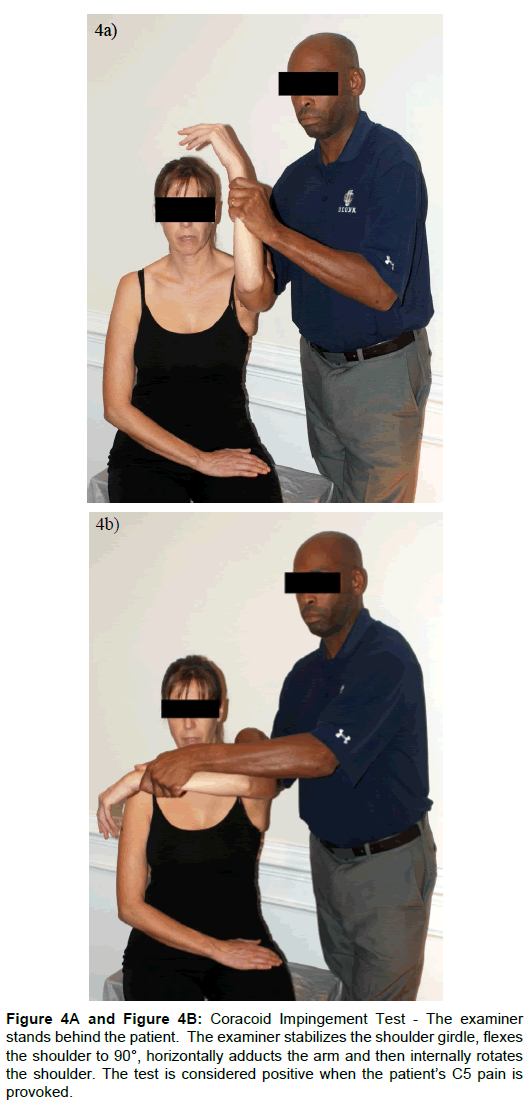
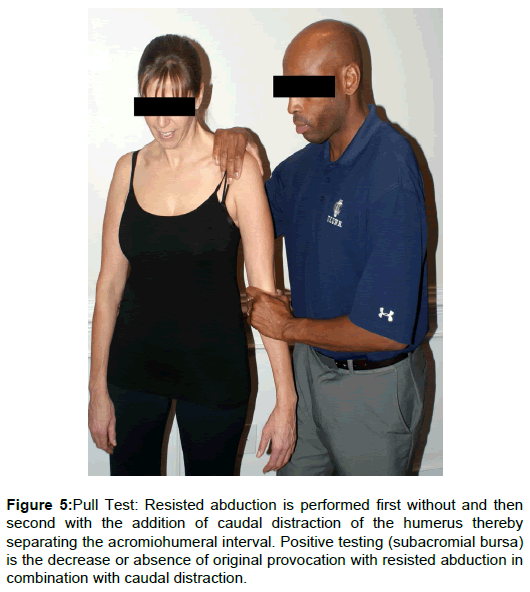
Passive GHJ ROM was as follows: left external rotation was 75° (80° on the right) with mild pain at end ROM; internal rotation and abduction were normal and pain free. Shoulder resistive tests were as follows: left abduction mild pain provocation 4+/5 (4+/5 on the right); left internal rotation moderate pain provocation 4/5 (5/5 on the right); adduction and external rotation were pain free with symmetrical strength (5/5 and 4+/5 respectively). The results of selected special tests were as follows: Mild left shoulder pain provocation with Hawkins-Kennedy test (Figure 3). Severe left shoulder pain provocation with subcoracoid impingement test (Figure 4) [10]. The pull test was performed on the patients left shoulder where by resisted abduction was repeated with the addition of caudal distraction (Figure 5). Previously reported mild pain with resisted left should abduction was eliminated. Winkel et al. theorized that if the resisted abduction is painful without the caudal distraction of the humerus and the pain is subsequently eliminated with caudal distraction (decrease compression in acromiohumeral interval) the subacromial bursa is affected [6].
Figure 3: Hawkins-Kennedy Test - The examiner stands behind the patient. In order to fixate the patient’s scapula, the examiner places his/her forearm on top of the patient’s scapular spine and acromion. At the same time, the hand grasps the patient’s distal upper arm just above the elbow, bringing the patient’s shoulder into internal rotation. From this initial position the patient’s shoulder is now flexed 90° (plane of scapular). Over-pressure is exerted into internal rotation. The test is considered positive when the patient’s C5 pain is provoked.
Figure 5: Pull Test: Resisted abduction is performed first without and then second with the addition of caudal distraction of the humerus thereby separating the acromiohumeral interval. Positive testing (subacromial bursa) is the decrease or absence of original provocation with resisted abduction in combination with caudal distraction.
Evaluation
Based on the patient’s subjective history and examination findings the tissue specific diagnosis was subscapularis tendinopathy with subacromial bursitis. This assessment was based on moderate pain with resisted internal rotation (subscapularis) and severe pain with subcoracoid impingement test. The diagnosis of subacromial bursitis is based on results of the pull test, mild pain during passive end ROM elevation, along with mild pain with Hawkins-Kennedy impingement test [10]. Tables 1 and 2 present a summary of the clinical reasoning process that the therapist utilized to reach the tissue specific diagnostic conclusion.
| Possible Pain Generators Following Subjective History | Objective Examination Findings |
|---|---|
|
Cervical screen normal pain free |
|
Shoulder girdle motions pain free |
|
Shoulder girdle motions pain free |
|
Capsular pattern of limitation for the glenohumeral joint not present |
|
Mild pain with resisted shoulder abduction |
|
No pain with resisted shoulder external rotation |
|
Moderate pain with resisted shoulder internal rotation |
|
No pain with resisted elbow flexion |
|
Mild pain with resisted shoulder abduction |
Table 1: Clinical decision chart of subjective and objective examination.
| Possible Pain Generators Following Objective Examination | Special Test Findings |
|---|---|
|
Positive Hawkins-Kennedy test Pull test – Pain with resisted abduction; no pain with resisted abduction combined with caudal distraction. Supraspinatus ruled out. |
|
Positive Hawkins-Kennedy test Pull test – Pain with resisted abduction; no pain with resisted abduction and caudal distraction. Subacromial bursa ruled in. |
|
Severe pain with sub coracoid impingement test. Subscapularis ruled in. |
Table 2: Clinical decision chart of special tests.
Treatment
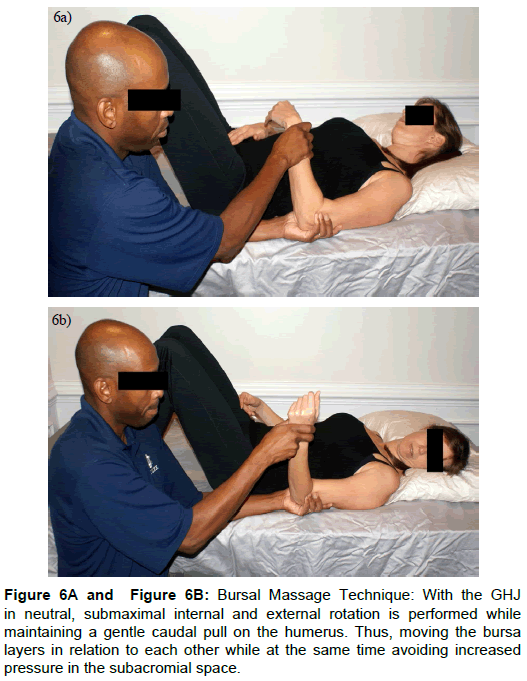
Based on the subjective history and examination findings initial treatment consisted of transverse friction massage to the subscapularis insertion (10- 15 minutes), and manual stretching to the subscapularis as described by Winkel et al., [6]. This was followed by pulsed ultrasound at 1.0 watts per centimeter squared 50% duty cycle for eight minutes to the subscapularis distal insertion. Several authors have suggested that non-thermal ultrasound may have a beneficial effect on collagen synthesis as well as a positive clinical impact [11-13]. Treatment sessions were concluded with bursal massage technique as described by Sizer et al., for management of symptoms related to subacromial bursitis [10] (Figure 6). The patient was given home exercise program consisting of gravity eliminated external and internal rotation for bursa related symptom control. She was also instructed on gentle self-stretching exercises for the left subscapularis. The goals of the initial treatments were to decrease pain as well as promote healing of the subscapularis tendon. Patient was seen three times per week for three weeks. See Table 3 for management summary, describing assessment measures, treatment, and outcomes per session.
Figure 6: Bursal Massage Technique: With the GHJ in neutral, submaximal internal and external rotation is performed while maintaining a gentle caudal pull on the humerus. Thus, moving the bursa layers in relation to each other while at the same time avoiding increased pressure in the subacromial space.
| Week/Visit | Tissue | Assessment Marker | Treatment | Outcome Next Visit |
|---|---|---|---|---|
| Week 1 Visits 1 and 2 |
Subscapularis tendon insertion |
|
|
“A little better”; Pain 4/10; SPADI = 60/130 |
| Subacromial bursa |
|
|
||
| Week 2 Visits 3 - 5 |
Subscapularis tendon insertion |
|
|
“Much better”; Pain 2/10; trace/no pain with resisted abduction (bursa symptoms resolved) |
| Subacromial bursa |
|
|
||
| Week 3 - 4 Visit 6 (re-evaluation) - 11 |
Subscapularis tendon insertion |
|
|
“Fifty percent better”; 1-2/10; Moderate pain with work/lifting activities. |
| Week 5 Visit 12 |
Subscapularis tendon insertion |
|
|
“Seventy-five percent overall improvement”; 1/10 pain with activity |
| Week 7 Visit 13 |
Subscapularis tendon insertion |
|
|
Discharge visit (week 9 visit14) – 0/10 pain at rest; “Minimal pain with busy work shift”; SPADI = 10/130 |
Table 3: Management summary, describing assessment measures, treatment, and outcomes per session.
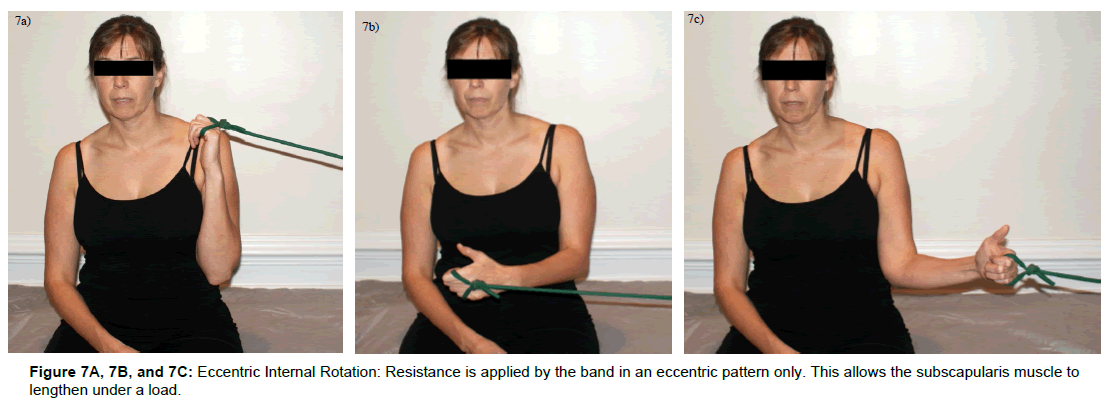
At visit six during week three a re-evaluation was performed. The findings were as follows: full active elevation with no complaints of pain, no pain at end passive elevation ROM, trace pain with resisted abduction (pain abolished with caudal distraction – Pull Test), moderate pain with resisted internal rotation, and severe pain with subcoracoid impingement test. The patient continued to have moderate increased pain with heavy lifting activities such as pulling patients up in bed at work. The impression at this time was that her symptoms related to subacromial bursitis were resolving as a result of bursal massage technique and home exercise program. These techniques were discontinued following visit five week two. Her symptoms related to subscapularis tendinosis were persisting despite a consistent decline in symptoms during the initial five visits (Table 3). At this time transverse friction massage and stretching techniques were continued with the addition of iontophoresis, at the request of her primary care physician. A magnetic resonance imaging (MRI) scan was ordered by her physician as well. The results of the MRI revealed tendinosis of the left subscapularis tendon. Patient continue with treatment three times per week for two weeks making certain that she received six iontophoresis treatments within a period of ten days (Week three – four, visits six – eleven) as recommended by Nirschl et al. [14]. At the conclusion of this two week (week 5 visit twelve) period the patient reported a continued reduction in symptoms reporting 50% overall improvement. Pain with resisted internal rotation was mild but strong 5/5 and subcoracoid impingement test provoked mild symptoms only. The patient’s primary complaint was moderate pain with heavy lifting activities including patient transfers and moving patients in bed. The final treatment intervention for this patient consisted of instruction on eccentric strengthening activities for the subscapularis (Figure 7a, 7b and 7c). The patient was instructed to begin with one set of ten repetitions daily for one week followed by gradual progression to three sets of ten repetitions as tolerated. The patient was informed about the possibility for an initial increase in pain associated with eccentric exercise, but was instructed to continue with exercise regardless. At this time treatment was decreased to follow-up every two weeks. At the time of the first follow up appointment patient had progressed to three sets of ten repetitions and reported 4.5 Pain at 1-2/10 with overall symptom improvement of 75%.
Outcome
At the time of her final follow-up appointment she continued to have trace symptoms with coracoid impingement test, and her resisted internal rotation was 5/5 with trace pain provocation. She had resumed her normal workout activities and stated that she only noticed her shoulder symptoms when she had a particularly busy shift. Her final SPADI score was 10/130. Her overall improvement was 83.3% on the SPADI. See Figure 8 for graphic representation of outcomes. At this time she was discharged from physical therapy with recommendation to continue her exercises on a daily basis.
Discussion
The patient in this case study demonstrated a positive functional outcome and considerable reduction of symptoms with implementation of an evidence based tissue specific treatment approach. Her symptoms associated with subacromial bursitis were resolved within a three week period. This rapid decrease in symptoms is most likely related to treatments which stressed pain relief through mechanoreceptor activation (bursal massage and gravity eliminated external and internal rotation). Her symptoms related to subscapularis tendinosis improved with a combination of transverse friction massage, ultrasound, and iontophoresis. Transverse friction techniques have been shown to have an analgesic affect as well as an ability to enhance fibroblast activity [15,16]. While Nirschl demonstrated the short term pain reliving effects of iontophoresis in the treatment of painful tendons [14]. This patient’s ultimate return to function and resolution of symptoms did not occur until the introduction of eccentric training for the subscapularis. Several studies have demonstrated positive outcomes with the introduction of eccentric training for tendon related pain in the shoulder [17-20]. These studies have all focused on the shoulder abductors, and particularly the supraspinatus muscle. Eccentric training has been theorized to decrease the pain associated with tendinosis as a result of normalization of tendon structure and elimination neovascularization following periods of therapeutic eccentric loading [21]. Eccentric exercise produces high frequency oscillatory loading profiles which are rarely seen during concentric contractions [22,23]. This oscillatory loading has been proposed as a possible biomechanical mechanism to explain the positive clinical results reported with eccentric training in patients with tendinopathy.
Clinical implications
Using a systematic examination process to identify tissue specific pain generators can provide therapists with the framework needed to implement evidence based treatment approach. This is particularly important when considering the multiple possible pain generators that therapist must consider when managing patients with shoulder pain. Therapists who use a consistent systematic approach on all patients have an enhanced ability to self-evaluate and utilize clinical experience with decision making during future patient encounters.
This case is an example of a successful treatment program for a patient with multiple pain generators in the shoulder that began with a systematic tissue specific examination process. The examination process allowed the therapist to direct his evidence based interventions at specific tissues while ruling out other none involved structures. Patient encounters that are not based on a systematic tissue specific approach to examination may result in unnecessary interventions and prolonged overall treatment time for patients.
Keypoints
▪ Multiple pain generators in the shoulder create a challenge for clinicians.
▪ A tissue specific examination is beneficial for evaluating patients.
▪ Interventions directed at specific structures can enhance patient outcomes.
Conflict of Interest
There were no conflicts of interest in the production of this manuscript.
References
- Glockner SM (1995) Shoulder pain: a diagnostic dilemma. Am Fam Physician51: 1677-1687, 1690-1672.
- Chastang JF, Niedhammer I, Landre MF, Roquelaure Y, Leclerc A (2004) Incidence of shoulder pain in repetitive work. Occup Environ Med 61: 39-44.
- Browning DG, Desai MM (2004) Rotator cuff injuries and treatment. Prim Care31: 807-829.
- Mehta S, Gimbel JA, Soslowsky LJ (2003) Etiologic and pathogenetic factors for rotator cuff tendinopathy. Clin Sports Med22: 791-812.
- Sizer PS, Phelps V, Gilbert KK (2003a) Diagnosis and Management of the Painful Shoulder. Part 1: Clinical Anatomy and Pathomechanics. Pain Practice3: 39-57.
- Winkel D, Matthijs O, Phelps V, Vleeming A (1997) Diagnosis and Treatment of the Upper Extremities: Non Operative Orthopaedic Medicine and Manual Therapy: Aspen Pub, Gaithersburg, Maryland.
- Ferrick MR (2000) Coracoid impingement. A case report and review of the literature. Am J Sports Med28: 117-119.
- Cyriax J, Cyriax R (1993). Illustrated Manual of Orthopaedic Medicine. Butterworths, London.
- Williams JW, Holleman DR, Simel DL (1995) Measuring shoulder function with the Shoulder Pain and Disability Index. J Rheumatol22: 727-732.
- Sizer PS, Phelps V, Gilbert KK (2003b) Diagnosis and management of the painful shoulder. Part 2: Examination, Interpretation, and Management.Pain Practice3: 152-185.
- Baker KG, Robertson VJ, Duck FA (2001) A Review of Therapeutic ultrasound: biophysical effects. Phys Ther 81: 1351-1358.
- Khan K, Cook J (2003) The painful nonruptured tendon: clinical aspects. Clin Sports Med 22: 711-725.
- Gursel YK, Ulus Y, Bilgic A, Dincer G, Van der Heijden GJ (2004) Adding Ultrasound in the Management of Soft Tissue Disorders of the Shoulder: a Randomized Placebo-Controlled Trial. Phys Ther84: 336-343.
- Nirschl RP, Rodin DM, Ochiai DH, Maartmann-Moe C (2003) Iontophoretic administration of dexamethasone sodium phosphate for acute epicondylitis. a randomized, double-blinded, placebo-Controlled study. Am J Sports Med 31: 189-195.
- De Bruijn R (1984) Deep Transverse friction; it's analgesic effect. Int J Sports Med5: 35-36.
- Gehlson GM, Ganion LR, Helfst R (1999) Fibroblast responses to variation in soft tissue mobilization pressure. Med Sci Sports Exerc 31: 531-535.
- Bernhardsson S, Klintberg IH, Wendt GK (2010) Evaluation of an exercise concept focusing on eccentric strength training of the rotator cuff for patients with subacromial impingement syndrome. Clin Rehabil25: 69-78.
- Camargo PR, Avila MA, Alburquerque-Sendin F, Asso NA, Hashimoto LH, et al. (2012) Eccentric training for shoulder abductors improves pain, function and isokinetic performance in subjects with shoulder impingement syndrome: a case series. Rev bras fisioter 16: 74-83.
- Jonsson P, Wahlstrom P, Ohberg L, Alfredson H (2006) Eccentric training in chronic painful impingement syndrome of the shoulder: results of a pilot study. Knee Surg Sports Traumatol Arthrosc14: 76-81.
- Maenhout AG, Mahieu NN, De Muynck M, De Wilde LF, Cools AM (2013) Does adding heavy load eccentric training to rehabilitation of patients with unilateral subacromial impingement result in better outcome? A randomized, clinical trial. Knee Surg Sports Traumatol Arthrosc21: 1158-1167.
- Ohberg L, Lorentzon R, Alfredson H (2001) Neovascularisation in achilles tendons with painful tendinosis but not in normal tendons: an ultrasonographic investigation. Knee Surg Sports Traumatol Arthrosc9: 233-238.
- Rees JD, Lichtwark GA, Wolman RL, Wilson AM (2008) The mechanism for efficacy of eccentric loading in Achilles tendon injury; an in vivo study in humans. Rheumatology47: 1493-1497.
- Rees JD, Wolman RL, Wilson A (2009) Eccentric exercises; why do they work, what are the problems and how can we improve them? Br J Sports Med43: 242-246.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi