Case Report, Int J Ophthalmic Pathol Vol: 12 Issue: 5
Management of an Invasive Squamous Cell Carcinoma of the Conjunctiva: A Case Report
Jamuna Gurung1, Rohit Saiju2, Malita Amatya2, Hom Bahadur Gurung2 and Purnima Rajkarnikar Sthapit2*
1Department of Ophthalmology, Gandaki Medical College Teaching Hospital, Nayabazar Rd, Pokhara 33700, Nepal
2Department of Oculoplasty and Ocular Oncology, Tilganga Institute of Ophthalmology, Ring Rd, Kathmandu 44600, Nepal
*Corresponding Author: Purnima Rajkarnikar Sthapit,
Department of Oculoplasty
and Ocular Oncology, Tilganga Institute of Ophthalmology, Ring Rd, Kathmandu
44600, Nepal
Tel: +9779860314317
E-mail: purnimark@gmail.com
Received date: 24 September, 2023, Manuscript No. IOPJ-23-114651;
Editor assigned date: 27 September, 2023, PreQC No. IOPJ-23-114651 (PQ);
Reviewed date: 11 October, 2023, QC No. IOPJ-23-114651;
Revised date: 18 October, 2023, Manuscript No. IOPJ-23-114651 (R);
Published date: 25 October, 2023, DOI: 10.4172/2324-8599.12.5.040
Citation: Gurung J, Saiju R, Amatya M, Gurung HB, Sthapit PR (2023) Management of an Invasive Squamous Cell Carcinoma of the Conjunctiva: A Case Report. Int J Ophthalmic Pathol 12:5.
Abstract
To describe the clinical findings and management of a patient with invasive Squamous Cell Carcinoma (SCC).
We present the case of a patient with a conjunctival mass with progressive growth in the right eye and decreased visual acuity. He had undergone excision of a limbal conjunctival mass one month before this condition. Examination revealed a fleshy conjunctival lesion on the temporal limbus that extended intraocularly. An irregular gray mass measuring 3 x 2 mm in size was observed in the anterior chamber. Modified enucleation with the implant was performed to control local invasion. Histopathological analysis showed recurrent conjunctival SCC, well-differentiated, tumors infiltrating the sclera, choroid and ciliary body, Tumour Node Metastasis (TNM) (American Joint Committee on Cancer classification) stage: pT3Nx. The patient was treated with adjuvant chemotherapy post-operatively.
Conclusion: Invasive squamous cell carcinoma of the conjunctiva is a rare condition. The management of a locally advanced tumor is enucleation and disease-free resection should be performed as this will impact the patient's prognosis and survival time.
Keywords: Enucleation; Histopathology; Invasive squamous cell carcinoma.
Introduction
Ocular Surface Squamous Neoplasm (OSSN) is a group of disorders ranging from dysplasia to invasive Squamous Cell Carcinoma (SCC). SCC is the most common tumor on the ocular surface [1,2]. The average incidence of OSSN ranges from 0.13/100,000 to 3.5/100,000 population. The risk factors include exposure to ultraviolet rays and human papillomavirus infection [3-6].
Intraocular invasion of conjunctival SCC has been reported in 2%-8% of cases [7,8]. Involvement of the deep corneal stroma and anterior chamber structures suggests intraocular invasion. Intraocular invasion of SCC can have a prior history of tumor excision. To prevent recurrences, suspicious limbal tumors should be managed by localized alcohol epithelialized corneal epitheliectomy, tumor removal by lamellar scleroconjunctivectomy and double freeze-thaw cryotherapy. Invasive SCC can be both sight and life-threatening when the tumor is spread into intraocular and orbital structures [9]. It is managed by plaque brachytherapy, modified enucleation, or orbital exenteration depending on the extent of the tumor [10].
Invasive SCC of the conjunctiva is uncommon with only a few cases reported in Nepal. Here, we report a case of intraocular invasion of conjunctival SCC and discuss its clinical presentation and management.
Case Presentation
A 54-year-old male underwent excision of a limbal conjunctival tumor on the right eye on 17th June 2022. He presented with a pinkish elevated mass on the temporal bulbar conjunctiva with pain and watering in his right eye one month after surgery. This lesion was misdiagnosed as granuloma and treated with anti-inflammatory drugs. The histopathology reported lately with invasive SCC. The patient was then referred to the Tilganga Institute of Ophthalmology.
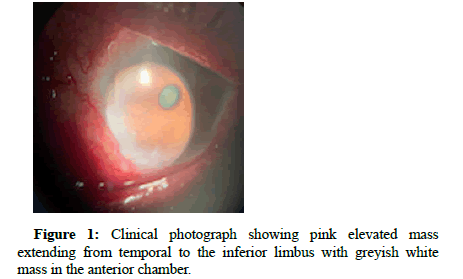
The patient presented with a mass in the right bulbar conjunctiva which was progressively increasing in size associated with pain and diminution of vision. The visual acuity was 6/18 in the right eye and 6/6 in the left eye. Slit lamp examination revealed a fleshy, highly vascularized conjunctival lesion affecting the temporal and inferior bulbar conjunctiva along with limbal conjunctiva between 6’o clock to 9’o clock positions (Figure 1). An irregular grey mass measuring 3 x 2 mm in size was seen in the inferotemporal direction of the anterior chamber. The iris, pupil, lens and posterior segment examination was normal and the regional lymph nodes were not palpable.
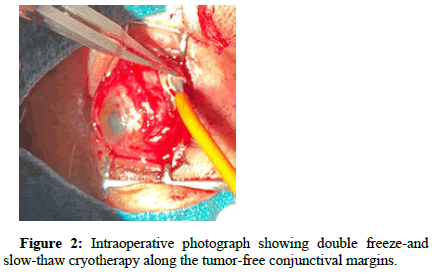
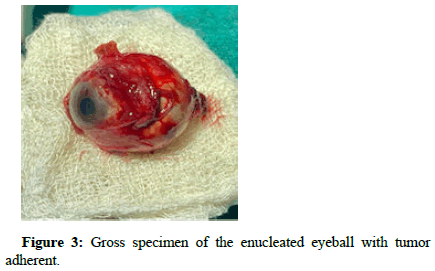
Considering the intraocular invasion, modified enucleation with the implant was performed. The conjunctival peritomy was performed keeping a 4 mm conjunctival margin free from the tumor-affected tissue. The tumor remained adherent to the globe at the limbus. The remaining steps of enucleation were done and the globe was removed with tumor adherent after cutting from the optic nerve. The margins of the remaining unaffected conjunctiva were treated with double freeze-and slow-thaw cryotherapy (Figure 2). Post-operatively, Post-operatively, the patient completed 4 cycles of 5-Fluorouracil 1%, given for remaining conjunctiva. The socket is healthy and no recurrence till date.
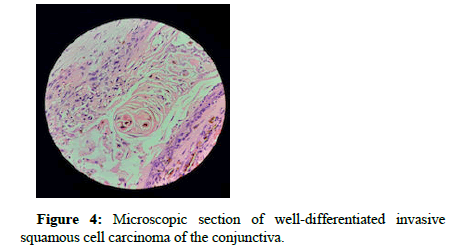
The sectioned globe showed a dark brown-colored conjunctival mass adjacent to the cornea which measures 2 x 1.5 cm (Figure 3). Histopathologically, the tumor is composed of a nest and cords of atypical squamous cells infiltrating the sclera, choroid and ciliary body. The cornea is focally invaded by the tumor. These nests show stratification, intercellular bridges, keratin pearls and moderate cellular pleomorphism. Mitotic figures were numerous and showed frequent atypia. The conjunctival margin, retina and optic nerve were free of tumors. Lymphatic, vascular and perineural invasion was not seen (Figure 4). It was graded as TNM (American Joint Committee on Cancer classification) stage: pT3Nx.
Results and Discussion
Conjunctival SCC has a high recurrence rate even after complete excision of the primary tumor. The risk of invasion into intraocular structures is more when there is limbal or scleral involvement. Conjunctival intraepithelial or invasive neoplasia is associated with a 24%-50% recurrence rate after simple excision [7,8,11]. In our case, an excisional biopsy of a limbal lesion recurred with the rapid growth of the tumor with intraocular invasion in a one-month follow-up. Intraocular involvement probably occurs through the numerous drainage and nerve channels or the canal left by trauma and surgery [12]. The scleral defect caused during the patient's first conjunctival excision or through the limbal tissues can be the source of the extension of tumors into intraocular structures in our case.
Enucleation is performed in eyes with intraocular invasive SCC and exenteration is when there is an orbital extension. Whereas, Char et al., performed successful resection of the sclera along with contiguous iris, ciliary body and choroid en bloc with adjunctive cryotherapy locally in a patient where the intraocular component was circumscribed, thus avoiding enucleation. There was no recurrence after almost 10 years [13]. Plaque brachytherapy using strontium-90 or ruthenium-106 reported nearly 100% success rates in cases with superficial conjunctival SCC. However, it has been reserved for patients with diffuse tumors incompletely resected and those with multiple recurrences [14]. In Kearsley and associates, 140 invasive cases were treated with strontium-90 radiotherapy with a recurrence rate of 2.3% with minimal complications [15]. In the clinical context of Nepal; we lack this mode of treatment. So, we performed modified enucleation which was followed by adjuvant chemotherapy.
Conclusion
Squamous cell carcinoma can be sight-threatening when it spreads intraocular and intraorbital structures. Management of SCC requires the standard no-touch surgical technique combined with an adjuvant therapy strategy. Despite optimal treatment, there can be recurrences. So, long-term close follow-up is essential. Management of recurrent tumors is challenging when there are limited resources.
This case highlights the clinical importance of accurate diagnosis and meticulous surgery. There should be a detailed histopathology examination and appropriate adjuvant therapy to prevent sightthreatening complications.
Informed consent
Written informed consent was taken from the patient for publication of this case report.
References
- Nanji AA, Mercado C, Galor A, Dubovy S, Karp CL (2017) Updates in ocular surface tumor diagnostics. Int Ophthalmol Clin 57:47-62.
- Shields CL, Demirci H, Karatza E, Shields JA (2004) Clinical survey of 1643 melanocytic and nonmelanocytic conjunctival tumors. Ophthalmology 111:1747-1754.
- Darwich R, Ghazawi FM, Le M, Rahme E, Alghazawi N, et al. (2020) Epidemiology of invasive ocular surface squamous neoplasia in Canada during 1992-2010. Br J Ophthalmol 104:1368-1372.
- Lee GA, Hirst LW (1992) Incidence of ocular surface epithelial dysplasia in metropolitan Brisbane: A 10-year survey. Arch Ophthalmol 119:525-527.
- Sun EC, Fears TR, Goedert JJ (1997) Epidemiology of squamous cell conjunctival cancer. Cancer Epidemiol Biomarkers Prev 6:73-77.
- Honavar SG, Manjandavida FP (2015) Tumors of the ocular surface: A review. Indian J Ophthalmol 63:187-203.
- Lee GA, Hirst LW (1995) Ocular surface squamous neoplasia. Surv Ophthalmol 39:429-449.
- Iliff WJ, Marback R, Green R (1975) Invasive squamous cell carcinoma of the conjunctiva. Arch Ophthalmol 93:119-112.
- Santoni A, Thariat J, Maschi C, Herault J, Baillif S, et al. (2019) Management of invasive squamous cell carcinomas of the conjunctiva. Am J Ophthalmol 200:1-9.
- Shields CL, Shields JA (2019) Tumors of the conjunctiva and cornea. Indian J Ophthalmol 67:1930-1948.
- Tabin G, Levin S, Snibson G, Loughnan M, Taylor H (1997) Late recurrences and the necessity for long-term follow-up in corneal and conjunctival intraepithelial neoplasia. Ophthalmology 104:485-492.
- Zhang Z, Li B, Shi J, Xu X, Li L, et al. (2007) Intraocular extension of conjunctival squamous cell carcinoma. Ophthalmologica 221:200-203.
- Char DH, Crawford JB, Howes EL Jr, Weinstein AJ (1992) Resection of intraocular squamous cell carcinoma. Br J Ophthalmol 76:123-125.
- Zehetmayer M, Menapace R, Kulnig W (1993) Combined local excision and brachytherapy with ruthenium-106 in the treatment of epibulbar malignancies. Ophthalmologica 207:133-139.
- Kearsley JH, Fitchew RS, Taylor RG (1988) Adjunctive radiotherapy with strontium-90 in the treatment of conjunctival squamous cell carcinoma. Int J Radiat Oncol Biol Phys 14:435-443.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi