Research Article, J Trauma Rehabil Vol: 1 Issue: 1
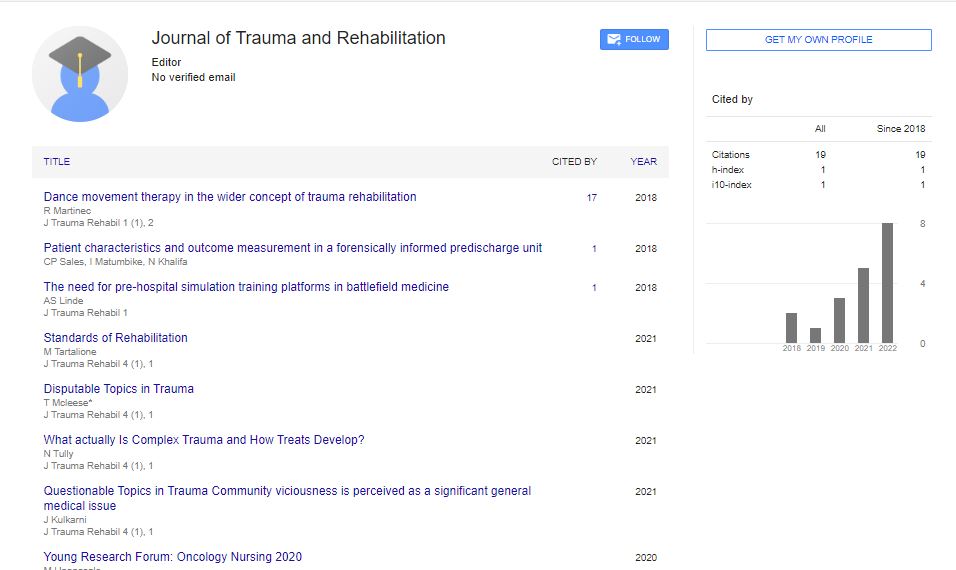
Patient Characteristics and Outcome Measurement in a Forensically Informed Predischarge Unit
Christian P Sales1,2*, Itai Matumbike1 and Najat Khalifa1,2
1Wells Road Centre, Nottinghamshire Healthcare NHS Foundation Trust, Nottingham, UK
2Institute of Mental Health, University of Nottingham School of Health Sciences, Nottingham, UK
*Corresponding Author : Christian P Sales
Institute of Mental Health, University of Nottingham School of Health Sciences, Nottingham, UK
Tel: +44 (0)115 823 0812
E-mail: Christian.sales@nottshc.nhs.uk
Received: January 17, 2018 Accepted: April 24, 2018 Published: April 30, 2018
Citation: Sales CP, Matumbike I, Khalifa N (2018) Patient Characteristics and Outcome Measurement in a Forensically Informed Pre-discharge Unit. J Trauma Rehabil 1:1.
Abstract
Purpose
This study sought to describe the demographic and clinical characteristics of patients admitted to forensically informed pre-discharge unit in England.
Design
Using a prospective service evaluation framework and a clinical case register (n=30) patients were assessed for any change over admission.
Findings
The results showed a statistically significant reduction in the security items and total scores on the Health of the Nation Outcome Scale (HoNOS), and the Clinical and Risk management items and total scores on the Historical Clinical Risk factor-20 (HCR-20), alongside a significance improvement in the Model of Human Occupation Screening Tool (MOHOST) total scores. Furthermore, when contrasted with each other the sample of community discharges showed similar significant improvements to the above whereas the recalled patients showed mostly declining scores evidencing the HCR-20, HoNOS and MOHOSTs ability as predictors of discharge.
Originality / value
These findings are relevant to both users and providers of forensic mental health services as this unit is unique in the sense of it not existing in other services.
Keywords: Pre-discharge; Outcome measures; Predictors of discharge; Forensic mental health; HoNOS; HCR-20; MOHOST; Forensic psychiatry
Introduction
An overview
Forensic mental health services in the United Kingdom cater for the needs of people with severe mental disorder who pose, or have the potential to pose, risks to others, as a result of their mental disorder [1,2]. In 2015 NHS England commissioned 7,719 inpatient beds in secure mental health services in England [3] including 795 in high, 3192 in medium and 3732 in low secure services. In England alone, secure mental health services cost the National Health Service (NHS) approximately £1.2 billion in 2009/10, corresponding to almost 19% of all public expenditure on mental health care [1], as such secure services are high cost but low volume [4]. The characteristics of the patient group that are cared for within forensic mental health services are demarcated by their challenging and risk related behaviours [2]. Patients’ risk behaviours (particularly the risk of harm to others) are intertwined with mental disorder and offending behaviour patterns. Additionally, personality difficulties, such as impulsivity and anger dyscontrol, substance misuse and their tendency to breach relational, procedural and physical security boundaries [5] have been concerns too. Short term reconviction and readmission rates for those discharged from forensic services is relatively low, between 10% and 15% over two years, but longer-term outcomes are much poorer, with reconviction and readmission rates of approximately 50% and over 33% respectively over twenty years [1]. Thus, effective management of this patient population requires a philosophy of care and recovery based approach that addresses their mental disorder, and offending behaviour, as well as challenging behaviours that historically have failed to respond to boundaries in all mental health services. Pathways to unlocking secure mental health care have been the subject of extensive debate among clinicians, academics, policy makers and specialised commissioning groups. Yet, and despite the increasing number of beds for low and medium secure services over the past two decades and benefits to a possible expansion of forensic aftercare services, developing non secure forensic care pathways including stepdown facilities has attracted little attention in the field of forensic mental health care in the UK. The relative lack of investment in developing these pathways may lead to; out of area transfers, delayed discharges or placement in higher levels of security than required [1]. It is imperative that patients are treated at the appropriate level of security not only from a financial perspective (with the annual cost of treatment ranging from £150 K to £300 K per patient in secure settings) but also with reference to the least restrictive principle enshrined within the Mental Health Act 1983 Code of Practice [6]. It is approximated that the use of this pre-discharge service can save the health economy circa £50,000 per patient, per annum compared to a low secure bed that (by definition of being low secure) delivers a more restrictive community discharge pathway. One of the other cost saving elements of this service is also to endeavour to reduce subsequent recall/readmissions to hospital by providing an additional layer of support, guidance and treatment to a complex patient group to allow them to successfully remain in the community.
Forensic care pathway
A care pathway has been defined by Kelly, Mc Cabe, Devine and Simpson as “a multi-disciplinary outline of anticipated care, placed in an appropriate timeframe to help a patient with a specific condition or set of symptoms move progressively through a clinical experience to positive outcomes.” Various other terms have been used to describe the same concept including care mapping, recovery pathway, and integrated care pathway to name a few members [7]. With reference to forensic mental health care, a care pathway has been construed in terms of the level of patient risk-as such there exists high, medium and low levels of security. However, there does not seem to be an agreement among clinicians, service providers and commissioners on what function non-secure foreniscally informed pre-discharge facilities can serve as part of the forensic care pathway. Patient involvement in planning forensic care pathways has attracted little attention too [8]. Arguably, facilities such as these have the potential to provide an effective pathway, underpinned by the principles of recovery and rehabilitation by developing patient awareness and emotional coping, allowing increased responsibility, self-management and independence, and most importantly opportunities for the testing out of behaviours prior to complete discharge into the community. In doing this it supports the safe transition of patients from secure settings into a community placement at an appropriate stage of their rehabilitation minimising the length of stay in secure services and thus reducing readmission. Furthermore, since the patients at this unit are more engaged in their own care pathways through a recovery based approach it has the potential to improve outcomes as demonstrated in the work by Ayub et al. [8]. A framework for this recovery approach has been developed and it involves the use of the ‘my shared pathway’ approach [9].
Present study
There is a dearth of literature on non secure forensically informed predischarge facilities, in terms their utility, existence, patients’ clinical charateristics and outcome measurement. A notable exception is a study which provided a descriptive overview of a non-forensic pre-discharge unit attached to a long term psychiatric hospital [10]. However, the study provided no information about the sample characteristics, outcome measurements used alongside any results and whether or not the unit was forensically informed. To our knowledge, our study is the first of its kind and fills a gap in the literature in the field of community discharges from forensic settings. Using a service evaluation framework, it aimed to describe the demographic and clinical characteristics of patients admitted to a forensically informed pre-discharge unit between its opening in April 2012 and April 2016 when a service evaluation was requested from NHS England, and to assess whether there were significant changes in clinical outcome measures from baseline to endpoints. The patient group that that has been admitted to this unit have been referred from other wards, being either rehabilitation n=20 (57%) or long-term rehabilitation n=15 (43%) as it had been deemed by their clinical teams that these patients would struggle to successfully transition directly into the community. In line with principles of least restrictive practice there was no justification to continue confinement in a low secure hospital just to complete/continue work in areas of mental health awareness, substance misuse or relapse signatures. As such, the use of this type of unit should be seen as being the most appropriate and proportionate.
Method
Setting
The study was conducted at a male only forensically informed pre-discharge NHS unit in England. The unit opened in 2012 and was originally established in response to the number of delayed discharges from conditions of low and medium security in the local area, decline in suitable community facilities for those who stepdown from conditions of low and medium security and in an attempt to reduce readmission after discharge. Treatment philosophy in the unit is based upon the ethos of the recovery model where personal recovery is as important as clinical recovery [11]. The unit is staffed by a multidisciplinary team with forensic expertise and led by a consultant forensic psychiatrist. It provides a non-secure structured environment though with an appropriate level of relational, physical and procedural security measures that is conducive to honest and transparent risk assessment supporting the testing out of behaviours prior to transfer into the community, with the aim of reducing the number of readmissions from community settings. All patients have individualised plans of care, relevant to their risks and rehabilitation goals, which they develop in conjunction with the multidisciplinary team. These plans of care include identified treatment targets with projected timescales, including pharmacological interventions and associated physical health monitoring, exploring educational and vocational opportunities, psychological interventions including social problem solving, anger management, substance misuse and CBT, nursing and occupational therapy interventions. It is important to note that there are clearly defined differences between this unit and a mental health ward in that it is more focussed on recovery and rehabilitation more than solely pharmaceutic treatment, the levels of patient risk and index offence type are more severe, the patients are always under a formal mental health section, there is a high level of input from and access to community team representatives early on in their admission, there are higher levels of interventions offered and the patient group are more treatment resistant. Additionally, there are clear differences between what a low secure unit offers in that as a separate rehabilitation unit there is no access to a seclusion suite or low stimulation area so it is expected that the patients have their own effective coping strategies in place, they should have a significant level of unescorted leave before being given a bed in order to assess their ability to integrate into the community suitably along with the ability to self-medicate, be at least moderately skilled in the activities of daily living (ADL) and to have insight, awareness and knowledge of their mental health problems and associated treatment needs.
Study design and sample
A prospective service evaluation framework utilising data from a clinical case register was employed. The sample consisted of 35 patients admitted to the unit between April 2012 and April 2016. Of those 34 patients were admitted from a local low secure unit and remaining one from a regional medium secure unit bypassing low secure treatment.
Data collection
The clinical database was designed to collect data prospectively on clearly defined outcome measures administered routinely as part of each patient’s care pathway. As a standard, this is completed in the first three months following admission and at six monthly intervals afterwards.
Demographic and clinical characteristics
Data on patient characteristics included (i) demographics such as age, gender, ethnicity, nationality and marital status; (ii) admission data such as referral source, date of admission, discharge data and discharge destination; (iii) diagnoses including both primary and co-morbidity diagnoses were assigned by the patients’ responsible clinician (a consultant forensic psychiatrist) using The International Classification of Diseases categories [12]; and (iv) offending data including the index offence type (including violent, sexual, and nonviolent offences), total number of violent offences across lifetime, total number of non-violent offences across lifetime and age at first offence.
Outcome measures
The Health of the Nation Outcome Scale - Secure [13]: HoNOSSecure contains the original twelve items that assess behaviour, impairment, symptoms and social problems (items 1-12) as well as an additional seven item security scale (items 13-19). Each item is rated on a five point Likert scale to measure levels of problem severity. The HoNOS-Secure is designed to track clinical outcomes as well as ongoing security needs. The Historical Clinical and Risk Management-20-Version 2 [14]. The HCR-20 is a risk assessment tool for predicting the risk of future violent behaviour in criminal and psychiatric populations. It consists of 20 items relating to historical risk information (ten items), clinical risk information (five items) and risk management information (five items) designed to capture relevant past, present and future risk considerations. Each item is scored from 0-2, with 0 being omit, 1 being no and 2 being yes. These scores produce 3 subtotals (Historical, Clinical and Risk Management) and an overall total score out of 40. Although predominately used in clinical practice for its utility in scenario planning, the HCR- 20’s numerical scoring is still considered relevant for purposes of statistical analysis which carry considerably more statistical weight and significance. The Model of Human Occupation Screening Tool- MOHOST [15]. These are completed routinely in order to assess improvements in occupation which form key elements of ability to move on to placements with less support. The evaluation criteria for scoring was used as Facilitates=3, Allows=2, Inhibits=1, Restricts=0 and the scoring criteria is broken down into 6 defined areas with 4 subcategories each. The 6 areas are motivation for occupation; pattern of occupation; communication and interaction skills; process skills; motor skills and environment. The maximum score would be out of 72 with the higher the score showing increased level of occupational ability. Therapeutic activity: This was measured as the number of hours in which patients participated in therapeutic activities (of any sort) collected in the patients’ weekly planners. Therapeutic activity incorporates a number of different activities, including skill development groups, psychological interventions, attendance at clinical meetings, work experience opportunities, activities of daily living and structured leisure time within the community.
Statistical analysis
Descriptive statistics were used to describe the sample. Since much of the data did not meet normal assumptions non-parametric Wilcoxon matched pairs signed ranks tests were used to assess changes in median HoNOS, HCR-20 and MOHOST ratings at different time points across the length of admission. The data was then split into those returned to low secure care and those with community discharge, the data was more evenly spread and a paired T-Test was used to assess for differences of those recalled and those discharged to the community.
Results
Sample characteristics
The results indicate that the average age was 39 years on admission (range=21-66). Overall, 70% of the sample was White British, with the remaining 30% being from Black and Minority ethnic groups. In all, 97% of the sample was single and 3% of other marital status. The primary source of initial admissions prior to transfer to the pre-discharge unit were from other forensic services (47%), followed by prison and other Criminal Justice settings (30%), generic adult mental health services (16%) and other sources (7%). All patients were detained under the Mental Health Act 1983. A total of 44% of the sample were classed as non-restricted patients (Section 3, 37), with the remaining 56% classed as restricted patients (Section 37/41, 47/49). Fewer than 24% of the sample had been discharged on a Community Treatment Order (CTO) before re-admission to secure services.
Clinical characteristics
Overall, 70% of the sample had a violent index offence with 10% having no index offence. The average number of violent offences committed by the sample across their lifetime was 3 (range 0-12) in comparison to the average number of 8 non-violent offences (range 0-42). The mean age at first offence was 24 years of age (range 13-65 years). The average length of time from admission to discharge was 269 days (range=30 to 622). At the time of this report, 6 of the 35 were still inpatients and 29 patients had been discharged, of whom 7 (24%) have been transferred back to the local low secure unit due to attempting to subvert security; unable to show commitment to community living; using leave inappropriately; absconding; substance misuse and also a psychotic episode followed by assault. The most common community discharge destination was supported accommodation (48%). Since the unit opened up until April 2016 only 1 from 22 community discharges (5%) has been re-admitted to forensic services (Table 1).
| Primary ICD-10 Diagnosis (n, %) 35 | |
|---|---|
| Schizophrenia Delusional disorder |
21 (60%) 3 (9%) |
| Schizoaffective disorder Affective disorder |
5 (14%) 4 (11%) |
| Other | 2 (6%) |
| Originally admitted to WRC from (n, %) 35 | |
| Prison | 10 (29%) |
| Other forensic services | 18 (51%) |
| Local services | 6 (17%) |
| Other | 1 (3%) |
| Offending History (n, %) 35 | |
| Index Offence Type | |
| Violent | 23 (66%) |
| Non-violent | 5 (14%) |
| Sexual | 4 (11%) |
| Not applicable | 3 (9%) |
| Number of violent offences across lifetime, including index offence, mean (range) | 2.8 (0-12) |
| Number of non-violent offences across lifetime, including index offence, mean (range) | 8.2 (0-24) |
| Age at first offence in years, mean (range) | 24.5 (13-65) |
| Length of stay in days, mean (range) | 269 (30-622) |
| Patient status (n, %) 35 | |
| Inpatient | 6 (17%) |
| Discharged | 29 (83%) |
| Discharge destination (n, %) 29 | |
| Supported accommodation | 14 (48%) |
| Independent living | 8 (28%) |
| Wells Road Centre | 7 (24%) |
Table 1: Summarises the clinical characteristics of the sample. The most common primary diagnosis in the sample was schizophrenia (60%), followed by affective disorders (14%). Substance misuse and dependence (including alcohol) was highly prevalent as a co-morbid diagnosis (53%), followed by personality disorder (15%).
Outcome measures
HoNOS-Secure, HCR 20 and MOHOST. Table 2 shows the changes in the HoNOS, HCR-20 and MOHOST ratings from baseline to end point (discharge or end of January 2016 for current inpatients). These results indicate a significant reduction from baseline to end point scores for the HoNOS secure items (W=255.5; z=-2.507, p=.012*) and HoNOS Total Score (W=309; z=-3.393, p=.001**). Similarly, significant differences were noted for the Clinical (W=259; z=- 3.120, p=.002*), Risk Management (W=284.00; z=-3.276, p=.001**) and Total HCR-20 (W=311.00; z=-3.447, p=.001**) items from the baseline, to end point scores along with statistical improvements for total MOHOST scores (W=276; z=-2.070, p=.038*). Alongside these paired-samples t-tests were conducted, shown in Table 3 to compare those who were recalled to low secure conditions and those discharged in to the community. There was a significant differences in scores for the HoNOS secure items for community discharges, admission scores (M=12.76, SD=4.55) to discharge scores (M=9.76, SD=3.99); t (16)=2.525, p=.023*. There were also significant difference in scores for the HoNOS total items for community discharges, admission scores (M=16.88, SD=4765) to discharge scores (M=13.53, SD=3.91); t (16)=2.845, p=.012*. With HCR-20 categories there were also significant changes for the community discharges – clinical (M=5.31, SD=3.09) (M=4.00, SD=2.82); t (16)=2.174, p=.046* - risk management (M=6.37, SD=2.52) (M=3.93, SD=1.98); t(16)=5.049, p=.001** and total score (M=25.43, SD=5.42) (M=21.56, SD=4.95); t (16)=4.291, p=.001**. Additionally, MOHOST had significant improvements for the community discharges (M=43.47, SD=16.03) (M=52.66, SD=10.68); t (16)=-3.363, p=.005*. The sample that was made up of recalled patients had some small improvements of scores but mostly showed a decline in scores. These results suggest that some patients can struggle with the extra freedom of the pre-discharge unit and as such have an increase in negative symptomology leading to recall.
| HoNOS- Secure | Baseline rating Mean (s.d.) n=33 |
End point rating Mean (s.d.) n=33 |
p |
|---|---|---|---|
| Total 12 Items | 5.6 (4.7) | 3.9 (3.5) | .321 |
| Total Security Scale Items | 13.9 (4.1) | 10.5 (5.3) | .012* |
| Total HoNOS-Secure Score | 17 (3.9) | 13.5 (3.5) | .001* |
| HCR-20 | Baseline rating Mean (s.d.) n=33 |
End point rating Mean (s.d.) n=33 |
p |
| Historical | 14.2 (3.1) | 14.6 (2.6) | .248 |
| Clinical | 5.2 (2.8) | 3.2 (2.4) | .002* |
| Risk Management | 5.8 (2.6) | 3.9 (2.2) | .001* |
| HCR-20 Total | 25.3 (5.4) | 21.7 (4.6) | .001* |
| MOHOST | Baseline rating Mean (s.d.) n=33 |
End point rating Mean (s.d.) n=33 |
p |
| 48.3 (15.8) | 53.7 (11.1) | .038* |
Table 2: Changes in mean HoNOS, HCR-20 and MOHOST ratings at baseline and end point, and significance of change.
| Patients returned back to low secure setting | Patients discharged to community settings | |||||
|---|---|---|---|---|---|---|
| HoNOS- Secure | Baseline rating Mean (s.d.) n=7 |
End point rating Mean (s.d.) n=7 |
p | Baseline rating Mean (s.d.) n=22 |
End point rating Mean (s.d.) n=22 |
p |
| Total 12 Items | 2.00 (1.82) | 2.00 (1.82) | Not computed as standard error of difference=0 | 5.88 (4.88) | 4.53 (3.33) | .336 |
| Total Security Scale Items | 15.25 (1.5) | 13.5 (3.31) | .336 | 12.76 (4.54) | 9.74 (3.99) | .023* |
| Total HoNOS-Secure Score | 16.75 (1.5) | 15.00 (4.24) | .258 | 16.88 (4.76) | 13.53 (3.91) | .012* |
| HCR-20 | Baseline rating Mean (s.d.) n=7 |
End point rating Mean (s.d.) n=7 |
p | Baseline rating Mean (s.d.) n=22 |
End point rating Mean (s.d.) n=22 |
p |
| Historical | 15.25 (2.62) | 15.00 (2.00) | .333 | 13.56 (3.44) | 13.62 (3.44) | .333 |
| Clinical | 4.5 (2.64) | 6.00 (1.73) | .429 | 5.31 (3.09) | 4.00 (2.82) | .046* |
| Risk Management | 5.25 (2.75) | 7.66 (0.57) | .421 | 6.37 (2.52) | 3.93 (1.98) | .001* |
| HCR-20 Total | 25.00 (5.59) | 28.66 (1.52) | .418 | 25.43 (5.42) | 21.56 (4.95) | .001* |
| MOHOST | Baseline rating Mean (s.d.) n=7 |
End point rating Mean (s.d.) n=7 |
p | Baseline rating Mean (s.d.) n=22 |
End point rating Mean (s.d.) n=22 |
p |
| 51.33 (13.57) | 42.00 (7.00) | .43 | 43.47 (16.03) | 52.66 (10.68) | .05* | |
Table 3: Changes in mean HoNOS, HCR-20 and MOHOST ratings at baseline and end point for patients returned to conditions of low secure and those discharged into the community (totalling 29 patients), and significance of change.
Therapeutic activities
The average number of hours of offered activity was 1463 (range=1095-1859) with a total number of accepted activities was 1433 (range=774-2071). When the data on therapeutic activity was averaged out we found that on average patients were offered 27 h of structured activity per week. Patients then went on to accept and engage in an average of 26 h of structured activity per week. Though this altered when the two groups were compared with the community discharges doing over 6 h more therapeutic activity per week than those recalled.
Discussion
The main findings of the study indicate that patients were mostly white ethnicity, single and classed as restricted patients. The most common primary diagnosis was that of Schizophrenia. Substance misuse was highly prevalent as a secondary diagnosis and the vast majority of the sample had a violent index offence. The average length of stay from admission to discharge was 269 days. There was a significant reduction from baseline to end point scores for the HoNOS secure items and HoNOS total scores. Similarly, significant improvements were noted for the Clinical, Risk Management and Total HCR-20 items from the baseline, to end point scores along with statistical improvements for total MOHOST scores. This suggests that the ongoing security needs and risk levels of the population reduced significantly over time with a significant increase in their level of occupational functioning, possibly as a result of admission to this pre-discharge unit. Additionally, to this there was some improvement in scores of HoNOS secure and total scores for those returned back to low secure but a decline in scores for the Clinical, Risk management and total scores for HCR-20 and also MOHOST. However, the community discharged patients continued to mirror the significant improvements from the combined scores. Since there is no literature on changes in these scores after community discharge from forensic units it is hard to determine whether these results are purely by chance or as a result of the extra support, although it seems reasonable to assume at least some progress is due to the extra support and interventions received which can potentially lead to reducing readmissions.
Patient Chracteristics Outcome Measures
Due to relative lack of of literature on pre-discharge units, it has not been possible to interpert the findings of this evaluation in the light of existing literature in the field. However, data from secure forenisc settings (particularly low and medium security) may assist with the interpretation of our findings as follows. The demographic characteristics reported in the study were evidenced to be similar to those of Pereria, Khalifa [16,17] with the majority of the sample being male, white, single and diagnosed with a mental illness such as schizophrenia. The average length of stay of 269 days for this study was considerably lower than length of stay reported in low secure services of 354 days and 399 days but it should be noted that the length of stay is additional to a stay in secure services not instead of. It is notable that there were more restricted patients in the present study (56%) when compared to the 26% reported by Beer, et al. [16]. Additionally, Beer reported that 56.5% of their sample were nonoffenders without an index offence compared to the 10% without an index offence in the present study showing the patients who transition through the pre-discharge unit have more complex needs/diagnoses and as such may require additional support to make a successful transition into the community [17]. Since this type of unit is relatively unique it is important to note the utility of what it can achieve differently from other secure and non-secure services (the differences of these units having been discussed previously). It should also be noted that those patients transferred back to the low secure setting not been seen as ‘failing’ since the unit is to assist in community reintergration for those who could’ve either been in hospital for a long time and/or who show treatment resistent traits. This could suggest that they may present as being well within hospital settings but complications could be triggered the closer they become to community living which would require tailored work such as what is offered in this pre-discharge unit. It has also proven to be valuable for those who were recalled to low secure were able to be managed more effectively at the pre-discharge unit than in a community placement whilst waiting for a secure bed to become available. The security items for the HoNOS-secure reduced significantly from baseline to endpoints. This indicates that the ongoing security needs of the patients reduced overtime. In contrast with this, no significant changes in the security needs were observed in a study by Sugarman [13]. This research noted no changes over time in patient symptomatology, but a reduction in their ongoing security needs as assessed by the HoNOS-Secure. This may be due to the fact that scores on the 12 items were already low at baseline, likely reflecting the progress made at previous placements. Sugarman argued the reason for their findings may have been due to the small size of the service and that there was less opportunities to progress through different levels of security within the service when compared to their other inpatient services, this is comparable to this service which also had a small sample but did achieve significant change [13]. When looking at the comparison between the recalled patients and the discharged for HoNOS secure scale and total scores there were reductions in all scores but only those discharged showed a significant change. This tends to ratify the previously mentioned reasons for recall which included the subversion of security, absconding and inability to commit to the community as these patients may still require a higher level of security to continue their rehabilitation and ensure the safety of everyone. Furthermore, significant changes were observed for the Clinical and Risk Management items, as well as the total HCR-20 score [14]. The results of this suggest that the ongoing risk status of the cohort was observed to change significantly over time, although these may reflect the progress made by the patient at previous placments rather than just the pre-discharge unit. Olsson, Strand, Kristiansen, Sjöling, Asplund also evidenced a reduction in the clinical and risk management scales from the first, second and third risk assessment over time. Similarly, research by Morrissey conducted in a high secure sample found that the clinical and risk management items decreased by approximately 1 point or less, and the HCR-20 total score reduced by 1.5 points across a five year period. Such research indicates that the HCR-20 is sensitive to changes over time, suggesting that positive change may come over the passage of time (though this is not the case with all forensic patients and as high secure patients their initial ratings were very high to begin with and as such could almost only show improvements). Alongside this when comparing samples, for those who were recalled their clinical, risk management and total HCR-20 scores showed a decline suggesting the level of support needed and risk levels could not be adequately managed outside a forensic hospital setting at that point contrasted with significant improvements from those discharged. It would be disingenuous to suggest that the extra time spent in pre-discharge for those with complex histories has little to no impact as referenced by a relatively low readmission rate (6%). Existing literature suggest that readmission rates in some psychiatric settings can range from 10-29 % (20) and up to 51% dependent upon length of admission [18], though these were mostly for general psychiatric settings rather than forensic. An international study by Fazel, looked at readmissions in forensic units and the rate was 1,171 from 3,522 (35%) [4]. Alongside this there were significant improvements in the total MOHOST scores for the patient group. These changes reflect improvement in patients’ occupational functioning, likely due to increased access to occupational therapy activities, easy access to community facilities and improvement in their mental state over time. They do not necessarily reflect improvement as a result of occupational therapy interventions. There is little information on changes over time MOHOST over time within a forensic environment [19]. It has been demonstrated that the recalled groups scores got worse in occupation and that on average they only took up just over 21 h per week compared with a statistically significant improvement for the discharged patients who took up over 27 h per week [20,21]. This shows a lack of community integration, functioning and correct use of leave which is part of successful community placements and suggested an increase of isolative type behaviours compared to the successes of patients who maintain motivating and reassuring social networks around them [22-25]. In all the use of assessing the scores of the two groups (recalled patients and community discharged patients) side by side suggests that by using HoNOS, HCR-20 and MOHOST scores along with therapeutic activity uptake could be useful as predictors of discharge (particularly into the community). This of course cannot replace knowledge of the patient. Work by Archibald, Campbell and Ambrose, shows that the HCR-20 is a better predictor of discharge than other tools. Alongside this a more direct route into the community can cause readmission problems rather than the staggered approach offered at the pre-discharge unit. This was demonstrated by Riorden, Haque and Humphreys where they showed that in their sample those conditionally discharged and with minimal supervision were 6 times more likely to readmitted if they misused drugs, 5 times more likely to be readmitted if they didn’t have a support network and were 4½ more times likely to be absolutely discharged if they had a successful care pathway planned [8,26]. These conditions and scenarios can be extrapolated against those services provided in pre-discharge again to account for the low readmission rates of the pre-discharge patients and the utility of a slow and integrated community and forensic approach.
Strengths and Limitations of Study
This study was able to provide an overview of patient characteristics and clinical outcomes over time during admission to a forensically informed pre-discharge unit. The findings of this study are relevant to clinical practice, as measuring and demonstrating clinical outcomes is an essential task in service improvement. Since this is a small unit there have only been a limited number of patients transition through the unit since opening this study should be veiwed as a pilot to be reviewed again when the numbers have increased to ensure the positive results being produced are replicatable.
Clinical Implications
It demonstrated the utility of the pre-discharge unit, in terms of improving patient outcomes in the domains of security, risks and occupation. These areas improve likeliness of success in the community. In the current economic climate, there is a greater need to increase psychiatric rehabilitation and minimise the negative impact of this high risk secure patient population with diminishing resources which is why treatment ethos has altered from cure to stabilisation. Often this has meant early discharge, and greater use of community services though at the expense of increased readmission rates which is where units like this can fill a gap in present services preventing re admission [27,28].
References
- Centre for mental health (2011) Pathways to unlocking secure mental health care.
- Joint Commissioning Panel for Mental Health (2013) Guidance for commissioners of forensic mental health services.
- NHS England (2015) NHS Standard contract for high secure mental health services (Adults).
- Fazel S, Fiminska Z, Cocks C, Coid J (2016) Patient outcomes following discharge from secure psychiatric hospitals: systemic review and meta-analysis. Br J Psychiatry 208: 17-25.
- Lindqvist P, Skipworth J (2000) Evidence-based rehabilitation in forensic psychiatry. The Br J Psychiatry 176: 320-323.
- Department of Health (2015). Mental Health Act 1983: Code of Practice. The Stationary Office-London.
- Kelly H, Mc Cabe T, Devine P, Simpson B (2011) Care pathway and model for community forensic teams in N. Ireland.
- Ayub R, Callaghan I, Haque Q, McCann G (2013) Increasing patient involvement in care pathways.
- NHS Networks (2012) My Shared Pathway in secure settings.
- Liu MC, Hughes MW, Ashton LM (1976) A predischarge unit in a long-stay hospital for subnormality. The Br Med J 2: 921-922.
- Slade M, Amering M, Farkas M, Hamilton B, Hagan M, et al. (2014) Uses and abuses of recovery: implementing recoveryâ€Âoriented practices in mental health systems. World Psychiatry 13: 12-20.
- World Health Organization (1993) The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research. Geneva, Switzerland: World Health Organization.
- Sugarman P, Walker L (2007) HoNOS-secure version 2b.
- Douglas KS, Hart SD, Webster CD, Belfrage H (2013) HCR-20 V3: Assessing risk of violence user guide. Burnaby, Canada: Mental Health, Law, and Policy Institute, Simon Fraser University.
- Parkinson S, Forsyth K, Kielhofer G (2005) The Model of Human Occupation Screening Tool version 2.0, Model of Human Occupation Clearinghouse, Department of Occupational Therapy, College of Applied Health Sciences, University of Illinois, Chicago, IL.
- Beer MD, Tighe J, Ratnajothy K, Masterson D (2007) Predicting outcome in low secure environments: a case series from one low secure unit. Journal of Psychiatric Intensive Care 3: 85-92.
- Pereira S, Dawson P, Sarsam M (2006) The National Survey of PICU and Low Secure Services: 1. Patient characteristics. J Psychiatr Intensive Care 2: 7-12.
- Figueroa R, Harman J, Engberg J (2004) Use of claims data to examine the impact of length of inpatient psychiatric stay on readmission rate. Psychiatric Services 55: 560-565.
- Moore M (2005) Chapter 11: Forensic psychiatry and occupational therapy. Occupational therapy in psychiatry and mental health. 4th edition London: Whurr Publishers Ltd.
- Fleury M, Grenier G, Bamvita J, Trembla, J., Schmitz, N, et al. (2013) Predictors of quality of life in a longitudinal study of users with severe mental disorders. Health Qual Life Outcomes 11: 92-104.
- Brooke CA (2015) Selected psychometric properties of the activity participation outcome measure to describe trends in a forensic population of mental health care users.
- Davies S, Clarke M, Hollin C, Duggan C (2007) Long-term outcomes after discharge from medium secure care: a cause for concern. Br J Psychiatry 191: 70-74.
- Kennedy HG (2002) Therapeutic use of security: mapping forensic mental health services by stratifying risk. Advances Psychiatric treatment 8: 433-443.
- Ayub R, Callaghan I, Haque Q, McCann G (2013) Increasing patient involvement in care pathways.
- Vigod SM, Kurdyak PA, Dennis C, Leszcz T, Taylor VH, et al. (2013) Transitional interventions to reduce early psychiatric readmissions in adults: systematic review. Br J Psychiatry 202: 187-194.
- Leamy M, Bird V, Le Boutillier C, Williams J, Slade M (2011) Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry 199: 445-452.
- Nelson EA, Maruish M.E., Axler JL (2000) Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatric Services 51: 885-889
- Young et al. (1999) Medication adherence failure in Schizophrenia: a forensic review of rates, reasons, treatments and prospects. J Am Acad Psychiatry Law 27: 426-444.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi