Research Article, J Spine Neurosurg Vol: 6 Issue: 5
Ossification Of The Ligamentum Flavum Of The Lumbar Spine In Caucasians: Case Series
Abolfazl Rahimizadeh1*, Housain Soufiani1, Mahan Amirzadeh1 and Shaghayegh Rahimizadeh2
1Pars Advanced and minimally invasive Manners medical research Center, Pars Hospital, Tehran, Iran
2Medical Doctor, Atlantic University, School of Medicine, P.O. Box 456 Island Park, NY, 11558, USA
*Corresponding Author : Dr. Abolfazl Rahimizadeh, MD
Pars Advanced and Minimally Invasive Manners Medical Research Center, Pars Hospital, Affiliated to Iran University of Medical Sciences, Keshawarz Blvd, Tehran, Iran
Tel: +098 21 88661244
E-mail: a_rahimizadeh@hotmail.com
Received: October 26, 2017 Accepted: November 08, 2017 Published: November 13, 2017
Citation: Rahimizadeh A, Soufiani H, Amirzadeh M, Rahimizadeh S (2017) Ossification of the Ligamentum Flavum of the Lumbar Spine in Caucasians: Case Series. J Spine Neurosurg 6:5. doi: 10.4172/2325-9701.1000283
Abstract
Ossification of the ligamentum flavum or OLF is a disease with heterotopic ossification in this spinal ligament. The key of OLF pathogenesis is the differentiation of fibroblasts into osteoblasts. The majority of cases of ossification of the yellow ligament occur at the lower third of the thoracic or the thoracolumbar spine. However, the literature contains only few reports of patients with OLF of the lumbar spine. The clinical presentation of lumbar OLF is radiculopathy or intermittent neurogenic claudication, although some might remain asymptomatic. Herein, we present 8 Caucasians with symptomatic lumbar OLf. The age and gender as well as the clinical picture, characteristic radiological features, the number of the affected levels will be described. The tips and tricks for achievement of a successful decompressive laminectomy, as the treatment of choice, done at one level in three and at two levels in five cases will be described. Furthermore, the degree of adherence of the lesions to dura and ultimate outcome will be discussed.
Keywords: Canal stenosis; Lumbar spine; Ossification of ligamentum flavum; Ossification of yellow ligament
Introduction
Ossification of the ligamentum flavum (OLF) was first reported in the 1920s by Polgar in lateral radiographs. This was further described by Yamaguchi and Isuruni as thickened or ossified ligamentum flavum this pathology is now appreciated as an important cause of thoracic myeloradiculopathy in Japanese population [1-4]. With regard to prevalence, this ligamentous disease is reported to occur in up 20% of the people older than 65 years among Japanese and many reports viewed it as a normal feature of aging in this ethnic group [2-4]. For more than 3 to 4 decades, it was believed that ossification of the ligamentum flavum occurs exclusively in Japanese people. However, this belief was ruled out, once the disease was found increasingly in other ethnic groups, in particular in Chinese and Koreans in the past few years [5-8].
In a prospective study done by Guo et al. in 2009, of total of 1736 Chinese volunteers for whom whole spine MRI had been done, the prevalence of OLF was 3.8% [5]. Surprisingly, in another study done by Lang et al the prevalence rate of thoracic OLF in 993 Chinese who had done chest spiral C.T scan reached to 63.9%.
Other than the East Asian people, there have been some scattered case reports among whites, Indians, Africans, Arabs and Caucasians [9-17]. However, there have been no case series reports among Iranian population.
Most of the OLFs occurs at the thoracic spine mainly at lower thoracic levels, but lumbar affection is regarded a rare entity [2-8]. In the survey of Guo et el. evaluating whole spine MRI of 1736 outpatients cases, only one subject with lumbar OLF with prevalence of 0/1%could be found [5]. In 1988, Kurihara et al. analyzed 2403 plain lumbar roentgenograms and found a prevalence rate of 8.4% for lumbar spine OLF, with frequent involvement of the upper and middle lumbar spine [18]. However, it should be noted that most of the patients harboring ossification of yellow ligaments were asymptomatic.
However, lumbar OLF as a distinct paper was first reported by Weiss and Spencer in 1970. Since then only a few papers with detailed information have been published so far. Surprisingly, majority of the cases with lumbar OLF were among east asian population. Furthermore, although with increased use of new imaging modalities, it was expected that more reports among Non-East Asian people emerge, but the number of the cases with the symptomatic lumbar OLF did not increase in the literature. Therefore, published papers about lumbar OLF remained scarce and confined to a few case reports.
Herein, a retrospective survey of 8 Iranian patients with lumbar OLF will be reported. Age, sex, medical history, clinical picture, interesting imaging features and family history of ossified spinal lesions are noted. Surgical treatment of choice and ultimate outcome after surgery will be described.
Material and Methods
We retrospectively reviewed the charts, imaging studies, and pathological reports obtained in 8 Iranian patients with symptomatic lumbar canal stenosis secondary to OLF treated at our hospital. There were four males and four female patients. The mean age at presentation was 61.75 years (range 37 to79 years). The clinical picture in three cases was lower limb radiculopathy and in the remaining five was neurogenic claudication. Duration of the symptoms from the onset before initial consultation to surgery ranged from 4 to 32 months with an average of 10.8 months. Sphincter dysfunction was not seen in any of these patients. Obesity was observed only in one patient and diabetes mellitus was not found in any. But, no other concomitant systemic diseases such as, flurosis, hemochromatosis and calcium metabolism disorders were found in the patients of this series. No family history of lumbar canal stenosis or lumbar laminectomy could be found in close relatives of the patients.
Radiological assessment included plain radiographs, standing dynamic lateral radiographs, magnetic resonance imaging (MRI) and axial and reconstructed computed tomography (CT) scan which were done in all cases.
Whole-spine MRI was also performed in all cases for exclusion of tandem involvement.
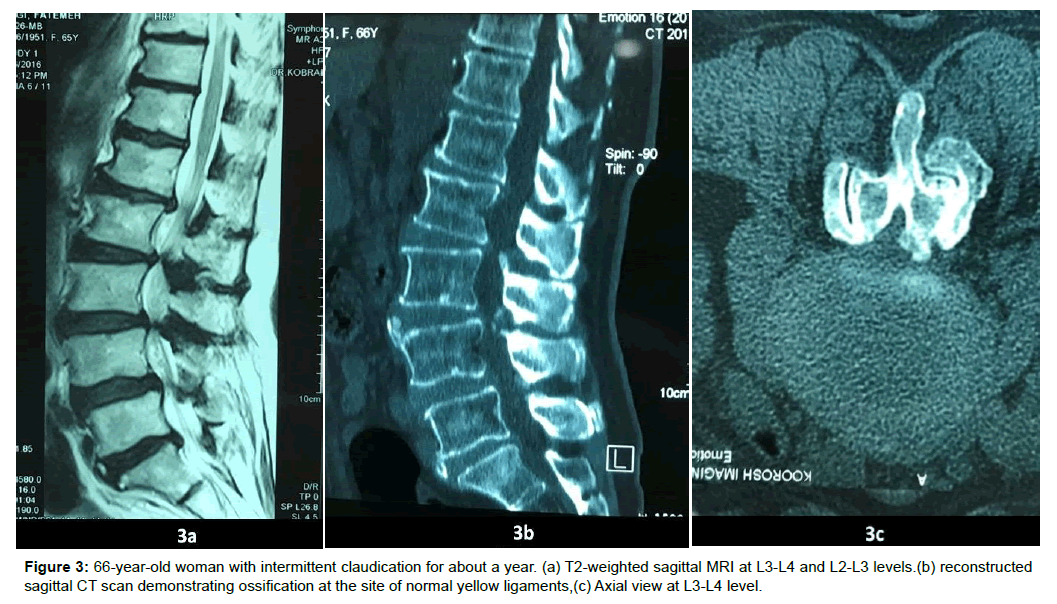
The upper lumbar region was the common site of involvement by the disease. The pathology was isolated in four and multiple in four all continuous. In all cases, the lesions were bilateral, affecting one level in three, double-level in five (Figures 1-5).
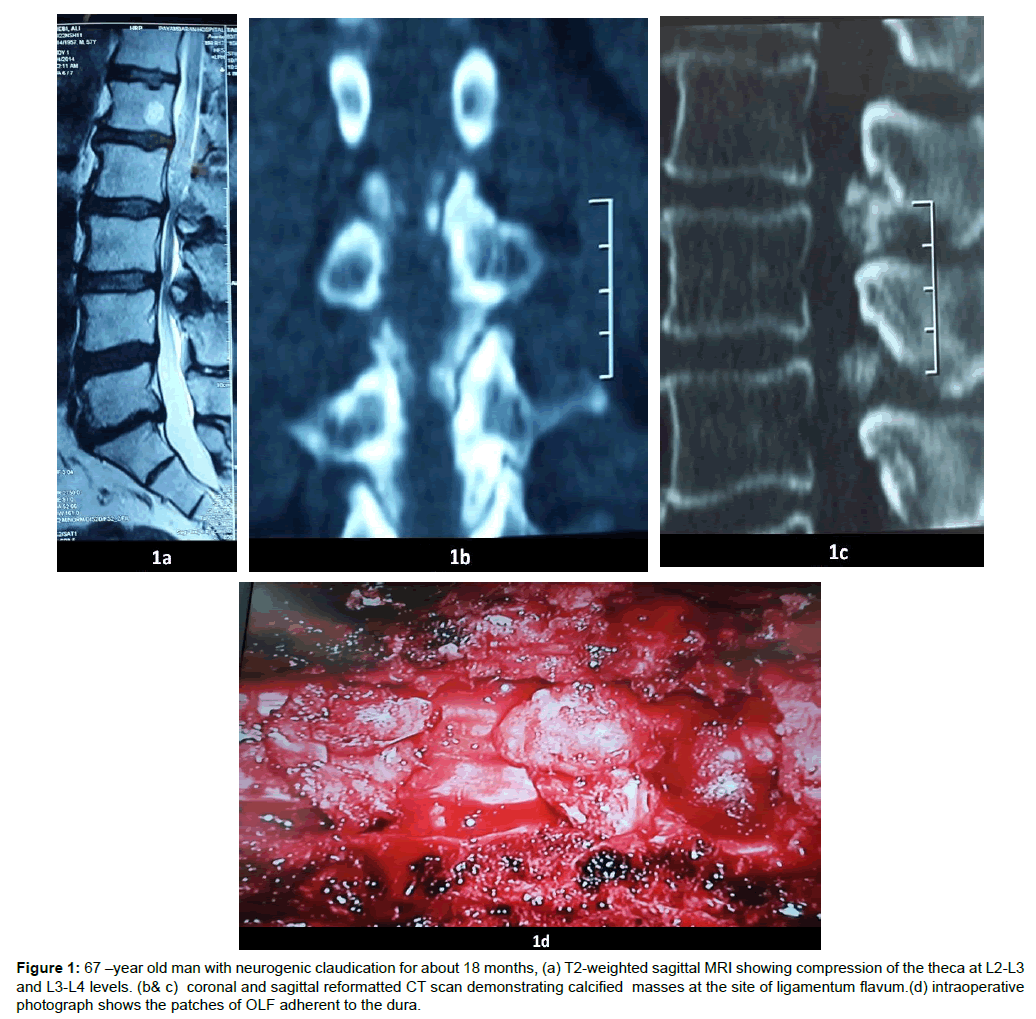
Figure 1: 67 –year old man with neurogenic claudication for about 18 months, (a) T2-weighted sagittal MRI showing compression of the theca at L2-L3 and L3-L4 levels. (b& c) coronal and sagittal reformatted CT scan demonstrating calcified masses at the site of ligamentum flavum.(d) intraoperative photograph shows the patches of OLF adherent to the dura.
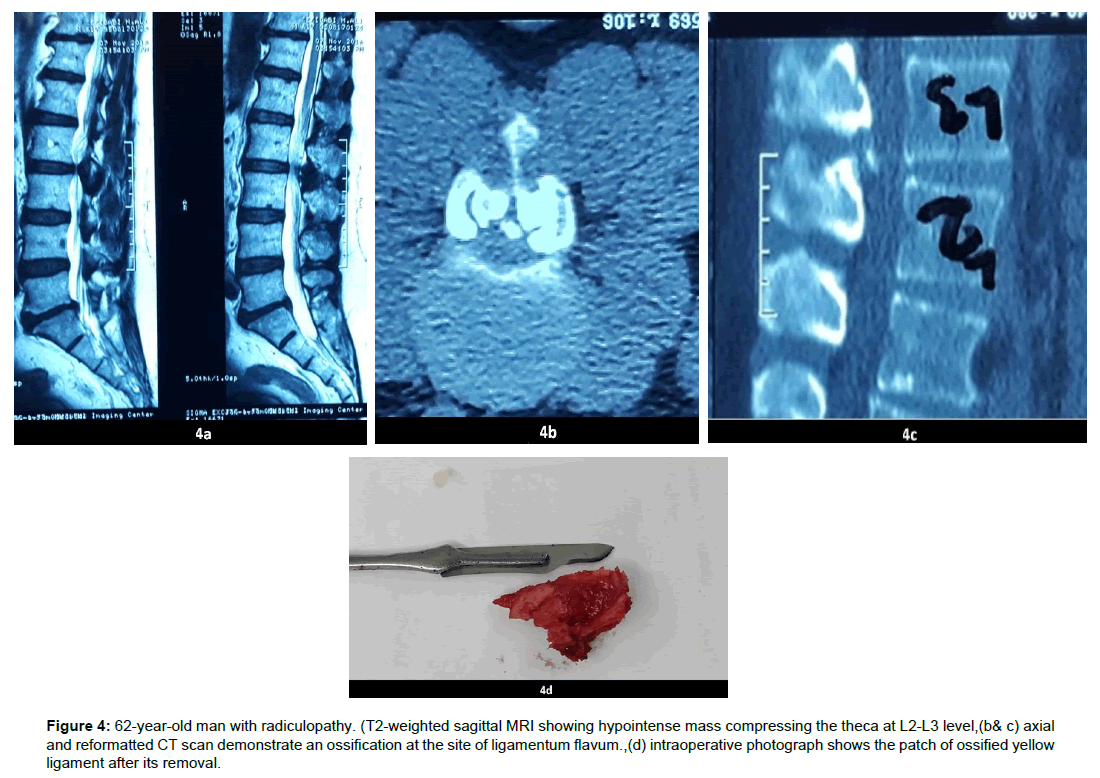
Figure 4: 62-year-old man with radiculopathy. (T2-weighted sagittal MRI showing hypointense mass compressing the theca at L2-L3 level,(b& c) axial and reformatted CT scan demonstrate an ossification at the site of ligamentum flavum.,(d) intraoperative photograph shows the patch of ossified yellow ligament after its removal.
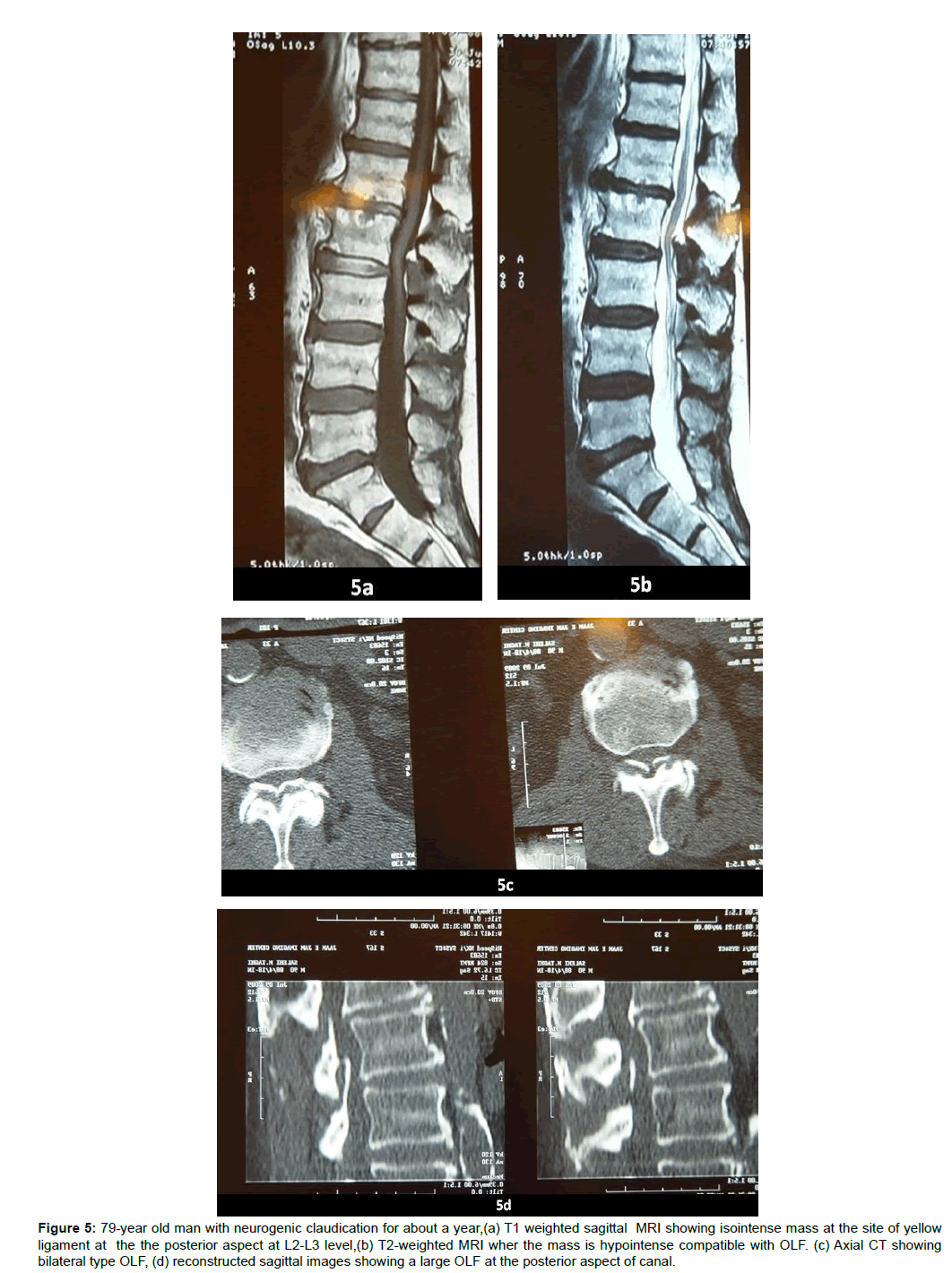
Figure 5: 79-year old man with neurogenic claudication for about a year,(a) T1 weighted sagittal MRI showing isointense mass at the site of yellow ligament at the the posterior aspect at L2-L3 level,(b) T2-weighted MRI wher the mass is hypointense compatible with OLF. (c) Axial CT showing bilateral type OLF, (d) reconstructed sagittal images showing a large OLF at the posterior aspect of canal.
However, radiographic features of ankylosing spondylitis and diffuse idiopathic skeletal hyperostosis (DISH) were not detected in the present study.
Surgical intervention
All patients underwent decompressive laminectomy. In total, 13 segments were decompressed. Surgery was started with a midline incision over the involved levels, with subsequent resection of the spinous processes followed by laminectomy. Laminectomy was done with the aid of high speed burr being started laterally near the medial facet joints with making a groove till dura could be exposed bilaterally. Drilling with burr was continued till the remaining lamina became paper thin. Thereafter, OLF dissection from the dura was done microscopically in seven and macroscopically in one. Adherence of OLFs to the dura was mild or moderate in 7, where in one was tight and severe.
Result
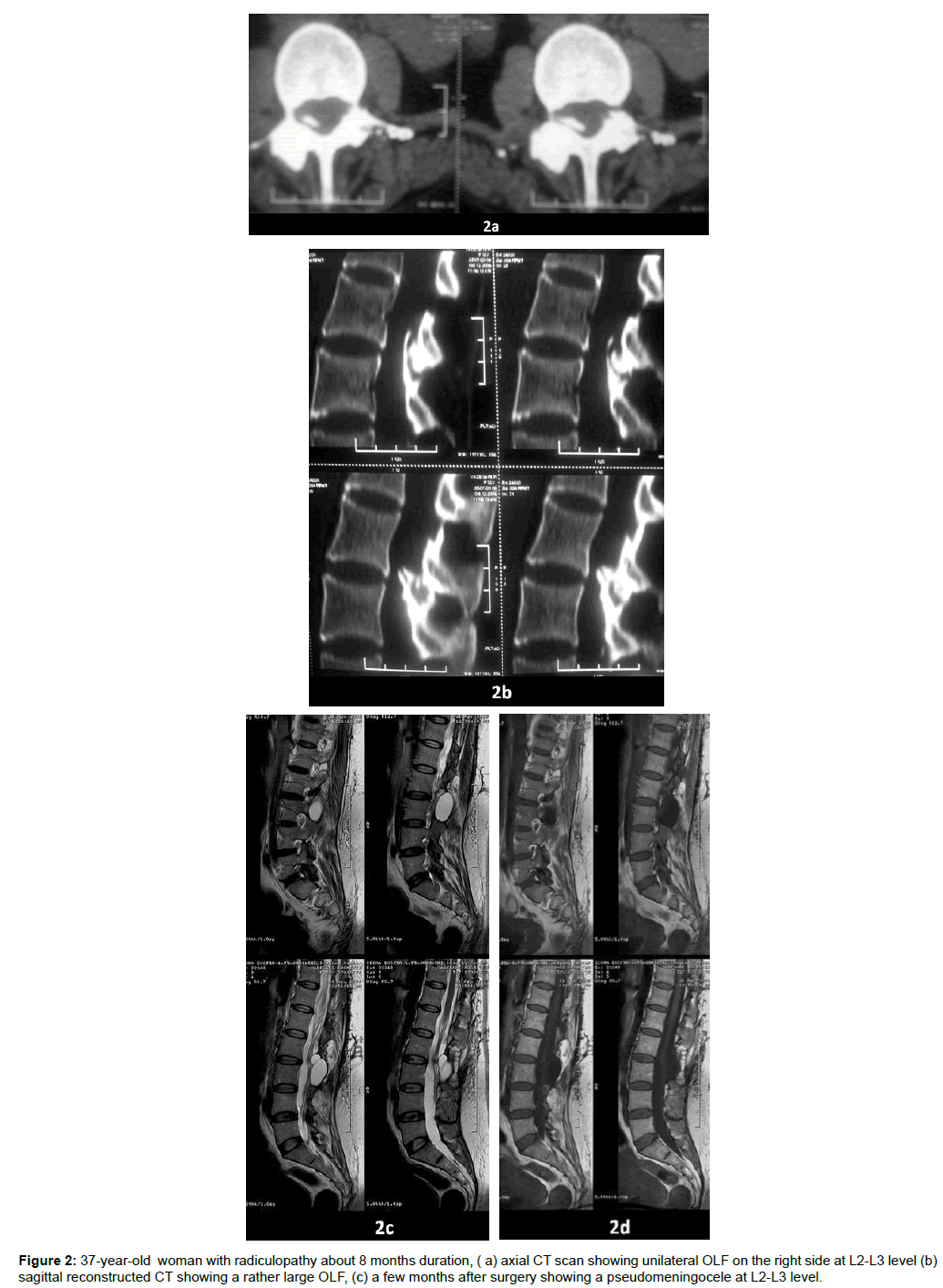
All patients showed good recovery except one who was readmitted because of low back pain in straining and coughing. In this case, further evaluation showed pseudomeningocele formation which was cured after a redo surgery.
The patients were followed from two to 82 months and no case with signs of recurrence of OLF could be detected. With classification of outcome to excellent, good, fair and poor, 6 patients were excellent and 2 were good. The distribution of lumbar OLF by age and gender and the level and the number of the affected levels are shown in Table 1.
| No | Sex | Age | Clinical Picture | Affected Levels | Treatment | Outcome |
|---|---|---|---|---|---|---|
| 1 | M | 67 | Intermittent claudication | L2-L3+L3-L4 | Laminectomy | excellent |
| 2 | F | 37 | Radiculopathy | L2-L3 | Laminectomy | Good |
| 3 | F | 66 | Intermittent claudication | L2-L3-L3-L4 | Laminectomy + Screw rod fixation | Good |
| 4 | M | 62 | Radiculopathy | L2-L3 | Laminectomy | excellent |
| 5 | M | 79 | Intermittent claudication | L2-L3 | Laminectomy | excellent |
| 6 | F | 64 | Intermittent claudication | L1-L2+L2-L3 | Laminectomy | excellent |
| 7 | F | 58 | Radiculopathy | L2-L3 | Laminectomy | Excellent |
| 8 | M | 61 | Intermittent claudication | L2-L3+ L3-L4 | Laminectomy | Excellent |
Table 1: showing the age, sex, clinical picture, the number of the affected levels, treatment and ultimate outcome of 8 patients.
Discussion
Ligamentum flavum is a well-defined elastic structure. About 80% of this ligament is composed of elastic fibers and 20% of collagen fibers. The function of this ligament is preserving intrinsic stability of spine.
Pathology
Ossified ligamentum flavum (OLF) is characterized by ectopic bone formation in the ligamentum flavum which is normally composed of fibrous tissue. Development of OLF begins with hypertrophy of this ligament (LF) gradual loss of elastic fibers, differentiation of the fibroblast into chondrocytes followed by transformation of the chondrocytes into osteoblasts.
Ligamentum flavum ossification, calcification and calcium pyrophosphate dehydrate crystal deposition disease (CPPDcdd) which are quite different entities, sometimes are confused due to lack of inadequate histological examination. However, it is now proved that calcification of the ligamentum flavum and CPPDcdd belong to a single category. Initially, basic changes in these two entities are similar and begin with retrograde degeneration. But, later their difference will become apparent with respect to the corresponding histologic findings.
Ossification initially develops in the cephalic and the caudal attachments of the ligamentum flavum to lamina, at the junction of the bone and ligament (enthesis) and is actually described as endochondral ossification or enthesopathy. Characteristic features of endochondral ossification are demonstration of the foci of wellformed woven bone, lamellar bone structure and bone marrow formation being surrounded by chondroid cells.. These findings indicate that factors other than aging are considered to be involved in formation, development and progress of the ossification. In calcification, CPPD crystals are deposited within degenerated ligamentous fibers calcified granules.
Eventually, mature bone is not demonstrated inside the degenerated ligament.
However, calcification is associated with increased CPPD crystal deposition being demonstrated as calcified granules inside the degenerated ligament.
Ossification of the yellow ligament mostly occurs at the lower third of the thoracic or the thoracolumbar spine, from T9 to T12 [2-8]. However, only a few authors have published surgically treated OLF of the lumbar spine with detailed clinical and radiological features [18-25]. Most of the cases with lumbar OLF have been observed in east Asian people, with only a few case reports from non-East Asian areas, from North America, Greece and Turkey have been published to date [19,21,23,24]. Therefore, this is the first lumbar OLF case series from non-east Asian countries and the first case series in Caucasian if we accept that Iranians are dissident of pure Aryans.
Pathogenesis
Despite numerous basic science studies, the pathogenesis of OLF has not been conclusively established. However, several investigators have described the possible contribution of repeated mechanical stress, metabolic diseases such as diabetes mellitus, hyperinsulism, hemochromatosis, calcium metabolism abnormalities, genetic and cell biological factors it has also been reported that patients with OLF have a higher frequency in the patients with obesity and in the cases with higher bone mineral density [26-35]. Besides these factors, dietary habits may constitute an independent risk factor for OLF formation. Moreover, it is known that the incidence of OLF is higher in patients with diffuse idiopathic skeletal hyperostosis, fluorosis, and ankylosing spondylitis [36].
In contrast to thoracic OLF which is reported to involve patients predominantly in their 60s and 70s, the reported lumbar OLF has been found to occur in younger people with mean of 53, 25 unpublished case reports. The mean age of the reported cases is less than our series with 61,75. However, review of the published papers about LOLF shows almost equally affection in males and females correlating with our case series [18-24].
Clinical feature
The slowly progressive course of lumbar OLF makes its early diagnosis difficult. Nonetheless, the symptoms in patients with OLF in the lumbar spine are similar to the cases with lateral recess syndrome or degenerative lumbar canal stenosis where it can be presented with radiculopathy or intermittent claudication respectively. Because of the insidious behavior of lumbar OLF, it is not unusual to depict the pathology once the disease has progressed with more sever root damage or cauda equina syndrome. Our patients were diagnosed in a rather early course of the disease, because of easy and direct accessibility of the Iranian patients to neurosurgeons, the low price for MRI performance and increased number of MRI centers both in private and governmental centers,
Association with diabetes insidious, or calcium metabolism should be carefully evaluated.
Imaging
A good quality AP and lateral lumbar plain radiographs might show OLF as a small ossified lesion between the bases of two spinal processes. Lateral dynamic lumbar X-ray is necessary to rule out instability.
However, the exact location, the number of the affected levels and the degree of cord or cauda equina compression can be best assessed with magnetic resonance imaging (MRI) [37,38]. A typical OLF is visualized in MRI as a hypointense signal intensity mass at the level of the posterior margin of the spinal canal, both in T1 and T2-weighted images. Besides, showing the degree of canal compromise [37-40]. In order to detect coexisting or tandem OLF at other locations, whole spine MRI is quite necessary. With the aid of MRI, ossification of the yellow ligaments has been classified with respect to the number into two types; isolated and multiple types. With regard to the continuity of the lesions, multiple type itself is divided into continuous and noncontinuous sub-types.
For detection of the shape and the extent of ossified lesions, computerized tomography is the diagnostic tool of choice. On axial CT scans, the lesions are seen as ossified mass from the facet joint to the base of the spinal process either unilaterally or bilaterally and in sagittal reconstructed images, OLF is seen as an ossified mass at the posterior aspect of the spinal column at the site of ligamentum flavum besides, the shape, contour and the extent of OLF, the type of the pathology can be obtained by this diagnostic tool [37-40].
With respect to CT images, OLF is classified into five types: The lateral type, Type I, is located only laterally at the origin of the ligamentum flavum at the articular processes. The extended type, Type II, extends from the lateral origin of the ligamentum flavum to the interlaminar portion of the ligamentum flavum. The enlarged type, Type III, protrudes into the canal posterolaterally but is not fused in the midline. The fused type or type IV consists of bilateral ossified ligaments that are fused at the midline with a groove at the fusion site in the midline. Type V, the tuberous type, occurs when the fused ossified ligamentum flavum forms a “tuberous” mass posteriorly in the midline, which protrudes into the spinal canal.
Another categorization is based on sagittal configuration of OLF into round and beak type, being demonstrated both in sagittal MRI and reconstructed CT scans, according to Kuh et al. in 2006.
Associated OPLL can also be suggested in sagittal MRI, but can be confirmed with computerized tomography. Unlike the patients with OLF in the thoracic spine with a high incidence of ossification of the other spinal ligaments, such as ossification of the posterior longitudinal ligament (OPLL), ossification of this ligament remains an infrequent event in the, the OLF of the lumbar.
Treatment
Where asymptomatic cases can be closely followed, decompressive laminectomy and excision of the OLF are the main stay of surgical procedure [41-43]. The indications for surgery are cauda equina syndrome, radiculopathy or progressive neurological impairment. This can be done after induction of general anesthesia with the patient in the prone position. After exposure, intraoperative fluoroscopy should be used for correct localization of the affected levels.
The spinal process can be removed with rongeur. Subsequently, laminectomy with high speed burr should be done. Laminectomy is better to be started from the lateral side of lamina with making a longitudinal groove on both sides. The grooves should be deepened till the lateral dura mater can be identified. Laminectomy with burr should be continued till the laminas become paper thin. After piece meal removal of sound lamina, a patch of thinned lamina and OLF remains on either side of the midline. These patches should be lifted, dissected and detached from the dura with a sharp dissector. At this moment, great care is necessary not to tear the dura [41-43]. However, in some instances, dural tearing is inevitable and in infrequent situation the dura might be absent at the site of OLF. However, the incidence of dural tears and CSF leakage in OLF patients is relatively frequent and has been estimated to be from 10% to 32%. The dural tears should be closed with continuous silk and for dural defects; duraplasty with a range of materials is required, usually with placement of fascia or artificial dura. Once, tight closure was accomplished, Valsalva maneuver is necessary to confirm the integrity of the repair. Subsequently, the wound should be closed tightly in 3 layers.
Post-operatively, therapeutic lumbar puncture or short term lumbar cerebrospinal fluid drainage are recommended. Leaving the small tears unrepaired may result in continued CSF leakage pseudomeningocele formation and even meningitis [44].
Laminoplasty as an alternative option has been used in a few patients by Kawaguchi et al. in 2005, with acceptable results [22]. Laminoplasty should be done only in the patients with lumbar lordosis.
Outcome
The outcome after surgery depends on the duration of the symptoms, degree of anteroposterior diameter of the lesion and type of OLF.
As has been documented, longer the duration of the symptoms, tuberous shape OLF with marked protrusion into the spinal canal and fused type of OLF are associated with poor prognosis [45-49].
However, unlike the thoracic spine, lumbar OLFs have better prognosis. The difference in outcome between lumbar and thoracic OLF can be explained with higher resistance of the cauda equina and the roots to gradual compression, their less susceptibility to intraoperative forces derived during laminectomy, more rapid response of the cauda to decompression, higher resistance of the cauda equina to perioprative fluctuation of the blood pressure, and finally more familiarity of the neurosurgeons to lumbar laminectomy.
Conclusion
Lumbar OLF (LOLF) remains one of the rare causes of intermittent claudication or lower extremity radiculopathy. It seems that OLF is under reported in Iran, despite lack of a case series among the Iranian population.
The present case series is the first retrospective study in Iranians with ossified ligamentum flavum. Our survey showed that the clinical and radiological features of lumbar OLF in the Iranian population appear to be similar to other ethnic societies. Early diagnosis with shorter duration of the symptoms probably due to easy availability of MRI have been the cause of relatively good outcome in Iranian patients.
References
- Polgar F (1920) Uber interakuelle wirbelverkalkung. Fortschr Geb Rontgenstr Nuklearmed Erganzungsbd 40: 292-298.
- Yonenobu K, Ebara S, Fujiwara K, Yamashita K, Ono K, et al. (1987) Thoracic myelopathy secondary to ossification of the spinal ligament.J Neurosurg 66: 511-518.
- Okada K, Oka S, Tohge K, Ono K, Yonenobu K, et al. (1991) Thoracic myelopathy caused by ossification of the ligamentum flavum Clinicopathologic study and surgical treatment. Spine (Phila Pa 1976) 16: 280-287.
- Aizawa T, Sato T, Sasaki H, Kusakabe T, Morozumi N, et al. (2006) Thoracic myelopathy caused by ossification of the ligamentum flavum: clinical features and surgical results in the Japanese population. J Neurosurg Spine 5: 514-519.
- Guo JJ, Luk KD, Karppinen J, Yang H, Cheung KM (2010) Prevalence, distribution, and morphology of ossification of theligamentum flavum: a population study of one thousand seven hundred thirty-six magnetic resonance imaging scans. Spine (Phila Pa 1976) 35: 51-56.
- Yoon SH, Kim WH, Chung SB, Jin YJ, Park KW, et al. (2011) Clinical analysis of thoracic ossified ligamentum flavum without ventral compressive lesion. Eur Spine J 20: 216-223.
- Hur H, Lee JK, Lee J H, Kim JH, Soo J- Kim H, et al. (2009) Thoracic Myelopathy Caused by Ossification of the Ligamentum Flavum. J Korean Neurosurg Soc 46: 189-194.
- Kang KC, Lee CS, Shin SK, Park SJ, Chung CH, et al. (2011) Ossification of the ligamentum flavum of the thoracic spine in the Korean population. J Neurosurg Spine 14: 513-519.
- Wiseman DB, Stokes JK, Toselli RM (2002) Paraparesis in a black man brought on by ossification of the ligamentum flavum: case report and review of the literature. J Spinal Disord 15: 542-545.
- Jayakumar PN, Devi BI, Bhat DI, Das BS (2002) Thoracic cord compression due to ossified hypertrophied ligamentum flavum. Neurol India 50: 286-289.
- Ben Hamouda K, Jemel H, Haouet S, Khaldi M (2003) Thoracic myelopathy caused by ossification of the ligamentum flavum: a report of 18 cases. J Neurosurg (Spine 2) 99: 157-161.
- Rahimizadeh A (2012) Isolated proximal thoracic ossified ligamentum flavum causing paraparesis in a Caucasian: A case report and review of the literature. World Spinal Column J 3: 38-43.
- Celli P, Caroli E, Trillo G, Ferrante L (2002) Ossification of the ligamentum flavum in a Caucasian: Case report. J Neurosurg Sci46: 96-99.
- Arafat QW , Jackowski A , Chavda SV, West R (1993) Case report: ossification of the thoracic ligamenta fl ava in a Caucasian: a rare cause of myelopathy. Br J Radiol66: 1193-1196.
- Hugues PM, Philippe C, Didier S, Yves C (2005) Symptomatic ossification of the ligamentum flavum: a clinical series from the French Antilles. Spine 30: e400-e405.
- Jaffan I, Abu-Serieh B, Duprez T, G Cosnard (2006) Unusual CT/MR features of putative ligamentum flavum ossification in a North African woman. British J Radiol 79: e67-e70.
- Christiano LD, Assina R, Goldstein IM (2011) Ossification of the ligamentum flavum: a unique report of a Hispanic woman. Neurosurg Focus 30: E15.
- Akira k, Yasushi A , Nobuhiro T, Yasunobu I (1988) Hyperostotic lumbar spinal stenosis: A review of 12 surgically treated cases with roentgenographic survey of ossification of the yellow ligament at the lumbar spine. Spine11: 1308-1316.
- Weiss MH, Spencer GE (1970) Ossification of a lumbar interspinous ligament with compression of the cauda equina. J Bone Joint Surg Am 52: 165-167.
- Baba H , Tomita K, Maezawa Y, S Imura (1993) Intermittent claudication of the spinal cord due to ossification of the ligamentum flavum: A report of two cases Int Orthop17: 169-172.
- Epstein NE (1999) Ossification of the yellow ligament and spondylosis and/or ossification of the posterior longitudinal ligament of the thoracic and lumbar spine. J Spinal Disord 12: 250-256.
- Kawaguchi Y, Oya T, Abe Y (2005) Spinal stenosis due to ossified lumbar lesions. J Neurosurg Spine 4: 262-270.
- Pantazis G, Tsitsopoulos P, Bibis A, Mihas C, Chatzistamou I, et al. (2008) Symptomatic ossification of the ligamentum flavum at the lumbar spine: a retrospective study. Spine 33: 306-311.
- Yano T, Doita M, Iguchi T, Kurihara A, Kasahara K, et al. (2003) Radiculopathy due to ossification of the yellow ligament at the lower lumbar spine. Spine 28: E401-E404.
- Odate S, Shikata J, Kimura H, Amano S, Soeda T, et al. (2012) Intolerable Low Back Pain Due to Ossification of the Ligamentum Flavum at the L5– S1 Level. J Spine Neurosurg 1:2.
- Tsukamoto N, Maeda T, Miura H, Jingushi S, Hosokawa A, et al. (2006) Repetitive tensile stress to rat caudal vertebrae inducing cartilage formation in the spinal ligaments: a possible role of mechanical stress in the development of ossification of the spinal ligaments. J Neurosurg Spine 5: 234-242.
- Baba H, Furusawa N, Fukuda M, Maezawa Y, Imura S, et al. (1997) Potential role of streptozotocin in enhancing ossification of the posterior longitudinal ligament of the cervical spine in the hereditary spinal hyperostotic mouse (twy/twy). Eur J Histochem 41: 191-202.
- Li H, Jiang LS, Dai LY (2007) Hormones and growth factors in the pathogenesis of spinal ligament ossification. Eur Spine J 16: 1075–1084.
- Sakou T, Taketomi E, Matsunaga S, Yamaguchi M, Sonoda S, et al. (1991) Genetic study of ossification of the posterior longitudinal ligament in the cervical spine with human leukocyte antigen haplotype. Spine 16: 1249-1252.
- Yamamoto Y, Furukawa K, Ueyama K, Nakanishi T, Takigawa M, et al. (2002) Possible roles of CTGF/Hcs24 in the initiation and development of ossification of the posterior longitudinal ligament. Spine 27: 1852-1857.
- Yayama T, Uchida K, Kobayashi S, Kokubo Y, Sato R, et al. (2007) Thoracic ossification of the human ligamentum flavum: Histopathological and immunohistochemical findings around the ossified lesion. J Neurosurg Spine 7: 184-193.
- Maigne JY, Ayral X, Guerin-Surville H (1992) Frequency and size of ossifications in the caudal attachments of the ligamentum flavum of the thoracic spine. Role of rotatory strains in their development. Surg Radiol Anat 14: 119-124.
- Li H, Jiang LS, Dai LY (2007) Hormones and growth factors in the pathogenesis of spinal ligament ossification. Eur Spine J 16: 1075-1084.
- Galliford TM, Murphy E, Williams AJ, Bassett JH, Williams GR (2005) Effects of thyroid status on bone metabolism: a primary role for thyroid stimulating hormone or thyroid hormone? Minerva Endocrinol 30: 237-246.
- Vera CL, Cure JK, Naso WB (1997) Paraplegia due to ossification of ligament flava in X-linked hypophosphatemia: A Case Report. Spine 22: 710-715.
- Muthukumar N (2005) Ossification of the ligamentum flavum as a result of fluorosis causing myelopathy: report of two cases. Neurosurgery 56: E622.
- Hanakita J, Suwa H, Ohta F, Nishi S, Sakaida H, et al. (1990) Neuroradiological examination of thoracic radiculomyelopathy due to ossification of the ligamentum flavum. Neuroradiology 32: 38-42.
- Xiong L, Zeng QY, Jinkins JR (2001) CT and MRI characteristics of ossification of the ligamentum flava in the thoracic spine. Eur Radiol 11: 1798-1802.
- Sugimura H, Kakitsubata Y, Suzuki Y (1992) MRI of ossification of ligamentum flavum. J Comput Assist Tomogr 16: 73-76.
- Kuh SU, Kim YS, Cho YE, Jin BH, Kim KS, et al. (2006) Contributing factors affecting the prognosis surgical outcome for thoracic OLF. Eur Spine J 15: 485-491.
- Chang UK, Choe WJ, Chung CK, Kim HJ (2001) Surgical treatment for thoracic spinal stenosis. Spinal Cord 39: 362-369.
- Liao CC, Chen TY, Jung SM (2005) Surgical experience with symptomatic thoracic ossification of the ligamentum flavum. J Neurosurg Spine 2: 34-39.
- Li F, Chen Q, Xu K (2006) Surgical treatment of 40 patients with thoracic ossification of the ligamentum flavum. J Neurosurg Spine 4: 191-197.
- Rahimizadeh A, Kaghazchi M, Rahimizadeh A (2014) post-laminectomy lumbar pseudomeningocele; Report of three cases and review of the literature. World Spinal Column J 4: 103-108.
- Shiokawa K, Hanakita J, Suwa H, Saiki M, Oda M, Kajiwara M, et al. (2001) Clinical analysis and prognostic study of ossified ligamentum flavum of the thoracic spine. J Neurosurg Spine 94: 221-226.
- Miyakoshi N, Shimada Y, Suzuki T, Hongo M, Kasukawa Y, et al. (2003) Factors related to long-term outcome after decompressive surgery for ossification of the ligamentum flavum of the thoracic spine. J Neurosurg 99: 251-256.
- He SS, Hussain N, Li SH, Hou TS (2005) Clinical and prognostic analysis of ossified ligamentum flavum in a Chinese population. J Neurosurg Spine 3: 348–354.
- Inamasu J, Guiot BH (2006) A review of factors predictive of surgical outcome for ossification of the ligamentum flavum of the thoracic spine. J Neurosurg Spine 5:133-139.
- Aizawa T, Sato T, Sasaki H, Matsumoto F, Morozumi N, et al. (2007) Results of surgical treatment for thoracic myelopathy: minimum 2-year follow-up study in 132 patients. J Neurosurg Spine 7: 13-20.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi