Research Article, J Virol Antivir Res Vol: 8 Issue: 1
Molecular Detection of Human Papilloma Virus Infection of Uterine Cervix among Women of Reproductive Age
Misbah Noor*, Eijaz Ghani, Saifullah Khan Niazi and Muhammad Tahir Khadim
Armed Forces Institute of Pathology, Rawalpindi, Pakistan
*Corresponding Author : Misbah Noor
Armed Forces Institute of Pathology, Rawalpindi, Pakistan
Tel: 923335212723
E-mail: misbahnoor001@gmail.com
Received: 03 December 2018 Accepted: 04 January 2019 Published: 11 January 2019
Citation: Noor M, Ghani E, Niazi SK, Khadim MT (2019) Molecular Detection of Human Papilloma Virus Infection of Uterine Cervix among Women of Reproductive Age. J Virol Antivir Res 8:1. doi: 10.4172/2324-8955.1000189
Abstract
Objective: The objective of this study was to determine frequency of human papilloma virus infection of uterine cervix among women of reproductive age by polymerase chain reaction.
Study Design and Duration: It was a cross sectional study of six months duration.
Methodology: 162 samples of exfoliated cervical cells were collected with cervical sampler; during gynecological examination. The tip containing cellular material was placed into PreservCyt bottle with collection medium, stored at 4°C and then transported to Virology department of AFIP for real time PCR.
Results: The frequency of human papilloma virus infection of uterine cervix among women of reproductive age by polymerase chain reaction was 2.47% (n=4). Mean age of participants was 33.2 ± 6.4 years. Mean age at 1st pregnancy was 23 ± 3.3 years while mean number of children was 3 ± 1.4. 87.7% of participants husband had one wife and 4.9% participants husband had more than one wives. 89.5% never used OCP while 5.6% were former and 4.9% were current users. 89% of participants never smoked, 9% were former smoker and 2% were current smokers. Among positive cases, three patients had HR-HPV 16 and one had a rare HR-HPV 51/59 infection.
Conclusion: The frequency of human papilloma virus infection of uterine cervix was not very high among women of reproductive in our setup. However, it was a single center study which may not reflect the frequency of the whole city as data from other hospitals was not included in the study. All four positive cases belong to >36 years age group. The positive women in our study had birth of their first child between 15-20 years of age (P=0.001 CI=95%) and also they had high parity (P=0.013 CI=95%). All the four positive women were apparently healthy, so screening must be recommended for sexually active women in our country. A nationwide study must be carried out for formulation of screening and vaccination strategies for future.
Keywords: Reproductive age; human papilloma virus infection; uterine cervix; polymerase chain reaction
Introduction
Human Papillomaviruses (HPVs) are non-enveloped doublestranded DNA viruses with more than 100 genotypes. According to International Agency for Research on Cancer working group, HPV-16, -18, -31, -33, -35, -39, -45, -51, -52, -56,-58, and -59 have been classified as “carcinogenic to humans” [1]. It is sexually transmitted virus causing mostly asymptomatic infections that clear spontaneously within a period of about 12 to 36 months [2]. If HPV infection becomes persistent, it can result in clinical disease in the form cervical dysplasia, cervical intraepithelial neoplasia and cervical carcinoma. High risk HPV types 16 and 18 are responsible for around 70% of all cervical malignancy cases around the world. Cervical cancer is a vaccine preventable cancer. As virus is transmitted via sexual route, so vaccination before the start of sexual activity decreases cervical cancer risk [3].
In women, cervical tumor has been perceived as the third most common cancer around the globe and it is the fourth most prevalent source of cancer related death around the world with 85% of these cases and deaths occur in developing countries. Papanicolaou (Pap) smear screening has assumed a noteworthy part in the finding of premalignant and malignant lesions in the cervix and has diminished the related death rate in nations that have a vigorous screening system set up, however such screening projects in developing nations are constrained or non-existent [4]. The most productive and practical screening method in low-resource nations incorporate testing HPV DNA in cervical cell samples [5]. A recent clinical trial in rural India found that a single round of HPV DNA testing was connected with around a half decrease in the risk of developing cervical cancer and related deaths [6].
According to a study conducted in India the prevalence of Human Papilloma Virus was 11.9% based on PCR [3]. Another study conducted in Karachi, Pakistan showed 2.8% prevalence of HPV in the general population with no evidence of higher HPV prevalence in young women [7]. The most noteworthy illness burden is found in nations with the poorest framework for cervical tumor screening and treatment. To diminish the weight of sickness in less developed nations where Pap smear screening projects are not promptly available, other cervical tumor anticipation techniques are required. These methodologies incorporate HPV testing by PCR as an essential screening tool and control of cofactors connected with sickness [8].
The purpose of this study is to estimate frequency of human papilloma virus infection of uterine cervix among women of reproductive age by polymerase chain reaction. This would help in early detection of patients at risk of developing cervical cancer so that prevention and treatment may be started early to avoid the long term consequences.
Methodology
162 non pregnant sexually active women of reproductive age (15-49 years as defined by WHO) [9] were included in the study (sample size calculated using WHO sample size calculator) while women already diagnosed with cervical diseases were excluded from the study.
Cervical specimens of exfoliated cervical cells were collected with cervical sampler; during gynecological examinations from women visiting gynecological OPD Military hospital, Rawalpindi who fulfilled inclusion criteria. The cervical sampler is inserted 1-1.5 cm into the endocervical canal and rotating 3-5 full turns in counterclockwise direction. The tip containing cellular material was then placed into PreservCyt container containing collection medium and then transported to Virology department, AFIP. The samples were stored at temperature of 2°C to 8°C and tested in batches of 25 samples. The samples were first vortexed for 30 sec then centrifuged for 5 min at 3500 rpm. 1 ml of sample is taken from the bottom of sample container and placed in HPV GeneXpert cartiridge. Real time HPV (Human Papilloma Virus) PCR (Polymerase Chain Reaction) was done on Genexpert (Cepheid, USA). GeneXpert has five channels for detection of various high risk genotypes of HPV. P1 for HPV 16, P2 for HPV 18/45, P3 for HPV 31/33/35/52/58, P4 for HPV 51/59 and P5 for HPV 39/56/66/68.
All data was entered and analyzed using SPSS version 21. Descriptive statistics were used to analyze and describe data. Frequency and percentage was calculated for categorical (qualitative) variables like smoking status, marital status, oral contraceptive use, human papilloma virus detection (yes/no) and genotype detected. Mean and Standard Deviation (SD) were calculated for numerical (quantitative) variables like age, parity and age at first pregnancy. Chi square test was applied to find out statistical significance that was considered at p<0.05.
Results
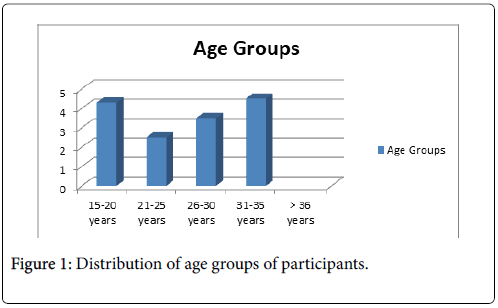
A total of 162 cervical samples from patients meeting inclusion criteria were analyzed during study period. Participant’s age ranged from 20-47 years, mean age was 33.3 ± 6.4 years. Mean number of participant’s children was 3±1.4 and mean age at first pregnancy was 23 ± 3.3 years. 12 (7.4%) participants were in age group 21-25 years, 53(32.7%) were in age group 26-30 years, 42 (29.5%) were in age group 31-35 years, while 54(33.3%) participants were in age group>36 years as shown in (Figure 1).
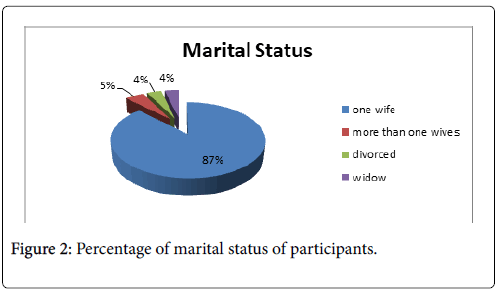
142 (87.7%) of participant’s husband had one wife, 8 (4.9%) had more than one wives, 6 (3.7%) were divorced and 6 (3.7%) were widowed (Figure 2).
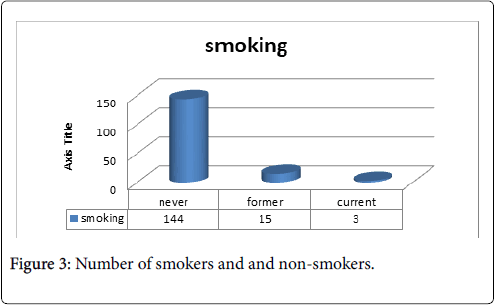
Among 162 participants, 144 (89%) never smoked, 15 (9%) were former smoker while 3 (2%) were currently smoking (Figure 3).
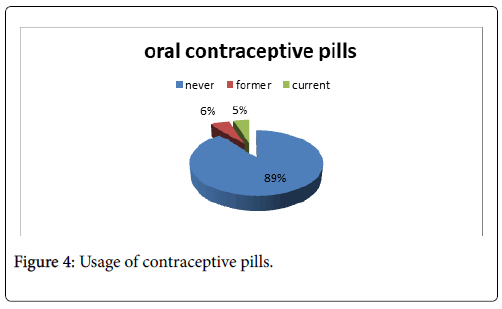
145 (89.5%) of participants never used oral contraceptive pills, 9 (5.6%) former users while 8 (4.9%) were currently using it (Figure 4).
Human Papilloma virus was detected in 4 (2.47%) patients among 162 samples analyzed. All of the four women were above 36 years of age. 3 (1.8%) patients were positive for HPV genotype 16 and 1 (0.62%) were positive for HPV 51/59. All the four positive women were between 15-20 years of age at time of birth of their first child. Chi square test also shows significant association of age at first pregnancy with HPV detection p value=0.001(CI=95%) (Table 1).
| Age at first pregnancy | HPV Detected | Total | P value | |
|---|---|---|---|---|
| Yes | No | |||
| 15-20 years | 4 | 28 | 32 | 0.001 |
| 21-25 years | 0 | 90 | 90 | |
| 26-30 years | 0 | 36 | 36 | |
| >31 years | 0 | 4 | 4 | |
| Total | 4 | 158 | 162 | |
Table 1: Association of first pregnancy with HPV detection, p value=0.001.
Number of pregnancies also have significant correlation with HPV detection as p value=0.013 (CI=95%) as shown in Table 2.
| Parity groups | HPV detected | Total | P value | |
|---|---|---|---|---|
| Yes | No | |||
| 1-3 childrens | 1 | 116 | 117 | 0.013 |
| 4-6 childrens | 2 | 38 | 40 | |
| >6 childrens | 1 | 4 | 5 | |
| Total | 4 | 158 | 162 | |
Table 2: Number of children detected with HPV, p value=0.013.
Discussion
Cervical cancer is third most common cancer in women around the word with more than 85% cases being reported from developing world. We compare our results with a study conducted in India where the prevalence of Human Papilloma Virus was 11.9% based on PCR [3]. These findings were higher than our results. The difference might be due social and religious constrains. Contrary to this a local study conducted in Karachi, Pakistan showed 2.8% prevalence of Human Papilloma Virus in the general population with no evidence of higher HPV prevalence in young women [7]. These results were comparable with our study.
In a small cross sectional study carried out in Northern Iran among 98 healthy women HR-HPV was found in only 4.08% which is comparable to our study. Most of the infected women in study were 26-39 years old [10]. Likewise, in our study all four positive women were>36 years of age. In a large population based survey carried on 2453 Iranian women referred for routine cervical cancer screening the overall HPV prevalence was 10.3%with 3% cases of HPV 16. According to this study the increase in HPV prevalence in Iran might be due to change in sexual behavior and increase use of tobacco among teenagers and youngsters. Also vaccination against HPV is not routinely available in the country [11].
Zahao et al. showed a HR-HPV prevalence of 15.1% in their population with most common genotype being HPV 16 followed by HPV 68 [12]. This is also comparable to our study as our predominant genotype was HPV 16.
Another local study conducted by Abdullah et al. [13] showed 3.26% prevalence of HR-HPV among 92 women tested which is comparable to our study. In this study, 2 samples were positive for HPV 16 while 1 sample was positive for HPV 18. While in our study out of 162 samples tested 3 were positive for HPV 16 while 1 was positive for rare HPV high risk genotype 51/59. None of the sample was positive for HPV 18. In a regional population based survey by Nahar et al. [14] on women aged 13-64 years overall HR-HPV prevalence was 7.7% which is higher as compared to our study.
As HPV infection is asymptomatic, it is unlikely that participation was highly correlated to HPV positivity. However, hesitancy to undergo gynaecological examination may be a strong obstacle to any future cervical cancer screening efforts in Pakistan [15]. Furthermore; vaginal examination is acceptable only to married women, as in similar surveys in Asia [16-18].
In Pakistan low HPV prevalence might be due to strong religious and cultural constraints with incidence of cervical carcinoma in female population much lower than breast and ovarian cancers. However, with sexual behaviors and attitudes of young people it may not hold true in future [19]. Implementation of routine cervical cancer vaccination can prevent our country from the future epidemic. The combined cost of screening and treatment of HPV induced cervical disease gives us a greater incentive to promote use of vaccine so as to reduce economic burden on country’s health system [20].
The low HPV prevalence in our study is consistent with the low ICC risk estimate from Karachi (7.5/100 000 cases annually; rarer than the breast, mouth, ovary and oesophagus) and other predominantly Muslim countries in Asia and, reassuringly, there is no evidence that HPV prevalence is higher in our population [21]. The findings of our study are helpful in early detection of patients at risk of developing cervical cancer, so that prevention and treatment may be started early to avoid the long term consequences. This study provided current local magnitude of HPV infection in women in our hospital only.
Limitations of our study
It is a single center study and we did not included data from other hospitals of the area, however, in future, the study may be extended to include other hospitals as well. The tests are analyzed on GeneXpert which had single primer for HPV 16 but other high risk types are grouped together as HPV 18/45 and group P3 (31,33,35,52 and 58), P4 (51 and 59) and P5 (39,56, 66, and 68). So, we were not able to separately find out the prevalence of all HR-HPV genotypes. Also, we have done only HPV PCR on cervical specimen and cytological examination of these specimens was not done.
Conclusion
The frequency of human papilloma virus infection of uterine cervix is not very high among women of reproductive age by polymerase chain reaction; however, it was a single center study which may not reflect the frequency of the whole city as data from other hospitals were not included in the study. All four positive cases belong to>36 years age group. The positive women in our study had birth of their first child between 15-20 years of age (P=0.001 CI=95%) and also they had high parity (P=0.013 CI=95%). All the four positive women were apparently healthy, so screening must be recommended for sexually active women in our country. A nationwide study must be carried out for formulation of vaccination strategy for future.
References
- Ye J, Cheng X, Chen X, Ye F, Lu W, et al. (2010) Prevalence and risk profile of cervical human papillomavirus infection in Zhejiang Province, southeast China: A population-based study. Virol J 7: 66.
- Siddiqa A, Zainab M, Qadri I, Bhatti M, Parish J (2014) Prevalence and genotyping of high risk human papillomavirus in cervical cancer samples from Punjab, Pakistan. Viruses 6: 2762-2777.
- Sarma U, Mahanta J, Borkakoty B, Sarmah B (2015) Distribution of human papilloma virus infections of uterine cervix among women of reproductive age: A Cross sectional hospital-based study from North East India. Asian Pac J Cancer Prev 16: 1519-1523.
- Jemal A, Bray F, Center M, Ferlay J, Ward E, et al. (2011) Global cancer statistics. CA Cancer J Clin 61: 69-90.
- Sherris J, Wittet S, Kleine A (2009) Evidence-based, alternative cervical cancer screening approaches in low-resource settings. IntPerspect Sex Reprod Health 35: 147-154.
- Sankaranarayanan R, Nene BM, Shastri SS (2009) HPV screening for cervical cancer in rural India. N Engl J Med 360: 1385-1394.
- Raza S, Franceschi S, Pallardy S, Malik F, Avan B, et al. (2010) Human papilloma virus infection in women with and without cervical cancer in Karachi, Pakistan. Br J Cancer 102: 1657-1660.
- Giuliano A, Harris R, Sedjo R, Baldwin S, Roe D, et al. (2002) Incidence, prevalence, and clearance of type specific human papillomavirus infections: The young women’s health study. J Infect Dis 186: 462-469.
- WHO (2015) Infertility definitions and terminology, Bangaledesh.
- Mehran SMM, Ghanaei MM, Mojtehadi A (2015) The prevalence of human papilloma Virus (HPV) in women using liquid base pap smear in Rasht, Northern of Iran. JCDR 9: 1-2.
- Jamdar F, Farzaneh F, Navidpour F, Younesi S, Balvayeh P, et al. (2018) Prevalence of human papillomavirus infection among Iranian women using COBAS HPV DNA testing. Infect Agent Cancer 13: 6.
- Zhao Y, Wu K, Tong H, Liu Y, Zha H, et al. (2018) Genotype patterns and prevalence of human papilloma virus in non-vaccinated women in Zunyi, China. Saudi Med J 39: 572-578.
- Adullah A, Qasim M, Shafiq M, Ijaz M, Parveen S, et al. (2016) Molecular diagnosis and phylogenetic analysis of human papilloma virus type-16 from suspected patients in Pakistan. Infect Agent Cancer 11: 1.
- Nahar Q, Sultana F, Alam A, Islam JY, Rahman M, et al. (2014) Genital human papillomavirus infection among women in Bangladesh: Findings fROM A POPULAtion-BASED SUrvey. PLoS ONE 9: e107675.
- Imam SZ, Rehman F, Zeeshan MM, Maqsood B, Asrar S, et al. (2008) Perceptions and practices of a Pakistani population regarding cervical cancer screening. Asian Pac J Cancer Prev 9: 42-44.
- Franceschi S, Herrero R, Clifford GM, Snijders PJ, Arslan A (2006) The IARC HPV prevalence surveys study group variations in the age-specific curves of human papillomavirus prevalence in women worldwide. Int J Cancer 119: 2677-2684.
- Dai M, Bao YP, Li N, Clifford GM, Vaccarella S, et al. (2006) Human papillomavirus infection in Shanxi Province, People's Republic of China: A population-based study. Br J Cancer 95: 96-101.
- Sherpa ATL, Clifford G, Vaccarella S, Shrestha S, Nygård N, et al. (2010) Human papillomavirus infection in women with and without cervical cancer in Nepal. Cancer Causes Control 21: 313-330.
- Jawaid A (2008) Cervical cancer vaccine in Pakistan: Let's start thinking. Int J Infect Dis 12: 217.
- Yousuf S, Syed S (2009) Prophylactic and therapeutic human papillomavirus vaccine: a breakthrough for women health. J Pak Med Assoc 59: 310-314.
- Curado MP, Edwards B, Shin HR, Storm H, Ferlay J, et al. (2007) Cancer Incidence in Five Continents 2007. International Agency for Research on Cancer, Lyon.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi