Research Article, J Spine Neurosurg Vol: 12 Issue: 4
Outcomes of the Surgical Treatment of Lumbar Fractures with Plate-Rod System
Armando Alpizar Aguirre*, Carla Lisette Garcia Ramos, Fernando Reyes Tarrago, Laura Chavez Montiel, Luis Miguel Rosales Olivarez, Alejandro Antonio Reyes Sanchez and Carlos Robles Choez
Department of Spine Surgery, National Institute of Rehabilitation, Mexico city, Mexico
- *Corresponding Author:
- Armando Alpizar Aguirre
Department of Spine Surgery,
National Institute of Rehabilitation,
Mexico city,
Mexico;
E-mail: armandoalpizar@hotmail.com
Received date: 20 June, 2022, Manuscript No. JSNS-23-67115;
Editor assigned date: 23 June, 2022, PreQC No. JSNS-23-67115 (PQ);
Reviewed date: 07 July, 2022, QC No. JSNS-23-67115;
Revised date: 17 July, 2023, Manuscript No. JSNS-23-67115 (R);
Published date: 14 August, 2023, DOI: 10.4172/2325-9701.1000161
Citation: Aguirre AA, Ramos CLG, Tarrago FR, Montie LC, Olivarez LMR, et al. (2023) Outcomes of the Surgical Treatment of Lumbar Fractures with Plate- Rod System. J Spine Neurosurg 12:3.
Abstract
Objective: Describe surgical, clinical and radiographic outcomes in patients with lumbar fractures treated with plate rod system (Placa Barra®-SOLCO)
Study design: Observational, longitudinal, direct assignation study.
Methods: The study is designed to evaluate surgical, clinical and radiological outcomes in patients with lumbar fractures, treated by short fixation with plate rod system (Placa Barra®), without arthrodesis, removing hardware at 1-year follow-up. The clinical outcomes are evaluated by the visual analogue scale, oswestry disability index, roland morris questionnaire and short form. Radiological measures considered in this study are vertebral body height of fractured vertebra, kyphosis angle and segmental motion.
Results: 8 patients were included in the study, with a mean age of 39.5 ± 18.26 years old. The mean surgery time was 123.5 ± 43.32 minutes and trans operatory blood loss of 343 ml ± 304.06 ml. No trans operatory complications were reported. The correction of kyphotic angle was 14.72° ± 9.04° and the correction lost was 7.15° ± 11.86°. Mean vertebral body height correction was 29.75° ± 12.58% and correction lost was 3.88° ± 6.98% in follow up (p=0.013). The spine segmental motion found was 5.03° ± 1.3°.
Conclusion: Fixation of lumbar fractures with plate rod system (Placa Barra®) without arthrodesis gives a kyphosis correction of 15°, with a 4° correction loss at a 1-year follow-up. Segmental mobility after material removal stayed at normal ranges.
Keywords: Thoracolumbar fracture, Spine fracture, Sagittal alignment, Spine segmental mobility
Introduction
Thoracic and lumbar spine fractures represent 54%-90% of all spine fractures, with an estimated incidence of 700,000 fractures per year around the world. In Mexico incidence has been reported as 1.79 cases per 100000 persons and affects in most cases economically active population. Clinical complications have been described: Paralysis, chronic pain, deformity and lost functionality, that compromise life quality of these patients [1].
The treatment of thoracolumbar fractures can be divided into conservative or surgical management. The biomechanical stability and neurological state, orientate to determine which treatment is indicated for the patient but can be controversial if doubtful biomechanical stability is presented without neurological compromise. Independently of therapeutic management, some basic principles must be followed: Early mobilization of the patient, a stable spine, no pain, alignment, preserving neurological function and reestablishing dynamic function of the spine. All previously described can be obtained by posterolateral fixation (with or without decompression), anterior decompression and fixation or by mixed procedures.
When posterior fixation is indicated, transpedicular screws and rods constructs are used, which can be o not done with posterolateral arthrodesis. Authors have proposed that arthrodesis protects fixation systems and diminishes the risk of fatigue of material subjected to multiple cycles of movement and improves radiographic parameters. Nevertheless, real value as adjuvant of the construct has been questioned, because of pseudoarthrosis risk and diminished mobility on an injured segment that causes more stress on adjacent segments and is traduced in low back pain and degenerative changes in adjacent segments. Multiples metanalysis has shown favorable outcomes in fixation without arthrodesis [2].
The general recommendation in spine fractures AO type B is to fixate and arthrodesis nevertheless, the current tendency is to do a posterolateral fixation in patients with neurological integrity and isolated bone lesion. The actual evidence level cannot give strong recommendations, new studies are required to study security and efficiency in long term. AO type C fractures require long fixation with arthrodesis because of instability.
Maintaining mobility of fracture segment at mid and long term, in no arthrodesis context and removing system when bone consolidation has been reached and has been incorporated as a principal fundament in spinal reconstructive surgery. Lost correction of fracture segment is considered inevitable even with arthrodesis or long instrumentations [3].
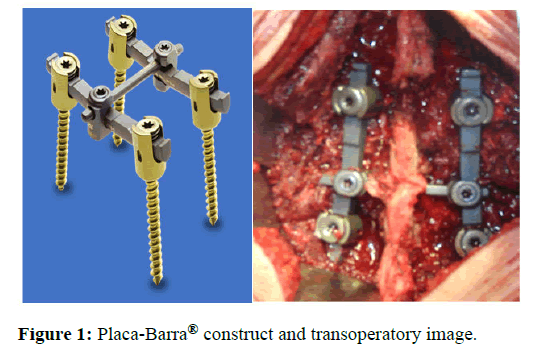
Innovation in osteosynthesis materials is focused on minimally invasive surgery, not taking into consideration the totality of therapeutic objectives in thoracolumbar fractures. Anthropometric difference between the Mexican population and first world countries, modifications on osteosynthesis material have been evaluated. In 1991 INO system was developed for bilateral posterior fixation of the thoracolumbar spine, with plates and transpedicular screws, with nut and locknut. This system showed biomechanical and clinical efficiency in thoracolumbar fracture treatment. This system was semirigid (metal-metal-bone) and didn’t need to be accompanied by arthrodesis, this was because no modification on the spine elasticity module was performed. With the finality of improving this implant for lumbar spine fixation, a plate rod system (Placa Barra®-SOLCO) was developed. The objective of this study is to describe the surgical, clinical and radiological outcomes of the Placa Barra® system in lumbar fractures (Figure 1).
Materials and Methods
Observational, prospective, longitudinal, deliberated intervention study, done in patients with lumbar fracture diagnosis, treated by transpedicular reduction, bone graft in the fracture site and posterior fixation with plate rod system (Placa Barra®) without arthrodesis in older than 18 years old, with preoperative and postoperative radiographs, tomography, magnetic resonance imaging, clinical expedient, pain and functionality scales and system removal at 1 year of follow up. Patients with open wound fracture, previous thoracolumbar surgery, bone metabolic diseases and complete spine cord injury were excluded [4].
Patients in the study were admitted to our spine surgery service, variables considered were: Age, gender, weight, height, Body Mass Index (BMI), fracture level, pain intensity evaluated by Visual Analogue Scale (VAS), surgery time (minutes), surgery total blood loss (milliliters), disability evaluated with Oswestry disability scale and Roland Morris scale and functionality with SF 36 questionnaire, spine cord injury by ASIA scale, all considered in preoperative, postoperative and posterior of plate rod system removal, also complications were analyzed.
Anteroposterior and lateral lumbar spine radiographs were taken at the emergency room, kyphotic angle, wedge angle, vertebral height loss and adjacent (cephalic and caudal) inter somatic space height were measured. Complementary studies were done with axial tomography and magnetic resonance imaging. All these fractures were classified with AO, TLICS and McCormack. Informed consent was explained and signed by patients and surgery was performed by the same surgeon [5].
Post operatory imaging consisting of standing anteroposterior and lateral radiographs were taken after 24 hours of surgery; regional kyphosis and vertebral height were measured, also variables previously described were measures. Clinical controls and radiographical control were taken at three, six and twelve months and after plate rod system removal was performed at 1 year.
After plate rod system removal same variables were measured, preand post-operative correction of regional kyphosis and vertebral height were compared. Segmental mobility was measured by the angular change in regional kyphosis in dynamic lateral radiographs (flexion and extension), also the adjacent level was considered in the evaluation.
Clinical and radiological examination
Oswestry disability index, Roland Morris (RM), SF 36 scale and analogue visual scale were obtained and analyzed in preoperatory, post-operatory and after plate rod system removal. The radiographic evaluation was done in anteroposterior and lateral radiographs: Kyphosis angle was measured using the Cobb method between the superior platform of the caudal vertebra and the inferior platform of the cephalic vertebra in relation to the injured level. The same method was used to measure de wedge angle of the injured vertebra.
Vertebral body height at injury level (divided in anterior, mid and posterior segment), inter somatic space at cephalic and caudal level, was measured in millimeters (mm). Height loss of vertebral bodies and protrusion of body fragments to spine canal were obtained following Mumford and Will method in percentage (%) [6].
Kyphosis correction in the injured segment was calculated as the difference between pre-operatory and post-operative kyphosis angles. Kyphosis correction loss was calculated by measuring the difference between post-operatory kyphosis and kyphosis after spine hardware removal. Segmentary mobility in the injured segment was examined after the plate rod system was removed, measured by the difference between kyphosis changes in flexion and extension radiographs, also mobility in intersomatic cephalic and caudal spaces were measured in flexion and extension obtaining changes in intersomatic mean angles. All measurements were done and analyzed by the same spine surgeon [7].
Surgery technique
General anesthesia was practiced in all patients, positioned in dorsal decubitus in operation table, gel spacers were positioned at thorax and pelvis level. Posterior mid lumbar approach was performed and dissection performed in midline until posterior arch, followed by subperiosteal dissection, vertebral posterior elements were exposed and transpedicular screws were positioned bilateral in cephalic and caudal level, fluoroscopic control was made. Fracture reduction was made by the transpedicular method and bone graft was positioned, the superior platform was reestablished and the system was positioned. A drain was positioned, and closure was performed [8].
Results
8 patients were examined, 3 female (37.5%) and 5 males (62.5%), with a relation of 1.6:1. The mean age was of 39.5 years (SD 18.26), the youngest patient was 21 years old and the oldest 69 years old. Mean weight was 70.75 kg (50 kg-98 kg); mean height of 1.66 m (1.56 m-1.78 m); mean body mass index was 25.5 kg/m2 (20.33 kg/ m2-31.6 kg/m2) [9].
Fracture etiology was presented as the following description: 25% of a car accident (2/8) and 75% (6/8) fall from height. 12% of fractures had an associated vertebral fracture and 25% presented bone fracture out of the spine column. According to AO classification, 62.5% (5/8) were AO A4, 25% (2/8) were AO type B2 and 12.5% (1/8) AO type C.
Spine level of L1 was compromised in 12.5% (1/8), L1L2 segment compromised in 25% (2/8), L2 level compromised in 12.5% (1/8) and 12.5% (1/8) compromised L3L4 level. The mean TILICS score was 5 points (SD 2.78, with the lowest score of 2 and highest of 8). McCormack scale had mean punctuation of 5.88 (5-8, SD 1.25). ASIA neurological scale presented as following: 1 patient with ASIA B (12.5%) and 87.5% ASIA E scale [10].
Surgical outcomes
Mean surgery time was of 123.5 minutes (SD 43.32, 60-198 minutes), mean anesthetic time of 160 minutes (SD 65.03, 90-230 minutes). Mean blood loss in surgery was 343 ml (SD 304.06 ml, 100 ml-1000 ml).
Clinical outcomes
The initial mean VAS was 7.38 (SD 0.74, range 6-8), 50% (4/8) had pelvic irradiation of pain. On follow up mean VAS was 1.75 points (SD 1.58). ODI preoperatory mean value was 57.25% (SD 10.47) after spine implant removal mean ODI was 15.75% (SD 12.49%). RM reported a mean of 13.38 points (SD 3.38) at preoperatory and after implant removal mean of 6.5 points (SD 4.93), having statistical significance.
In SF 36 questionnaire patients at the preoperatory stage had a mean physical exam of 29.57 points (SD 5.5) and a mental exam of 47.5 points (SD 9.67), on follow-up after removal of plate rod system, physical exam averaged 45.5 points (SD 9.29) and mental exam average 53.38 points (SD 4.1), having statistical significance (Table 1).
| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | Total M (SD) | p-value |
|---|---|---|---|---|---|---|---|---|---|---|
| Age, years | 42 | 29 | 60 | 24 | 48 | 21 | 23 | 69 | 39.5 (18.26) | - |
| VAS pre, pts | 7 | 8 | 6 | 7 | 8 | 7 | 8 | 8 | 7.38 (0.74) | 0.0001* |
| VAS post, pts | 5 | 2 | 3 | 1 | 1 | 1 | 0 | 1 | 1.75 (1.58) | |
| SF-36 PCS, pre % | 32 | 30 | 24 | 28 | 26 | 34 | 40 | 24 | 29.75 (5.5) | 0.001* |
| SF-36 PCS, post % | 44 | 40 | 45 | 42 | 29 | 50 | 58 | 56 | 45.50 (9.29) | |
| SF-36 MCS, pre % | 48 | 54 | 28 | 40 | 46 | 52 | 54 | 58 | 47.50 (9.67) | 0.106 |
| SF-36 MCS, post % | 52 | 54 | 49 | 58 | 52 | 48 | 54 | 60 | 53.38 (4.10) | |
| ODI, pre % | 60 | 58 | 40 | 64 | 72 | 58 | 62 | 44 | 57.25 (10.47) | 0.0001* |
| ODI, post, % | 42 | 14 | 10 | 18 | 22 | 8 | 0 | 12 | 15.75 (12.49) | |
| RM, pre, pts | 12 | 10 | 18 | 14 | 15 | 13 | 17 | 8 | 13.38 (3.37) | 0.016* |
| RM, post, pts | 18 | 6 | 7 | 3 | 5 | 2 | 6 | 5 | 6.50 (4.92) | |
| Surgery time, min | 120 | 120 | 60 | 198 | 75 | 120 | 145 | 150 | 123.5 (43.32) | - |
| Anesthetic time, min | 150 | 180 | 90 | 210 | 110 | 150 | 160 | 230 | 160 (65.03) | - |
| Trans operatory Bleed, cc | 250 | 100 | 100 | 4000 | 1000 | 100 | 500 | 300 | 343 (304.06) | - |
| Wedge angle pre,° | 21.8 | 17.2 | 15.5 | 29.1 | 9.6 | 20.2 | 3 | 25.6 | 17.75 (8.47) | 0.002* |
| Wedge angle final,° | 14.7 | 4.7 | 8.9 | 9.4 | 1.9 | 3.9 | 1.5 | 9.1 | 6.76 (4.53) | |
| Initial segmentary kyphosis° | 10.7 | 5.1 | 13.2 | 22.9 | -12.5 | 9.5 | -28.8 | 14.2 | 4.28 (16.77) | 0.536 |
| Final segmentary kyphosis,° | 28.3 | 3.4 | 28.8 | 4.9 | 15.6 | 6.1 | -26.2 | 2.3 | 7.90 (17.48) | |
| Final segmentary mobility,° | 3.6 | 6.3 | 4.8 | 5.2 | 5.2 | 5.1 | 3 | 7 | 5.02 (1.29) |
Note: M=Mean, SD=Standar Deviation, * p<0.05
Table 1: The statistical significance of patients at the preoperatory stage.
Radiological outcomes
The mean preoperatory kyphosis angle was 1.19° (SD 16.72, 26.7°-13.5°), after surgery mean angle of 13.53° (SD 10.13), with a mean kyphosis angle correction of 14.71° (SD 9.04). After implant removal mean kyphosis angle was -6.38° (SD 11.81, 28.1°-25.4°). Correction loss on injury level averaged 7.15° (SD 11.86).
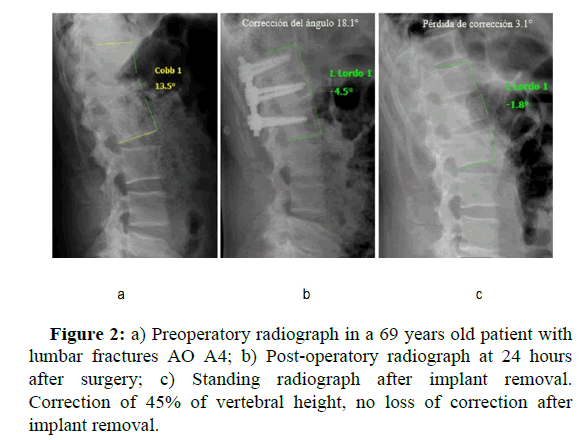
Vertebral height was also evaluated, in preoperatory mean vertebral height at fracture level was 43% (SD 17.01), after surgery 13.63% (SD 6.91) and after implant removal of 16.63% (SD 7.73); vertebral height correction reached was 29.75% (SD 12.58), nevertheless, at the end of follow up, we found a loss in vertebral height of 3.38% (SD 6.98) (Figure 2) [11].
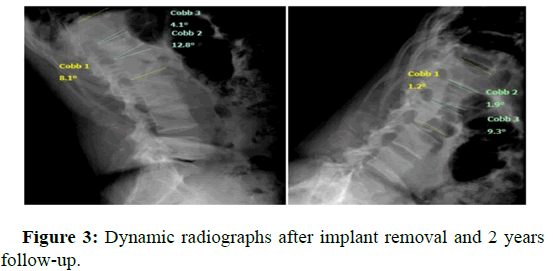
One patient presented implant fatigue at follow-up (five transpedicular screws) at 37 months after surgery was practiced. The patient did not come to implant removal at 1 year follow up, had a fracture AO type B2, TLICS and McCormack of 7 points, Kyphosis correction was of 21.2° and at follow up a kyphosis correction loss of 35.9°. Mean movement of cephalic inter-somatic space of fractured level after implant removal was 3.85° (SD 2.18) and caudal of 5.69° (SD 2.37). Mean segmentary mobility averaged 5.03° (SD 1.3, 3°-7°) (Figure 3) [12].
Discussion
The objective of surgical treatment in thoracolumbar fractures is to preserve neurological function, correct deformity, reestablish and maintain long-term spinal alignment, reestablish dynamic and protective function of the spine, avoid intense pain and early mobilization. For treatment election not only injury personality and neurological state are taken into count, but the clinical state like pain and disability must be considered.
Some authors propose that arthrodesis protects construct and prevent fatigue of material that is brought under multiple cycles of movement as the patient becomes aged and improves radiographical parameters; nevertheless, its coadjutant valor has been put on question because it increases surgery time and trans operatory blood loss, decreases the mobility of injured segment and is associated with the complication of donator site [13].
Not fixating a fractured vertebra has been a surgical technique, but stabilizing the rest of the spine adjacent segments to fractures has been done to decrease neurological damage but is associated with an increased risk of failure. In clinical and biomechanical studies fixating injured vertebrae with trans pedicular screws has been observed; described a recent metanalysis and recommend this technique (fixating injury level, one cranial vertebra and one caudal vertebra to injury level), a lower risk of failure was obtained and a better correction of the segment was obtained at mid and large term.
Implant removal is suggested at one-year post-operatory, in patients without arthrodesis to prevent material failure or fatigue. Chou et al., recommends that implant removal can or cannot be necessary after fixation without arthrodesis, but about 36.3% of the patients presented fatigue of implants, no statistical significance was found in radiological and functional parameters comparing the group with implant removal and without removal (p<0.05). Nevertheless, removal of implants even in arthrodesis patients increases the mobility angle in the injured segment from 1.6° ± 1.5° to 5.8° ± 3.0° at 2 years follow up. This provides better functionality of the spine.
Zhang et al, studied the effectivity of monoaxial screw fixation combines with polyaxial screw fixation in fractured vertebra compared with only polyaxial screws in thoracolumbar fractures. No statistical significance was found at final follow up in pain scale (p=0.774), the radiological height of fracture level, Cobb angle, sagittal angle and correction angle did not have statistical significance when using monoaxial screws (p<0.05), nevertheless correction loss did not present statistical significance (p>0.05).
With this background, spine functional surgery of thoracolumbar fractures with plate rod system (Placa Barra®) is proposed doing a segmentary fixation with transpedicular monoaxial screws including fractures level, without arthrodesis and removal of implant 12 months after fixation.
Wang et al., reported that no arthrodesis group surgery timeaveraged 162 ± 44.4 minutes (70-300) and blood loss of 303 ± 148 milliliters (100 ml-600 ml), being comparable with our results (123.5 ± 43.3 minutes and blood loss of 343.75 ± 304.06 ml).
Metanalysis have reported in no arthrodesis groups less surgery time (WMD=53.85, 95% CI=37.38-70.32; p<0.05) and less blood loss (WMD=220.98, 95% CI=140.19-301.77; p<0.05) than in patients treated with fusion. When the autologous graft is used, obtaining graft increases surgery duration and morbidities of the donor site. Posterior instrumentation with arthrodesis is a more complex and invasive procedure that does not gives better clinical or radiological outcomes compared to no arthrodesis.
Compared the difference between mean VAS in fusion and no fusion groups of 0.1 points (95% CI-0.31-0.51; p=0.63; I2=0), being worse in the fusion group. This reflects that arthrodesis and no arthrodesis can reach similar clinical outcomes; this supports our results and indication to no fusion [14].
Chou et al, demonstrated a correction loss in the arthrodesis group of 10° and 12° in no arthrodesis groups, but no statistical significance was found (p>0.05). In our study we found a mean kyphotic angle correction of 14.71° ± 9.04° and a correction loss at final follow up of 7.15 ± 11.86° (range 0.1°-35.9°), also compared with Wang et al results of 8.3 ± 3.4°. Nevertheless, when the implant presented fatigue, correction loss of 35.9° was found, increasing the average of the group. Large-term follow-up of these patients must be done, to compare it with RCT with a long-time follow-up. In Tang et al study correction loss at final follow up was 10.1%, also in other studies described as 19.2% ± 13.9%, nevertheless, Wang et al, show a correction loss of 3.6% ± 4.4%. In metaanalysis that compare arthrodesis with no arthrodesis, no statistical significance is shown in kyphotic angle preoperatory, post-operatory and final follow up, also no statistical significance in the correction of fracture and loss in vertebral height (p>0.05). Vertebral height correction in this study averaged 29.75% ± 12.58% with a correction loss of 3.88% ± 6.98% at final follow-up, with statistical significance between these measures (p=0.013), showing the important difference with literature.
The only radiological parameter that showed statistical significance was segmentary mobility, this was examined in two studies and suggest that mobility was conserved in no arthrodesis group between 4.2 and 4.8° ± 2.35°, even at 10 years follow, not showing instability (WMD=-3.49, 95% CI=4.19-2.80; p<0.005; 12=0%). This was confirmed by us in this study with a mean 5.03° ± 1.3° in segmentary mobility at final follow-up. This segmentary mobility principal contributor was a caudal intervertebral disc with an average of 5.69° ± 2.37° (not commonly injured in fracture) and a cephalic intervertebral disc with an average of 3.85° ± 2.18°. This result must be taken into consideration with precaution and studies with a bigger population must be done to confirm [15].
Possible advantages of the plate rod system can be due to its angulation of 14° in lordosis and the rigidity of implant that maintains even in the distraction of vertebral body fractures and in all bone, segment allowing consolidation and adequate perfusion to the intervertebral disc. This is previously corroborated in the previous Placa INO. One limitation exists, the implant can only be used in the lumbar spine. This study has limitations. First, the number of patients included is small and by being no comparative study its evidence level is low. Studies with small samples tendency to up estimate clinical effects. Second, no long-term follow-up after removal of implants has been done.
A patient (12.5%) of the sample did not accomplish indication of implant removal and at 3 years follow-up had fatigue of implant (rupture of 5 screws), presented clinical symptoms, had a correction loss of 35.9°. Previous studies demonstrate that no arthrodesis increases the risk of implant failure and increases kyphosis from 9%-54% in long-term follow-up. Nevertheless, implant failure is comparable in arthrodesis and no arthrodesis groups without statistical significance (p<0.05), this reports in LAN metanalysis [16].
Conclusion
This functional technique can preserve segmentary mobility and decreases loss of vertebral body height correction. This implant can accomplish therapeutic objectives in thoracolumbar fractures, restructuring anatomy and reestablishing functionality. A comparative long-term study is needed to examine the preservation of segmentary mobility and vertebral height in lumbar fracture treatment.
References
- Wang H, Zhang Y, Xiang Q (2012) Epidemiology of traumatic spinal fractures: Experience from medical university-affiliated hospitals in Chongqing, China, 2001-2010. J Neuro Spine 17: 459-468.
[Crossref] [Google Scholar] [PubMed]
- O Boynick CP, Kurd MF, Darden BV (2014) Timing of surgery in thoracolumbar trauma: Is early intervention safe? Neurosurg Focus 2: E7.
[Crossref] [Google Scholar] [PubMed]
- Cisneros F, Hurtado A (2003) Incidence of traumatic vertebral lesions in the spine surgery service of a concentration hospital of the social security system. Mexican Orthop Act 17: 292-297.
- Wood K (2014) Management of thoracolumbar spine fractures. Spine J 14: 145-164.
[Crossref] [Google Scholar] [PubMed]
- Joaquim AF, Patel AA (2013) Thoracolumbar spine trauma: Evaluation and surgical decision making. J Cranio Vert Spine 4: 3-9.
[Crossref] [Google Scholar] [PubMed]
- Vaccaro AR, Oner C, Kepler CK, Dvorak M, Schnake K, et al. (2013) AO Spine spinal cord injury and trauma knowledge forum. AO Spine thoracolumbar spine injury classification system: Fracture description, neurological status and key modifiers. Spine 38: 2028-2037.
[Crossref] [Google Scholar] [PubMed]
- Vaccaro AR, Zeiller SC, Hulbert RJ, Anderson Pa, Harris M, et al. (2011) Thethoracolumbar injury severity score: A proposed treatment algorithm. J Spinal Disord Tech 18: 209-215. [Crossref]
[Google Scholar] [PubMed]
- Joaquim AF, Fernandes YB, Cavalcante RC, Fragoso RM, Honorato DC, et al. (2011) Evaluation of the thoracolumbar injury classification system in thoracic and lumbar spinal trauma. Spine J 36: 33-36.
[Crossref] [Google Scholar] [PubMed]
- Oner FC, Ramos LMP, Simmermacher RKJ, Kingma PT, Diekerhof CH, et al. (2002) Classification of thoracic and lumbar spine fractures: problems if reproducibility. A study of 53 patients using CT and MRI. Euro Spine J 11: 234-245.
[Crossref] [Google Scholar] [PubMed]
- Lu DC, Lau D, Lee JG (2010) The Transpedicular approach compared with the anterior approach: An analysis of 80 thoracolumbar corpectomies. J Neurosurg Spine 12: 583-591.
[Crossref] [Google Scholar] [PubMed]
- Parker JW, Lane JR, Karaikovic EE, Gaines RW (2000) Successful short-segment instrumentation and fusion for thoracolumbar spine fractures: A consecutive 41/2-year series. Spine J 25: 1157e70.
[Crossref] [Google Scholar] [PubMed]
- Yung AW, Thng PL (2011) Radiologicaloutcomeof short-segment posterior stabilization and fusion in thoracolumbar spine acute fracture. Ann Acad Med Singap 40: 140e4. [Crossref]
[Google Scholar] [PubMed]
- Hwang JH, Modi HN, Yang JH, Kim SJ, Lee SH, et al. Short segment pedicle screw fixation for unstable T11-L2 fractures: With or without fusion? A three-year follow-up study. Acta Orthop Belg 75: 822e7. [Crossref]
[Google Scholar] [PubMed]
- Dai LY, Jiang LS, Jiang SD (2009) Posterior short-segment fixation with or without fusion for thoracolumbar burst fractures: A five to seven-year prospective randomized study. J Bone Joint Surg Am 91: 1033e41.
[Crossref] [Google Scholar] [PubMed]
- Wang ST, Ma HL, Liu CL, Yu WK, Chang MC, et al. (2006) Is fusion necessary for surgically treated burst fractures of the thoracolumbar and lumbar spine? A prospective, randomized study. Spine 31: 1724e31.
[Crossref] [Google Scholar] [PubMed]
- Yang H, Shi JH, Ebraheim M, Liu X, Konrad J, et al. (2011) Out come of thoracolumbar burst fractures treated with indirect reduction and fixation without fusion. Eur Spine J 20: 380e6.
[Crossref] [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi