Case Report, Int J Ophthalmic Pathol Vol: 7 Issue: 1
Orbital Solitary Fibrous Tumour: A Report of Two Cases and Review of the Literature
Albert-Fort M* and González-Candial M
Department of Ophthalmology, Doctor Josep Trueta University Hospital of Girona, Spain
*Corresponding Author : Mara Albert-Fort, MD
Doctor Josep Trueta University Hospital of Girona, Departament of Ophthalmology, Avda de Franca s/n, E-17007 Girona, Spain
Tel: + 34 972 94 02 00
Fax: + 34 972 940 296
E-mail: albert_marfon@gva.es
Received: November 14, 2017 Accepted: January 06, 2018 Published: January 13, 2018
Citation: Albert-Fort M, Gonzalez-Candial M (2018) Orbital Solitary Fibrous Tumour: A Report of Two Cases and Review of the Literature. Int J Ophthalmic Pathol 7:1. doi: 10.4172/2324-8599.1000213
Abstract
We present two clinical cases of patients aged 36 and 74 with an orbital solitary fibrous tumour (SFT). The diagnosis was confirmed by immunohistochemistry being positive for CD34, BCL-2, CD99 and STAT6. The first case was satisfactorily removed during the biopsy and in the second case partial resection was achieved. The patient was referred to neurosurgery after confirming the diagnosis and because of intracranial invasion of the tumour. Discussion Orbital SFT is a generally benign neoplasm originating from the mesenchyme, uncommon in the orbit. It is diagnosed using immunohistochemical technique and the treatment of choice is surgical resection of the tumour in order to prevent recurrences. Usually, local resection of the tumour is sufficient. However, in some situations, infiltration of the tumour requires more extensive resection of adjacent tissues. Radiation therapy does not appear to be beneficial and the efficacy of chemotherapy has not been demonstrated in this type of tumour.
Keywords: Solitary fibrous; Orbit tumor; Mesenchymal origin tumor; CD34
Introduction
Solitary fibrous tumour (SFT) is an uncommon neoplasm at the orbital level that behaves in benign way in most cases [1]. It usually presents itself as a painless ocular proptosis and has a unilateral location. Its diagnosis is histologic using immunohistochemical techniques [2]. As far as possible, treatment involves complete resection as the presence of remnants of intraorbital tumour tissue after the operation carries the risk of causing recurrence of the tumour and can even undergo transformation by becoming malignant [3]. Here we have presented two cases of orbital SFT, together with a review of the literature.
Clinical Cases
The two cases of orbital SFT were treated at the Ophthalmology Department at the Dr Josep Trueta University Hospital in Girona in 2017. In both patients an exploratory lateral orbitotomy under general anaesthetic was performed and the anatomical specimens obtained in the interventions were analysed by the Department of Pathological Anatomy at the same hospital.
Case 1
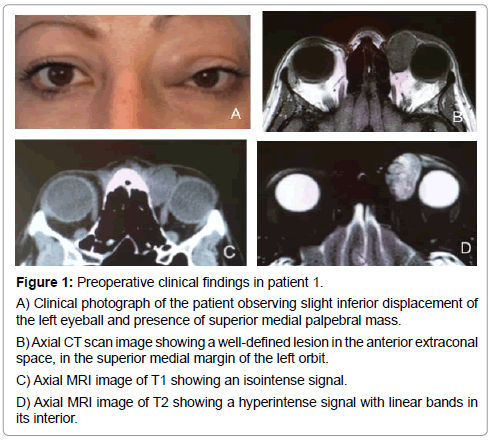
First case was a 36-year-old patient who referred to our centre for an eyelid tumour at the superior medial level of the left eye. In the exploration, visual acuity was 20/20 in both eyes; the anterior pole did not exhibit alterations, intraocular pressure (IOP) 17 mmHg in both eyes and normal eye fundus and presented with slight inferior displacement of the left eyeball. In the Computed tomography (CT), the presence of a well-defined lesion with nodular morphology, located in the anterior extraconal space in the superior medial margin of the left orbit, without visible calcifications in the inner part or signs of infiltration into the adjacent tissues was observed. The patient was able to move both the left eyeball laterally and the internal rectus muscle and presented maximum diameters of 2.5 × 1.5 × 2 cm (Figure 1). The magnetic resonance imaging (MRI) showed an isointense mass on T1 and hyperintense on T2 with some linear bands as an interior signal, compatible with intralesional vascular matrix. After administration of intravenous contrast, the mass showed an intense and homogeneous enhancement (Figure 1).
Figure 1: Preoperative clinical findings in patient 1.
A) Clinical photograph of the patient observing slight inferior displacement of the left eyeball and presence of superior medial palpebral mass.
B) Axial CT scan image showing a well-defined lesion in the anterior extraconal space, in the superior medial margin of the left orbit.
C) Axial MRI image of T1 showing an isointense signal.
D) Axial MRI image of T2 showing a hyperintense signal with linear bands in its interior.
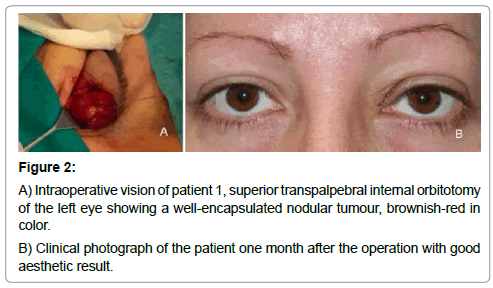
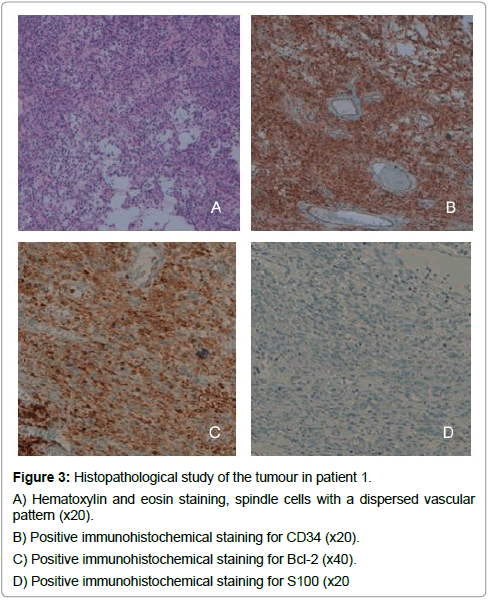
The lesion was approached through a medial incision in the upper skin fold of the left eye. The mass was located within a clear dissection plane, isolated from the surrounding extraocular muscles with no evidence of local infiltration; introduction of an overlying capsule facilitated its complete excision. Macroscopically, it was a polylobate tumour, encapsulated in a brownish colour, firmly attached to the orbital fat, with almost no visible vascular framework on the surface (Figure 2). On a histopathological level a fusocellular proliferation was observed in the presence of a vascular net-work, with some more cellular areas, and other more hyalinised areas. With regard to the mitotic activity, less than 4 mitoses per 10 high power fields were observed. The immunohistochemical stains of the tumour showed positive staining for CD34, CD99, Bcl-2, STAT6 and in contrast negative staining for SMA, S100, CD45, D240, CD31 and EMA (Figure 3).
Figure 3: Histopathological study of the tumour in patient 1.
A) Hematoxylin and eosin staining, spindle cells with a dispersed vascular pattern (x20).
B) Positive immunohistochemical staining for CD34 (x20).
C) Positive immunohistochemical staining for Bcl-2 (x40). D) Positive immunohistochemical staining for S100 (x20
There were no incidents presented in the postoperative period, with resolution of the dystopia of the eye. Three months after the operation, no recurrence has been observed. The patient continues to be monitored.
Case 2
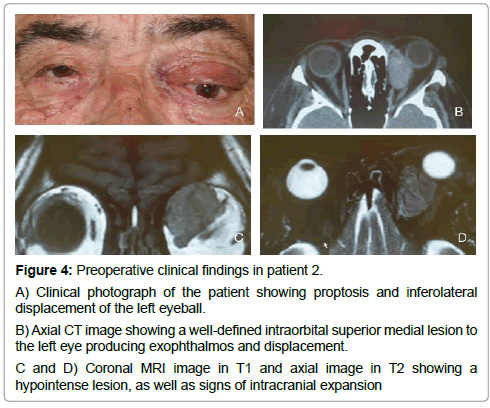
Second case was a 74-year-old patient who came in due to proptosis of the left eye and progressive vertical diplopia which had been evolving over a few months. In the visual acuity exploration the patient presented with 20/25 in both eyes, presence of conjunctival hyperaemia in the left eye, IOP 18 mmHg in both eyes and normal eye fundus. Noteworthy was the presence of dystopia of the left eyeball of 5 mm inferolateral along with exophthalmos of the same eye shown by a Hertel of 19 mm in the right eye and 25 mm in the left eye with base 100 and restriction to the movement, especially at the top. In the CT scan, an expansive well-demarcated lesion was observed in the left intraorbital superior medial with both an intra and extraconal portion measuring approximately 3 × 1.8 × 2 cm. This caused inferolateral displacement of the optic nerve, compression and displacement of the superior rectus and medial rectus muscles and inferior and external displacement of the left eyeball. It was associated with significant thinning of the bone of the left orbital roof, at the level of the inferior wall of the frontal sinus. The MRI exam showed hypointense signal on T2 (Figure 4) and after the administration of intravenous contrast, there is an intense homogeneous enhancement. An excisional biopsy was performed through a lateral superior medial orbitotomy through the skin fold in the left eye. Macroscopically, it was a tumour with vascular cords on the surface, with unclear demarcation and adjacent tissues that made the resection difficult especially towards the intraconal space; there was no presence of a capsule and the appearance was brownish with an elastic consistency in its interior. The histopathological study showed fragments with proliferation of spindle cells with hyperchromatic and elongated nuclei surrounded by collagen bands, with no signs of mitotic activity or necrosis. The immunohistochemical stains of the tumour showed positive staining for CD34, CD99, Bcl-2, STAT6 (Figure 5) and in contrast it was negative for SMA, S100, CD45, D240, CD31 and EMA. During the postoperative follow-up the tumour showed a sign of intracranial growth and thus the patient was referred to neurosurgery for its excision.
Figure 4: Preoperative clinical findings in patient 2.
A) Clinical photograph of the patient showing proptosis and inferolateral displacement of the left eyeball.
B) Axial CT image showing a well-defined intraorbital superior medial lesion to the left eye producing exophthalmos and displacement.
C and D) Coronal MRI image in T1 and axial image in T2 showing a hypointense lesion, as well as signs of intracranial expansion
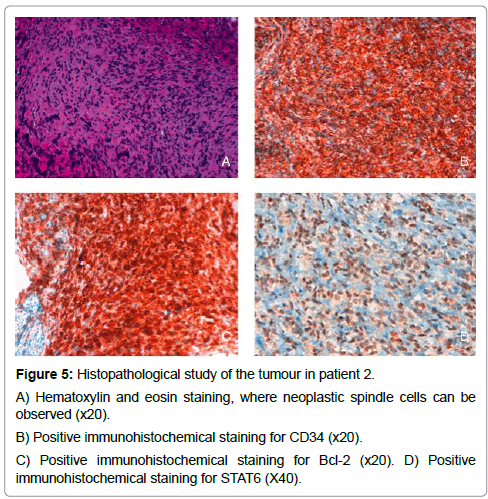
Figure 5: Histopathological study of the tumour in patient 2.
A) Hematoxylin and eosin staining, where neoplastic spindle cells can be observed (x20).
B) Positive immunohistochemical staining for CD34 (x20).
C) Positive immunohistochemical staining for Bcl-2 (x20).
D) Positive immunohistochemical staining for STAT6 (X40).
Discussion
A solitary fibrous tumour (SFT) is a rare neoplasm of spindle cells, described for the first time in 1931, by Klemperer and Rabin [4] in the pleura and considered to be from a submesothelial origin. It was not until 1942 when Stout and Murray [5] proposed a mesothelial origin according to their published studies. For many years, there has been an overlap between the tumours which are considered to be haemangiopericytoma (HPC) and SFTs as they show similar traits at a histological level, especially in the cellular forms of SFTs which are indistinguishable from the description given by Stout on HPC [6]. Currently there is no consensus in differentiating an SFT as a distinct entity from HPC. The pleura is not the only location of the tumour, it has been observed in other parts of the body such as the: pericardium,mediastinum, peritoneum, nasopharynx, sinuses, salivary gland, pelvis, adrenal gland, kidney, liver, the urogenital system, and even in the meninges and the spinal cord [7-13].
The orbit is in an extrapleural location, mostly superior medial and superior lateral (8), but we can also find it at the retrobulbar, lacrimal caruncle and fossa for lacrimal sac [14] and even in the optic nerve sheath [15]. Although its clinical presentation is very nonspecific (painless unilateral proptosis, ordinary palpable mass, effect on eye movement, hyper-globus or blepharoptosis secondary to mass effect), since the first case published by Westra et al. in 1994, more than 50 cases have been described in this location, with increasing diagnosis thanks to immunohistochemical techniques, in particular using the CD34 antigen [2].
The vast majority of orbital SFTs have a benign behaviour, therefore in 2002, the World Health Organisation classified it as an “intermediate type, rarely metastasising” [16], although it has to be acknowledged that 5-10% of cases may manifest themselves in a more aggressive clinical form, characterised by local invasion, tumour recurrence and even some isolated cases of extraorbital tumour invasion [1,3,17-20] have also been published. The mechanism causing malignant tumour transformation is still unknown. Cases in which the tumour is larger than 5 cm and has a histological level presenting hypercellularity, a mitotic rate of more than 4 mitoses per 10 high power fields and the presence of necrosis [21,22] are considered potentially malignant. Mosquera et al. speak of a possible phenomenon of “dedifferentiation” in some cases of orbital SFT, a behaviour that has been described in other well-differentiated tumours, such as liposarcoma, chordoma, chondrosarcoma and osteosarcoma, defined by the presence of an abrupt transition between the well-differentiated tumour component and the highgrade, poorly differentiated areas accompanied by loss of positivity for CD34 and overexpression of p16 and p53 that make it a more aggressive biological variety. These areas described are different from those that manifest in a normal malignant SFT in which these two morphologically distinct components do not exist in the same tumour [20,23]. The role that radiation therapy can play in cases of malignant transformation is not known either; Blandamura et al. [21], published a case of orbital SFT that was treated with radiation therapy for an early recurrence a year after the surgical removal, which recurs with a generally more aggressive behaviour.
The radiological studies of the SFT located in the head and neck are quite unspecific [24,25]. Orbital SFTs are visible in CT scan as well-defined lesions with heterogeneous density, which can sometimes present calcifications in their interior and rarely manifest effects on the bone, which should then suspected as showing behaviour concurrent with a malignant tumour [24-26]. In a MRI study the isointensity is shown with regard to the muscle on T1 and hypointense on T2. The tumour stands out when using a contrast medium as it is richly vascularised [25,27,28]. In addition, as published by Kim et al. [25], tubular structures in the interior of the lesion can be observed showing the intensity of a null signal that may be compatible with blood flow within the tumour, as you can see in our case 2 (Figure 3). An angiography is a complementary technique that is used for this type of tumour with vascular characteristics [29-31], it should be taken into account that the differential diagnosis provided by the radiological findings describing SFT lesions are for highly vascular orbital lesions such as capillary haemangioma, cavernous haemangioma, haemangiopericytoma and giant cell angiofibroma [25], and on occasion the CT and MRI scans do not reveal sufficient diagnostic information. Hasegawa M et al. also state that the preoperative diagnosis is essential for the therapeutic management which should take place for orbital tumours and that the angiography provides us with a more accurate preoperative anatomical and pathological picture for almost all types of orbital lesions, especially with regard to the characterisation of normal vascular anatomy and pathology as demonstrated in his study. In addition he claimed that the combination of the arteriography and CT scan techniques are able to not only reveal the presence of nutrient vessels that are not visible on the digital subtraction angiography or the traditional MRI, but also they can also show the component of the tumour fed by the internal carotid artery or the external carotid artery, the latter being useful to estimate the effectiveness of the preoperative embolization [31].
Diagnosis is established through a histological study together with immunohistochemical confirmation. In general, the natural history of fibroblast tumours is more difficult to establish by cytological criteria than superficial epithelial tumours. Therefore, given the variable histological appearance of the tumour, orbital SFTs are often confused with other orbital spindle cell tumours such as hemangiopericytoma, fibrous histiocytoma (HF), meningioma and schwannoma [8,32]. Among the most classic histological characteristics are the thick bands of collagen alternating with areas of hypocellularity and hypercellularity and a vascular pattern similar to hemangiopericytoma [33,34]. However, it has been acknowledged that there is a wide spectrum of histological forms of SFT, and thus SFT variants have been suggested according to the morphological characteristics found: cell variant of SFT (with numerous thin-walled vessels with a less fibrous component), a fibrous variant of SFT (with a highly fibrous component) and other variants such as the fat-forming SFT (formerly known as HPC lipomatous, with a branching vascular pattern with the presence of a variable number of mature, atypical adipocytes) and the variant of SFT rich in giant cells (formerly known as giant cell.
Angiofibroma is characterised by the presence of numerous giant stromal cells, distributed throughout the lesion or pseudovascular walls) [35,36]. It must also be stressed that there is an overlap between the SFT and the variant of malignant fibrous histiocytoma, which a large proportion is expressed in CD34 and can therefore represent another variant of SFT [36-38]. These histologic patterns can guide us to the diagnosis of the tumour, but it must be taken into account that it may be complicated when there is little biological material (for example in a biopsy) or if there are malignant characteristics present. SFTs are characterised using immunohistochemical techniques, showing as positive in CD34. The antigen CD34 is selectively expressed in hematopoietic stem cells in the vascular endothelium [2,39,40] being a diagnostic tool for different types of leukaemia and vascular neoplasms. Based on the presence of studies which showed that certain populations of mesenchymal stromal cells in the dermis and other locations showing CD34 immunoreactivity [41,42], as a result of his study, Westra W.H. et al. proposed that this marker was a potential tool for the diagnosis of this type of tumour [2]. In addition, SFT is immunoreactive to CD99 [43], STAT6 [44] and Bcl-2 [45]. On the other hand, it is positive to mesenchymal markers such as vimentin and negative for epithelial markers (cytokeratin), vascular (factor VIII-related antigen), neural (S-100 protein) and smooth muscle-specific actin [46].
For a lesion with benign behaviour, the treatment of choice is complete surgical resection of the tumour, whenever possible, without leaving any remains of the tumour to prevent recurrence and malignant transformation [4,13,19]. Previous use of embolizing agents such as onyx, in orbital SFTs in the case of vascular lesions and facilitating their subsequent resection [29] has been recently published. Furthermore, radiation therapy has been used in the isolated treatment of some SFT cases, however this is controversial both for its use and because of potential damage to vital orbital structures such as the optic nerve, as well as possible recurrence of the tumour that has been described after the intervention as published in a case by Blandamura et al. [21].
Conclusion
Orbital SFT is a generally benign neoplasm originating from the mesenchyme, uncommon in the orbit. It is diagnosed using immunohistochemical technique and the treatment of choice is surgical resection of the tumour in order to prevent recurrences. Usually, local resection of the tumour is sufficient. However, in some situations, infiltration of the tumour requires more extensive resection of adjacent tissues. Radiation therapy does not appear to be beneficial and the efficacy of chemotherapy has not been demonstrated in this type of tumour.
References
- Le CP, Jones S, Valenzuela AA (2014) Orbital solitary fibrous tumor: a case series with review of the literature Orbit 33: 145-151.
- Westra WH, Gerald WL, Rosai J (1994) Solitary fibrous tumor. Consistent CD34 immunoreactivity and occurrence in the orbit. Am J Surg Pathol 18: 992-998.
- Glazer-Hockstein C, Syed NA, Warhol M, Gausas RE (2004) Malignant solitary fibrous tumor metastatic to the orbit. Ophthal Plast Reconstr Surg 20: 471-473.
- Klemperer P, Rabin C (1931) Primary neoplasm of the pleura: A report of five cases. Arch Pathol 11: 385-412.
- Stout AP, Murray MR (1942) Localized pleural mesothelioma: investigation of its characteristics and histogenesis by the method of tissue culture. Arch Pathol 34: 951-964.
- Stout AP, Murray MR (1942) Hemangiopericytoma: a vascular tumour featuring Zimmermann’s pericytes. Ann Surg 116: 26-33.
- Gengler C, Guillou L (2006) Solitary fibrous tumour and haemangiopericytoma: evolution of a concept. Histopathology. 48: 63-74.
- Furusato E, Valenzuela IA, Fanburg-Smith JC, Auerbach A, Furusato B, et al. (2011) Orbital solitary fibrous tumor: encompassing terminology for hemangiopericytoma, giant cell angiofibroma, and fibrous histiocytoma of the orbit: reappraisal of 41 cases. Hum Pathol 42: 120-128.
- Brunnemann RB, Ro JY, Ordonez NG, Mooney J, El-Naggar AK, et al. (1999) Extrapleural solitary fibrous tumor: a clinicopathologic study of 24 cases. Mod Pathol 12: 1034-1042.
- Fukunaga M, Ushigome S, Nomura K, Ishikawa E (1995) Solitary fibrous tumor of the nasal cavity and orbit. Pathol Int 45: 952-957.
- Fukunaga M, Naganuma H, Nikaido T, Harada T, Ushigome S (1997) Extrapleural solitary fibrous tumor: a report of seven cases. Mod Pathol 10: 443-450.
- Nielsen GP, O'Connell JX, Dickersin GR, Rosenberg AE (1997) Solitary fibrous tumor of soft tissue: a report of 15 cases, including 5 malignant examples with light microscopic, immunohistochemical, and ultrastructural data. Mod Pathol 10: 1028-1037.
- Hasegawa T, Matsuno Y, Shimoda T, Hasegawa F, Sano T, et al. (1999) Extrathoracic solitary fibrous tumors: their histological variability and potentially aggressive behavior. Hum Pathol 30: 1464-1473.
- Scott IU, Tanenbaum M, Rubin D, Lores E (1996) Solitary fibrous tumor of the lacrimal gland fossa. Ophthalmology 103: 1613-1618.
- Kitamura Y, Akiyama T, Hirose S, Yoshida K (2012) Optic nerve sheath solitary fibrous tumor. Acta Neurochir 154: 633-635.
- Fletcher CDM, Unni KK, Mertens F (2002) World Health Organization Classification of Tumours. Pathology and Genetics of the Tumours of the Soft Tissue and Bone. Lyon: IARC Press, France.
- Hasegawa T, Matsuno Y, Shimoda T, Hasegawa F, Sano T, et al. (1999) Extrathoracic solitary fibrous tumors: their histological variability and potentially aggressive behavior. Hum Pathol 30: 1464-1473.
- Girnita L, Sahlin S, Orrego A, Seregard S (2009) Malignant solitary fibrous tumour of the orbit. Acta Ophthalmol 87: 464-467.
- Parrozzani R, Fusetti S, Montesco C, Favero V, Midena E (2013) Biphasic solitary fibrous tumor of the orbit with distant metastases. Int Ophthalmol 33: 701-705.
- Mosquera JM, Fletcher CD (2009) Expanding the spectrum of malignant progression in solitary fibrous tumors: a study of 8 cases with a discrete anaplastic component--is this dedifferentiated SFT? Am J Surg Pathol 33: 1314-1321.
- Blandamura S, Alaggio R, Bettini G, Guzzardo V, Valentini E, et al. (2014) Four cases of solitary fibrous tumour of the eye and orbit: one with sarcomatous transformation after radiotherapy and one in a 5-year-old child's eyelid. J Clin Pathol 67: 263-267.
- England DM, Hochholzer L, McCarthy MJ (1989) Localized benign and malignant fibrous tumors of the pleura. A clinicopathologic review of 223 cases. Am J Surg Pathol 13: 640-658.
- Yokoi T, Tsuzuki T, Yatabe Y, Suzuki M, Kurumaya H, et al. (1998) Solitary fibrous tumour: significance of p53 and CD34 immunoreactivity in its malignant transformation. Histopathology 32: 423-432.
- Ganly I, Patel SG, Stambuk HE, et al. (2006) Solitary fibrous tumors of the head and neck: a clinicopathologic and radiologic review. Arch Otolaryngol Head Neck Surg 132: 517-525.
- Kim HJ, Kim YD, Yim YJ, Kim ST, Jeon P, et al. (2008) Solitary fibrous tumor of the orbit: CT and MR imaging findings. AJNR Am J Neuroradiol 29: 857-862.
- Festa S, Lee HJ, Langer P, Klein KM (1999) Solitary fibrous tumor of the orbit: CT and pathologic correlation. Neuroradiology 41: 52-54.
- Krishnakumar S, Subramanian N, Mohan ER, Mahesh L, Biswas J, et al. (2003) Solitary fibrous tumor of the orbit: a clinicopathologic study of six cases with review of the literature. Surv Ophthalmol 48: 544-554.
- Perez Moreiras JV, Prada Sanchez MC (2002) Patología orbitaria Tomo 2. Barcelona, Edika Med.
- Hashemi N, Ling JD, Soparkar C, Sami M, Ellezam B, et al. (2015) Transarterial Onyx Embolization of an Orbital Solitary Fibrous Tumor. Ocul Oncol Pathol 1: 98-102.
- Warner EJ, Burkat CN, Gentry LR (2013) Orbital Fibrous Histiocytoma Mimicking Cavernous Hemangioma on Dynamic Contrast-enhanced MRA Imaging. Ophthal Plast Reconstr Surg 29: e3-5.
- Hasegawa M, Fujisawa H, Hayashi Y, Yamashita J, Suzuki M, et al. (2005) CT arteriography for orbital tumors: diagnostic and surgical value. J Clin Neurosci 12: 548-552.
- Kashyap S, Pushker N, Meel R (2009) Orbital schwannoma with cystic degeneration. Clin Experiment Ophthalmol 37: 293-298.
- Dalton WT, Zolliker AS, McCaughey WTE, Jacques J, Kannerstein M (1979) Localized primary tumors of the pleura: an analysis of 40 cases. Cancer 44: 1465-1475.
- Scharifker D, Kaneko M (1979) Localized fibrous “mesothelioma” of pleura (submesothelial fibroma): a clinicopathologic study of 18 cases. Cancer 43: 627-635.
- Pitchamuthu H, Gonzalez P, Kyle P, Roberts F (2009) Fat-forming variant of solitary fibrous tumour of the orbit: the entity previously known as lipomatous haemangiopericytoma. Eye 23: 1479-1481.
- Gengler C, Guillou L (2006) Solitary fibrous tumour and haemangiopericytoma: evolution of a concept. Histopathology 48: 63-74.
- Coindre JM (2002) Deep benign fibrous histiocytoma. In World Health Organization classification of tumours. Pathology and genetics of tumours of soft tissue and bone. Lyon: IARC Press 114-115.
- Croxatto JO, Font RL (1982) Hemangiopericytoma of the orbit: a clinicopathologic study of 30 cases. Hum Pathol 13: 210-218.
- Fina L, Molgaard HV, Robertson D, Bradley NJ, Monaghan P, et al. (1990) Expression of the CD34 gene in vascular endothelial cells. Blood 75: 2417-2426.
- Molgard HV, Spurr NK, Greaves MR (1989) The hemapoeitic stem cell antigen, CD34, is encoded by a gene located on chromosome1. Leukemia 3: 169-180.
- Arber DA, Kandalaft PL, Mehta P, Battifora H (1993) Vimentin-negative epithelioid sarcoma. The value of an immunohistochemical panel that includes CD34. Am J Surg Pathol 17: 302-307.
- Nickoloff BJ (1991) The human progenitor cell antigen (CD34) is localized on endothelial cells, dermal dendritic cells, and perifollicular cells in formalin-fixed normal skin, and on proliferating endothelial cells and stromal spindle-shaped cells in Kaposi's sarcoma. Arch Dermatol 127: 523-529.
- Renshaw AA (1995) O13 (CD99) in spindle cell tumors. Reactivity with hemangiopericytoma, solitary fibrous tumor, synovial sarcoma, and meningioma but rarely with sarcomatoid mesothelioma. Appl Immunohistochem 3: 250-256.
- Yoshida A, Tsuta K, Ohno M, Yoshida M, Narita Y, et al. (2014) STAT6 immunohistochemistry is helpful in the diagnosis of solitary fibrous tumors. Am J Surg Pathol 38: 552-559.
- Chilosi MFF, Dei Tos AP, Lestani M, Morassi ML, Martignoni G, et al. (1997) Bcl-2 expression in pleural and extrapleural solitary fibrous tumours. J Pathol 181: 362-367.
- Hashemi N, Ling JD, Soparkar C, Sami M, Ellezam B, et al. (2015) Transarterial Onyx Embolization of an Orbital Solitary Fibrous Tumor. Ocul Oncol Pathol 1: 98-102.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi