Case Report, Int J Ophthalmic Pathol Vol: 8 Issue: 1
Non-Neural Granular Cell Tumor of the Eyelid: Case Report with Immunohistochemical and Ultrastructural Correlation
Joseph G Mathew*, Michael Carvalho, Ihab El-Shinnawy and Samih Salama
Department of Pathology and Molecular Medicine, McMaster University/St. Joseph’s Hospital, Hamilton Regional Laboratory Medicine Program, Hamilton, Ontario, Canada
*Corresponding Author : Dr. Joseph G Mathew
Department of Pathology and Molecular Medicine, McMaster University/St. Joseph’s Hospital, Hamilton Regional Laboratory Medicine Program, Hamilton, Ontario, Canada
Tel: +1 905 525 9140
E-mail: joseph.mathew@medportal.ca
Received: February 28, 2019 Accepted: March 08, 2019 Published: March 18, 2019
Citation: Mathew JG, Carvalho M, El-Shinnawy I, Salama S (2019) Non-Neural Granular Cell Tumor of the Eyelid: Case Report with Immunohistochemical and Ultrastructural Correlation. Int J Ophthalmic Pathol 8:1. doi: 10.4172/2324-8599.1000229
Abstract
Skin and soft tissue granular cell tumours (GCTs) are uncommon, but well-described, neoplasms that are favoured to arise from Schwann cells. Nonneural GCTs (nnGCTs) are morphologically indistinguishable from classic GCT but lack the necessary S100 positivity. nnGCTs are usually benign, although three cases with metastasis have been reported. The histogenesis of nnGCTs is uncertain. Here we report a case consistent with nnGCT arising in the skin of the eyelid with immunohistochemical and ultrasctructural correlation. This is only the second reported case of nnGCT from this site.
Keywords: Granular cell tumor; Non-neural granular cell tumor; Eyelid tumor; Dermatopathology
Introduction
Conventional granular cell tumours (GCT) of skin and soft tissue are uncommon but well-described neoplasms that characteristically exhibit features of neural differentiation, including S100 positivity by immunohistochemistry [1]. Non-neural granular cell tumors (nnGCT), referred to historically as atypical polypoid granular cell tumor and more recently as primitive non-neural granular cell tumor, are even more rare than their conventional counterpart, and while they can be morphologically indistinguishable from classic GCT, they are characteristically negative for S100 [1-3]. The histogenesis of nnGCTs remains uncertain. They are typically benign, although three cases with regional lymph node metastasis have been reported [2-5]. Non-neural granular cell tumor has been reported in patients ranging in age from 3 to 83 years with no obvious gender bias [2,6]. The most common sites have been on the back, neck, shoulders and upper extremities [2,3].
Here, we describe a case of nnGCT, arising in the skin of the eyelid. This is only the second reported case of nnGCT from this site [7].
Case Report
Clinical history
A 72 year-old male presented with a 12 × 6 mm tender nodule in the left lower eyelid below the tarsal plate. The lesion had been present for approximately five weeks and was slowly growing. There was no injection of the adjacent skin or conjunctival surface. No lymphadenopathy was apparent at initial presentation. The lesion was excised and sent for histologic examination.
Gross findings: The gross specimen consisted of a firm nodule, 1.1 cm in greatest dimension, lined by skin and conjunctival mucosa on opposite sides. On cut section the nodule consisted of homogenous pale red tissue.
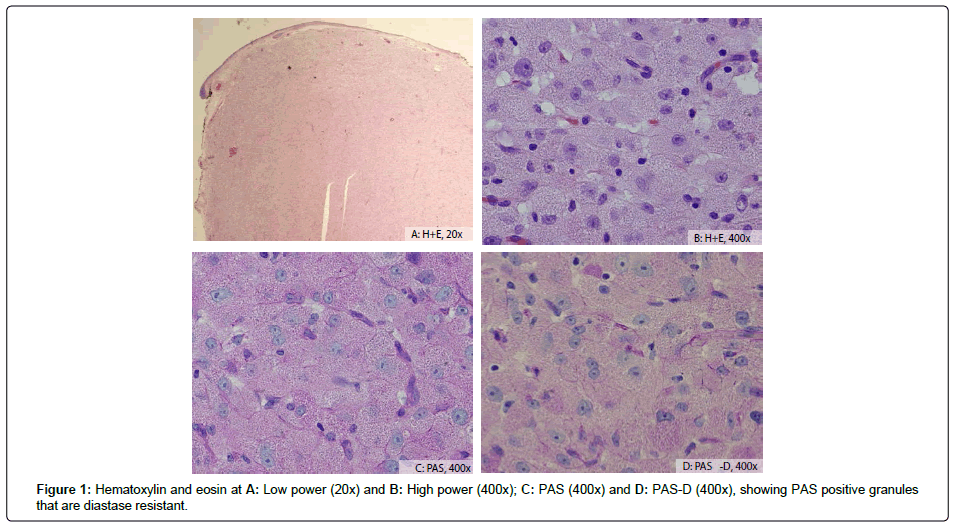
Microscopic findings: Histologic sections (Figures 1a and 1b) of the tumour showed a well circumscribed intradermal granular cell proliferation consisting of cohesive polygonal cells with abundant eosinophilic granular cytoplasm. The cells were organized into solid sheets, with a delicate vasculature in between. The nuclei were vesicular, with prominent nucleoli. There was moderate cytologic atypia and rare mitoses identified. The histology was consistent through the entire tumour. Tumor necrosis and lymphovascular invasion were absent. The tumor involved the deep resection margin.
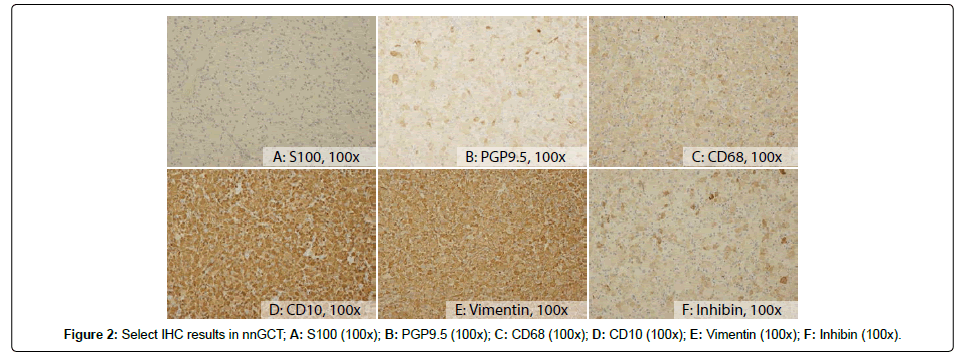
The tumour showed several features overlapping with classic GCT; intracytoplasmic granules were highlighted by PAS and PAS-D (Figures 1c and 1d). Immunohistochemistry (Figure 2) showed the tumor cells were negative for S100, cytokeratins (AE1/AE3 and Cam5.2) and epithelial membrane antigen (EMA), as well as melanoma markers (melanoma cocktail consisting of HMB-45, Melan A and tyrosinase). The tumor was also negative for neuron specific enolase (NSE) and CD34. The tumor cells were positive for CD68 and PGP9.5, as well as CD10, vimentin, and inhibin.
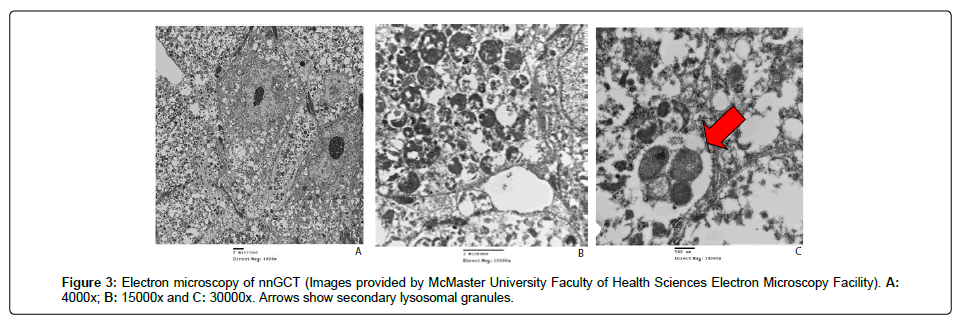
Electron microscopy: Ultrastructural examination (Figure 3) revealed primitive cells containing abundant variably-sized secondary lysosomes filling the cell cytoplasm. The cells showed no junctional desmosomal attachments, cytoplasmic filaments or membranous microvilli that would suggest epithelial differentiation. Luse bodies (long spacing collagen fibres suggestive of neural origin) were not seen.
Follow up: Despite positive margins, the patient remains disease free, without clinical recurrence or metastasis after 5 years of follow-up.
Discussion
The diagnosis of nnGCT can be challenging. The lack of S100 staining in these tumors may lead pathologists towards an alternate diagnosis, as S100 negativity would exclude a diagnosis of the conventional GCT. While nnGCT show characteristic granular cytoplasm, with intracytoplasmic granules highlighted by PAS and PAS-D, it is important to note that granular cell change can be seen in a variety of tumors. This includes granular variants of leiomyoma (typically showing fascicular architecture with positive staining for caldesmon, desmin and often smooth muscle actin), dermatofibroma (typically a poorly circumscribed lesion showing collagen entrapment by tumor cells), fibrous papule (limited to the face and typically less cellular than GCT), melanoma or nevus (typically positive for S100 and other melanoma markers including HMB45, Melan A and SOX10), atypical fibroxanthoma (typically showing marked pleomorphism and abundant mitotic activity on a background of sun damaged skin) and basal cell carcinoma, among others. Many experts consider non-neural granular cell tumor to be a diagnosis of exclusion, once these other entities have been ruled out.
Our case shows several other morphologic and immunohistochemical features that have been reported previously in nnGCT, including a well circumscribed intradermal growth pattern, vesicular nuclei and prominent nucleoli, which are less common in conventional GCT [2,3,8]. By immunohistochemistry, our case showed S100 negativity, in addition to being negative for cytokeratins, EMA, muscle markers (desmin and SMA), melanoma markers (HMB45, Melan A and tyrosinase), CD34, and NSE. This is in keeping with immunohistochemistry profiles previously reported in nnGCT [2,3]. Our case also showed positivity for PGP9.5 and CD68, highlighting nonspecific reaction to lysosomes. NKI-C3 is another lysosomal marker that has been reported as positive in these tumors [2], although this is again non-specific. This is the seventh case of nnGCT showing positive CD10 staining [4,9,10], and the first showing positive inhibin staining. Further studies are needed to determine how frequently these markers are positive in nnGCT.
Electron microscopy proved to be useful in the workup of our case. Although non-specific, the presence of secondary lysosomal granules is expected in granular cell tumors, and the absence of Luse bodies seen in tumors of neural origin supports a non-neural origin of this tumor.
Conclusion
This is the second reported case of non-neural granular cell tumor arising in the skin of the eyelid [7]. Given the diagnostic challenge that this lesion presents both clinically and histologically, it is likely that this tumor is under-recognized, and may involve the eyelid as well additional sites not previously reported more frequently than described in the literature. This diagnosis should be considered in the differential for a granular S100-negative lesion. Further studies are required to determine the histogenesis and long-term prognosis of these rare tumors.
References
- Leboit PE, Barr RJ, Burall S, Metcalf JS, Yen TS, et al. (1991) Primitive polypoid granular-cell tumor and other cutaneous granular-cell neoplasms of apparent nonneural origin. Am J Surg Pathol 15: 48-58.
- Lazar AJ, Fletcher CD (2005) Primitive nonneural granular cell tumors of skin: clinicopathologic analysis of 13 cases. Am J Surg Pathol 29: 927-934.
- Chaudhry IH, Calonje E (2005) Dermal non-neural granular cell tumour (so-called primitive polypoid granular cell tumour): a distinctive entity further delineated in a clinicopathological study of 11 cases. Histopathology 47: 179-185.
- Habeeb Al, Weinreb I, Ghazarian D (2009) Primitive non-neural granular cell tumour with lymph node metastasis. J Clin Pathol 62: 847-849.
- Newton P, Schenker M, Wadehra V, Husain A (2014) A case of metastatic non-neural granular cell tumor in a 13-year-old girl. J Cutan Pathol 41: 536-538.
- Kabir B, Ramien M, Shammary M, Nanassy J, Demellawy D (2018) Dermal non-neural granular cell tumor in a 3-year-old child. Pediatr Dermatol 35: 241-242.
- Lawson K, Mckenzie S, Gates G, Sarantopoulos GP, Smart C (2018) Cutaneous non-neural granular cell tumor presenting on the eyelid of a 3-year-old boy. American Society of Dermatopathology, Annual Meeting Poster Session 2.
- Habeeb AA, Salama S (2008) Primitive nonneural granular cell tumor (so-called atypical polypoid granular cell tumor): Report of 2 cases with immunohistochemical and ultrastructural correlation. Am J Dermatopathol 30: 156-159.
- Schoedel KE, Bastacky S, Silverman A (1998) An S100 negative granular cell tumor with malignant potential: report of a case. J Am Acad Dermatol 39: 894-898.
- Fernandez FA, Cassarino DS, Riveiro FE, Rodriguez JL, Fernandez MT, et al. (2017) Cutaneous dermal non-neural granular cell tumor is a granular cell dermal root sheath fibroma. J Cutan Pathol 44: 582-587.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi