Editorial, Analg Resusc Curr Res Vol: 6 Issue: 1
Paediatric Anterior Mediastinal Mass: A Night Mare for the Anaesthesiologist & the Need for a Systematic Evidence Based Approach towards Management of Anterior Mediastinal Mass in Paediatric Population
Sandeep Kumar Kar*
Department of Cardiac Anaesthesiology, Institute of Postgraduate Medical Education and Research, Kolkata, India
*Corresponding Author : Sandeep Kumar Kar
Assistant Professor, Cardiac Anaesthesiology, Institute of Postgraduate Medical Education and Research, Kolkata, India
Tel: 9477234900
E-mail: sndpkar@yahoo.co.in
Received: July 05, 2017 Accepted: July 07, 2017 Published: July 12, 2017
Citation: Kar SK (2017) Paediatric Anterior Mediastinal Mass: A Night Mare for the Anaesthesiologist & the Need for a Systematic Evidence Based Approach towards Management of Anterior Mediastinal Mass in Paediatric Population. Analg Resusc: Curr Res 6:1. doi:10.4172/2324-903X.1000e108
Abstract
Mediastinal masses have always posed as a nightmare even for the skilful anaesthesiologists. The compression effects, the proximity to major vascular and airway structures, the complex surgical approaches has altogether made both the diagnostic and therapeutic procedures a high risk event. The scenario is more troublesome if the patient is an infant or child. The practice of paediatric thoracic anaesthesia is challenging and paediatric anterior Mediastinal masses have always emerged as night mare for the anaesthesiologists. The ability to envision emerging complications arising out of the anaesthesia procedure or induction and thereby formulation of counteractive resuscitative measures forms the corner stone of safe anaesthesia practice.
Keywords: Mediastinal masses; Anterior mediastinum
Mediastinal masses have always posed as a nightmare even for the skilful anaesthesiologists. The compression effects, the proximity to major vascular and airway structures, the complex surgical approaches has altogether made both the diagnostic and therapeutic procedures a high risk event. The scenario is more troublesome if the patient is an infant or child.
The practice of paediatric thoracic anaesthesia is challenging and paediatric anterior Mediastinal masses have always emerged as night mare for the anaesthesiologists. The ability to envision emerging complications arising out of the anaesthesia procedure or induction and thereby formulation of counteractive resuscitative measures forms the corner stone of safe anaesthesia practice.
Pediatric patients are unique in the sense that they have small thoracic cavity thereby increasing the incidence of cardiovascular and airway catastrophic conditions in the presence of Mediastinal mass in the anterior mediastinum, due to kinking of the great vessels and compressive effects of the mass on the airway. These patients have low functional residual capacity and total lung volume; both of them get drastically reduced in the presence of anterior mediastinal mass. Pediatric patients have heart rate dependent cardiac output and are more susceptible to hypoxic cardiac arrest. A large epiglottis serves as a hindrance to qualitative laryngoscopic view. All these in a cumulative fashion add to the difficulty in anaesthesia induction in paediatric patients, especially in the presence of large anterior mediastinal mass. Therefore time to secure the airway and establish adequate oxygenation becomes a challenging task on the part of the anaesthesiologist.
Preoperative Anaesthesia check-up visit performed by the anaesthesiologist provides valuable information regarding the anaesthesia management plan in paediatric patients with anterior mediastinal masses. In this pre-operative anaesthesia visit, the anaesthesiologist not only clinically assess the patient, but the child’s mother gives the anaesthesiologists definitive clues about the preferred decubitus adopted by the child to maximise airflow in such air flow limiting conditions. These clues are vital in resuscitative and rescue measures adopted by the anaesthesiologist in case of inadvertent airway related problems arising due to compressive effects of the anterior mediastinal mass on trachea and great vessels.
Two new terms coined by the author need adequate explanation as they form the basic principle of airway management and play a pivotal role in airway rescue in case of airway and hemodynamic problems encountered in anaesthesia induction of paediatric patients with anterior mediastinal mass. The first term being “Position of maximum airway patency” and the second term being “Position of airway rescue”. Valuable information about the position of maximum airway patency is conveyed from the choice of decubitus adopted by the child, this being a nature taught process so as to maximise air entry into the respiratory system, in order to ensure adequate oxygenation. If the child is too small to move to such a position by himself, the mother knows best at which position, the obstructive respiratory symptoms of the child is best relieved and thereby work of breathing is minimised. The information regarding decubitus of choice is recorded and noted by the anaesthesiologist and when the child is put to this position by the anaesthesiologist, for the rescue of the airway, in case of any inadvertent airway or great vessel compression symptoms arise during the process of anaesthesia induction or after induction in the immediate intra-operative period. This position is termed as Position of airway rescue. So the terms basically imply the decubitus of choice but depending upon the situation, when the anaesthesiologist put the patient in the position of maximum airway patency as a resuscitative measure, it is termed as position of airway rescue. However in case of intra-operative or preoperative great vessel compression by the anterior mediastinal mass the patient is put in lateral position or lifting force is applied by the surgeon on the mediastinal mass with the help of suitable retractors to minimise the compressive effects.
Flow volume loop offer some information about the behaviour of mediastinal mass with positional change and a rough estimate of air way compressive effects, which in adults classically shows a mid-expiratory plateau in moving the patient from upright to supine position. However paediatric patients are poor candidates for flow volume loop assessment of gravitational dependency and compressibility effects of mediastinal mass on the airway and the great vessels.
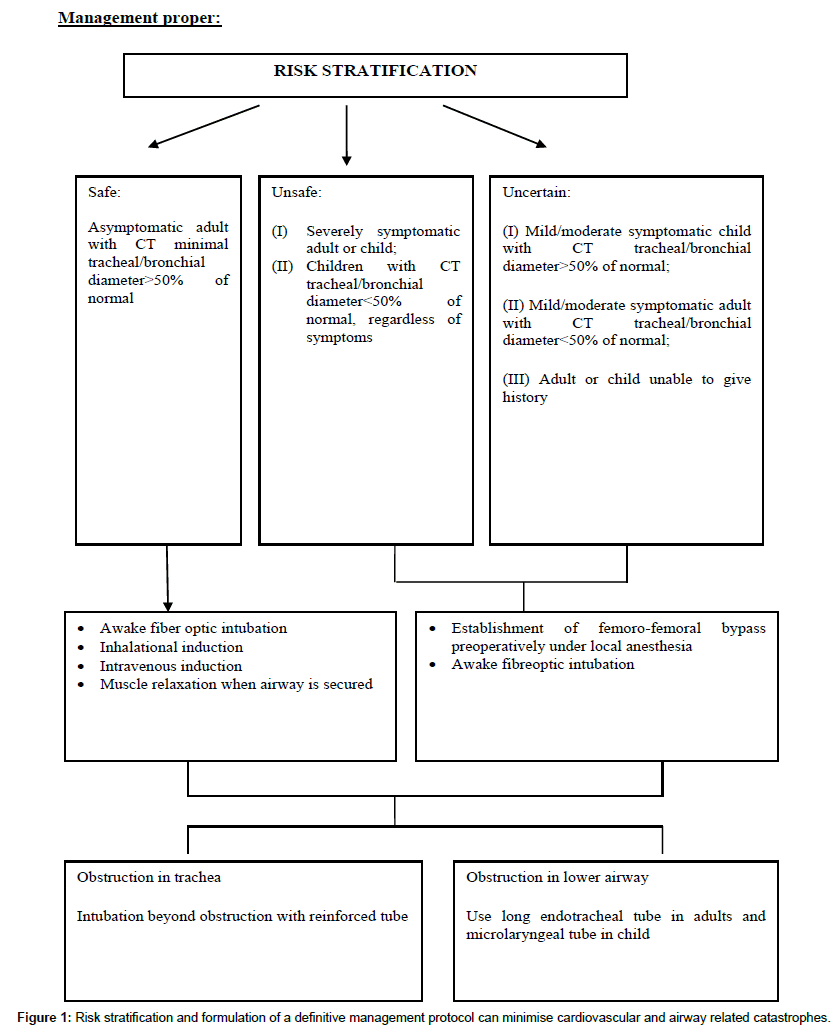
Risk stratification [1] and formulation of a definitive management protocol can minimise cardiovascular and airway related catastrophes as shown in Figure 1. The difficult airway algorithm of American society of anaesthesiologists is not of much help in airway management of paediatric patients with anterior mediastinal masses as the airway obstruction occurs more distally and the very basic design of the difficult airway algorithm is based on the concept of difficulty of visualization of the larynx. The primary option of air way rescue and maintaining adequate oxygenation is effected by airway stenting which is a cumbersome process in the paediatric age group. There has been a long controversy regarding the role of cardiopulmonary bypass in management of mediastinal mass. Recent studies have clearly indicated that ‘standby’ cardiopulmonary bypass is not a good option for paediatric patients with anterior mediastinal mass. In case of emergency even in presence of a primed bypass circuit, experienced technician and staffs, it will require at least 5-10 min before adequate oxygenation can be ensured within which irreversible neurological damage may ensue [2].
Patients with severe positional symptoms due to airway or cardiovascular compression cannot be safely given induction of general anaesthesia, even with maintenance of spontaneous ventilation, unless an alternative technique to maintain oxygenation or circulation (extracorporeal membrane oxygenation or cardiopulmonary bypass) has been established.” Alternate mode of oxygenation usually provided by a femoro-femoral bypass instituted under local anaesthesia [3-6].
In case of cystic mediastinal masses preoperative image guided aspiration is advisable to minimise compressive symptoms and in case of neoplastic mediastinal masses, empirical chemotherapy may be instituted. Empirical chemotherapy doesn’t affect tissue biopsy and histopathology findings, if biopsy sample is taken within seventy two hours of chemotherapy. The process of acquiring pathological tissue for biopsy is another anaesthetic challenge. If a patient with mediastinal mass is posted for a diagnostic biopsy, the authors insist on regional anesthesia technique. However, it may be assisted by cautious use of sedation, either with inhalation anesthetics (preferably sevoflurane) [7] or intravenous short acting agents (such as Dexmeditomedine infusion or titrated dose of propofol-ketamine). The rationality behind this technique is biopsy comes with all the deleterious effects of anaesthesia on the airways and great vessels (compressive effects due to the anterior mediastinal mass); and adding to the trouble the mediastinal mass remains in situ after the biopsy procedure is over, making the postoperative period stormy and risk prone.
Adequate imaging must be done to quantify the extent of compressive effects and the effective airway available for oxygenation and plan strategies as per the findings of the images obtained. Therefore a systemic and algorithmic approach, proper risk stratification quantified by adequate imaging and using extracorporeal circulation for establishment of oxygenation electively in selective cases and not as an rescue option or standby can minimise anaesthesia and surgery related complications in paediatric anterior mediastinal masses.
Acknowledgement
The author acknowledges his sincere thanks to Professor Anupam Goswami, Head of the Department of Cardiac anaesthesiology, Institute of Postgraduate Medical education & Research ,Kolkata for providing invaluable suggestions and ideas in structuring this editorial.
References
- Kar SK, Ganguly T, Dasgupta CS, Goswami A (2014) Cardiovascular and airway considerations in mediastinal mass during thoracic surgery. J Clin Exp Cardiol 5: 354.
- Gothard JW (2008) Anesthetic considerations for patients with anterior mediastinal masses. Anesthesiol Clin 26: 305-314.
- Kaplan JA, Slinger PD (2003) Thoracic anesthesia: Anesthesia for esophageal and mediastinal surgery. (3rd Edn), Churchill Livingstone, Elsevier, Philadelphia.
- Slinger PD, Campos JH (2014) Anesthesia for thoracic surgery. Miller’s anesthesia. (8th edtn), Elsevier Saunders, Philadelphia.
- Slinger P, Karsli C (2007) Management of the patient with a large anterior mediastinal mass: Recurring myths. Curr Opin Anaesthesiol 20: 1-3.
- Lalwani P, Chawla R, Kumar M, Tomar AS, Raman P (2013) Posterior mediastinal mass: Do we need to worry much? Ann Card Anaesth 16: 289-292.
- Chait P, Rico L, Amaral J (2005) Ultrasound guided core biopsy of mediastinal masses in children. Pediatr Radiol 35: s76.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi