Research Article, J Clin Exp Oncol Vol: 7 Issue: 6
Patterns of Outcome in Human Papilloma Virus Positive Oropharyngeal Squamous Cell Carcinoma Treated Primarily with Radical Radiotherapy
Ha Lu1*, Anni Chen1, Ivan Iankov1, Myo Min2, Raghu Gowda1, Rahul Mukherjee1, Daniel Roos1,3 and Hien Le1
1Radiation Oncology Department, Royal Adelaide Hospital, Adelaide, Australia
2Radiation Oncology Department, Sunshine Coast University Hospital, Queensland, Australia
3School of Medicine, University of Adelaide, Adelaide, Australia
*Corresponding Author : Ha Lu
Radiation Oncology, Royal Adelaide Hospital, Port Road, Adelaide, Australia
Tel: +61 8 7074 0000
E-mail: ha.lu.adelaide@gmail.com
Received: October 22, 2018 Accepted: November 06, 2018 Published: November 13, 2018
Citation: Lu H, Chen A, Iankov I, Min M, Gowda R, et al. (2018) Patterns of Outcome in Human Papilloma Virus Positive Oropharyngeal Squamous Cell Carcinoma Treated Primarily with Radical Radiotherapy. J Clin Exp Oncol 7:6. doi: 10.4172/2324-9110.1000232
Abstract
Introduction: The aims of this study were to determine patterns of outcome and prognostic factors in human papilloma virus positive oropharyngeal squamous cell carcinoma (OPSCC+) treated primarily with radical radiotherapy.
Materials and methods: We identified 54 patients at a tertiary hospital in South Australia who received treatment with curative intent for OPSCC+ with radical radiotherapy ± chemotherapy or cetuximab from 1st January, 2010 to 31st March, 2017. We explored the effect of patient, tumour and radiotherapy factors on treatment outcomes. The primary endpoint was overall survival and the secondary endpoint was disease-free survival.
Results: The median age was 59, with most patients being male (82%). The majority had advanced disease (89% stage IV). The median follow-up was 22.5 months. The one-year and two-year overall survival and disease-free survival rates were 89% and 79% and 77% and 68% respectively. Active smoking during radiotherapy was associated with trends to shortened overall survival (p=0.084) and reduced time to recurrence (p�?0.1). However, there was no statistically significant relationship between any other patient, tumour or treatment factors and disease-free or overall survival.
Discussion: Despite advanced stage at presentation, radiotherapy ± concurrent systemic therapy results in favorable outcomes for OPSCC+. Active smoking during radiotherapy may compromise overall survival. We strongly recommend smoking cessation prior to commencing radiotherapy for OPSCC+. In addition, we note that smokers involved in de-intensification trials may be at increased risk of poor outcomes.
Keywords: Squamous cell carcinoma; Oropharyngeal neoplasms; Human papilloma virus; Prognostic factors; Radiotherapy; Smoking
Introduction
The overall incidence of oropharyngeal squamous cell carcinoma (OPSCC) is increasing despite a progressive decline in tobacco use, a well-known risk factor [1-4]. In fact, this trend is occurring in the context of decreasing incidence of all other head and neck cancers [5] due to the increasing incidence of human papilloma virus (HPV) positive OPSCC (OPSCC+) [1,2,6,7]. OPSCC+ is a growing epidemic, with over 70% of OPSCC cases thought to be HPV-related [8,9]. OPSCC+ is associated with changing sexual behaviours, resulting in shifting demographics of OPSCC patients who are more likely to be younger, Caucasian and from developed countries [1,10-12].
OPSCC+ is increasingly recognized as a biological and clinical entity distinct from OPSCC- [3]. There are fundamental differences in terms of genetics, risk factors, natural history and treatment response [13]. HPV is the most common sexually transmitted infection, but most subtypes do not cause clinical disease. A small proportion of subtypes, particularly p16 and p18, may be persistent and oncogenic, causing OPSCC+. OPSCC+ is associated with wild-type p53, downregulation of pRb, and up-regulation of p16, whereas OPSCC- is associated with increased p53 mutations, up-regulation of pRb and decreased p16 levels [4]. Immunohistochemistry for p16 is currently used as a reliable surrogate marker for HPV, although other markers are also being investigated [9,14].
The number of oral sexual partners is a risk factor for OPSCC+, but not OPSCC- [3,15]. In contrast, heavy tobacco and alcohol use are risk factors for OPSCC-, but not OPSCC+ [3]. OPSCC+ typically presents as a smaller primary tumor but with more advanced lymph node disease, resulting in higher stage [16,17]. A growing body of literature demonstrates that survival in OPSCC+ is significantly better compared to OPSCC- [18-27]. For example, a cancer registry review in the United States determined the median survival in OPSCC+ patients to be 131 months, compared with 20 months in OPSCC- patients [2].
Recommendations from international best practice guidelines include either surgery or radiotherapy for early stage disease [28,29]. Locally advanced disease is generally approached with multimodality treatment, with surgery plus postoperative adjuvant therapy (radiotherapy with or without chemotherapy) or radical radiotherapy in combination with systemic therapy [28,29]. The purpose of this retrospective review was to examine outcomes and prognostic factors for OPSCC+ patients treated non-surgically with curative intent at our institution.
Materials and Methods
We studied patients at a tertiary hospital in South Australia who received treatment for OPSCC+ with radical radiotherapy. Patients managed with surgical resection were excluded. We explored the effect of patient, tumour and radiotherapy factors on treatment outcomes. The primary endpoint was overall survival and the secondary endpoint was disease-free survival.
Departmental databases and medical records were reviewed from 1st January 2010 to 31st March 2017. 54 patients were identified as suitable for the study. Patient data collected included age, gender, smoking history and alcohol history. Disease-related data collected were tumour stage (American Joint Committee on Cancer 7th edition) and tumour differentiation. Treatment data collected were radiotherapy dose, radiotherapy fractionation and systemic therapy agent [30].
Estimates of disease-free survival and overall survival were calculated using the Kaplan-Meier method for each covariate of interest. The two groups were compared using the log-rank test. We developed two proportional hazard Cox regression models, one with time to death as the dependent variable and one with time to recurrence as the dependent variable.
Results
Table 1 summarises the patient, tumour and treatment factors. Consistent with the known demographics of OPSCC+, most patients were male (82%), either current smokers (32%) or ex-smokers (44%), and actively consuming alcohol (70%). The median age was 59.
| Characteristic | n (%) |
|---|---|
| Gender Male Female |
44 (81.5%) 10 (18.5%) |
| Age Range Median |
38-82 59 |
| Smoking Current smoker Ex-smoker Non-smoker |
17 (31.5%) 24 (44.4%) 13 (24.1%) |
| Alcohol history Current alcohol consumption Previous alcohol consumption Never consumed alcohol |
38 (70.4%) 7 (13.0%) 9 (16.7%) |
| Tumour stage Stage I Stage II Stage III Stage IV |
1 (1.9%) 0 (0%) 5 (9.3%) 48 (88.9%) |
| Tumour differentiation Well differentiated Moderately differentiated Poorly differentiated Unknown |
3 (5.6%) 20 (37.0%) 27 (50%) 4 (7.4%) |
| Radiotherapy dose 66Gy in 30 fractions 70Gy in 35 fractions |
38 (70.4%) 16 (29.6%) |
| Chemotherapy Yes Cisplatin Carboplatin Cetuximab Unknown No |
49 (90.7%) 34 (63.0%) 1 (1.9%) 11 (20.4%) 3 (5.6%) 5 (9.3%) |
Table 1: Patient, tumor and treatment characteristics.
In terms of tumour characteristics, the majority had advanced disease (89% stage IV) with moderately (37%) or poorly differentiated (50%) histology.
All patients were treated with radiotherapy, either 66Gy in 30 fractions (70%) or 70Gy in 35 fractions (30%), most with concurrent systemic therapy (91%), predominantly cisplatin or cetuximab.
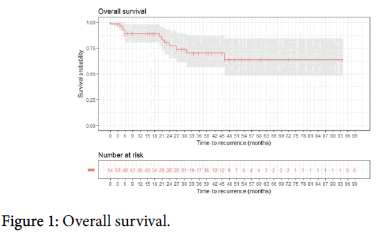
The median follow-up was 22.5 months. The one-year and two-year overall survival rates were 89% and 79%, respectively (Figure 1).
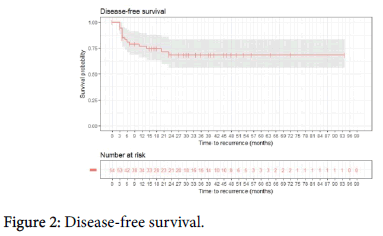
The one-year and the two-year disease-free survival rates were 77% and 68%, respectively (Figure 2).
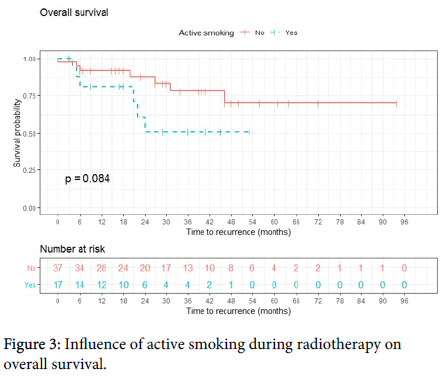
Median survival was not reached. Sites of distant metastases included lung, bone, liver and brain. Active smoking during radiotherapy was associated with a trend to shortened overall survival (p=0.084) (Figure 3).
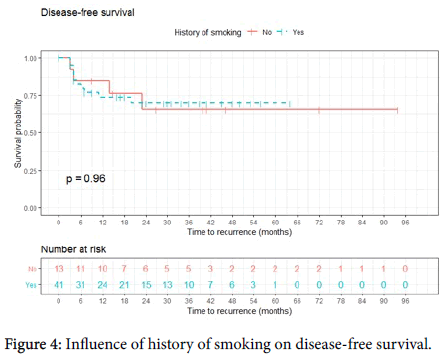
Cox proportional hazards modelling with response variable time to death and regressor smoking status estimated that patients who actively smoked during radiotherapy had a monthly hazard rate 2.57 times higher than patients who did not smoke (p=0.095). However, possibly due to the small sample size, using the Cox proportional hazards model with response variable time to recurrence and regressor smoking status, the influence of active smoking on time to recurrence was not statistically significant (p>0.1). History of smoking (patients who were active or reformed smokers) trended towards shortened overall survival, but again this was not statistically significant (p>0.1). There was no association between history of smoking and time to recurrence (Figure 4). Data analysis did not reveal evidence that smoking status is confounded with any known risk factor for higher mortality or recurrence rate.
No other patient, tumour or treatment factors had a statistically significant influence on disease-free survival or overall survival.
Discussion
This retrospective, single centre review confirmed favourable outcomes for generally advanced stage OPSCC+ patients treated nonsurgically. Although the small sample size limited the strength of our findings regarding prognostic factors, there was a strong trend to worse survival for current smokers, but no other statistically significant patient, tumour or treatment factors.
Radical chemo-radiotherapy is associated with significant acute and chronic morbidity [31]. Adverse effects include the need for gastrostomy tube placement, dysphagia, aspiration, mucositis, xerostomia and dysgeusia [32,33]. This is even more pertinent to OPSCC+, as patients are generally younger and therefore likely to survive longer with late effects. Although it is now well understood that OPSCC+ has a better prognosis and response to treatment compared to OPSCC-, treatment currently remains the same [4,34]. Given the treatment morbidity and the relatively good prognosis of OPSCC+, there is debate regarding the potential for treatment deintensification [35]. Evidence for modified regimens remains limited, but there are numerous current and planned clinical trials investigating treatment de-intensification [36-38]. Currently, modified treatment for OPSCC+ is limited to these clinical trials [5,39]. In the clinical setting, HPV testing is used as a strong and independent prognostic indicator for OPSCC+, but is not yet used to guide treatment [18].
De-intensified treatment could potentially be offered to patients with favorable prognostic factors, who would need to be distinguished from patients at high risk of disease progression. Treatment options include minimally-invasive surgery, reducing radiation dosage, reducing radiation treatment volumes, altered radiation fractionation, alternative chemotherapy agents and omission of chemotherapy [39].
There are several factors that may contribute to poor outcomes in smokers with OPSCC+ receiving radical radiotherapy. The biological behaviour of OPSCC+ may be altered by smoking, promoting tumour progression and leading to decreased response to therapy [15,18]. Smoking can reduce the oxygen carrying capacity of blood and can contribute to a hypoxic tumour micro-environment, which is thought to cause hypoxia-induced radiation resistance [40-42]. Smoking can increase the risk of developing secondary malignancies such as lung and oesophageal cancer. Patients who continue to smoke during radiotherapy may be at increased risk of mucosal toxicities [43,44] which may in turn affect treatment compliance and long term oncological outcome.
Conclusion
Several strategies may be used to support patients with smoking cessation. It should be recognised that smoking is a chronic addictiondriven condition that can be treated with medical intervention. We suggest that clinicians make smoking cessation a key component and should begin with education and counselling, which we recommend commencing at the first consultation. This may be augmented with behavioural and pharmacological therapy. The clinician may also involve the primary carrier and a drug and alcohol unit in treatment. Finally, reformed patients should be reviewed periodically as smoking relapse rates are up to 50% at one year [45]. The routine follow-up consultations that OPSCC+ patients attend provide ideal opportunities to encourage and reinforce smoking cessation. Nurse-managed smoking cessation programs for head and neck cancers have shown positive results and these could be integrated into treatment programs [46].
Study Limitations
This study was conducted at a recognised centre of excellence for the treatment of head and neck cancer with initial referrals directed primarily to the Department of Otorhinolaryngology and Head and Neck Surgery. Therefore, our hospital may treat more cases of OPSCC + surgically than other centres. As such, fewer cases are primarily treated with radical radiotherapy and therefore our cohort may be biased towards those with advanced loco-regional disease and multiple comorbidities precluding them from surgical treatment.
Although this data set was collected over a seven year period, we acknowledge that the sample size was relatively small, with heterogenous radiation and systemic treatment practices. However, this reflects ‘real-world’ variations in patient treatment. The follow-up time was also relatively short and patient outcomes will need to be monitored over a longer period to strengthen the conclusions.
Given our findings, we strongly recommend smoking cessation prior to commencing radiotherapy for OPSCC+. In addition, we note that smokers involved in de-intensification trials may be at increased risk of poor outcomes.
References
- Ang KK, Sturgis EM (2012) Human papillomavirus as a marker of the natural history and response to therapy of head and neck squamous cell carcinoma. Semin Radiat Oncol 22: 128-142.
- Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, et al. (2011) Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol 29: 4294-4301.
- Gillison ML, D'Souza G, Westra W, Sugar E, Xiao W, et al. (2008) Distinct risk factor profiles for human papillomavirus type 16-positive and human papillomavirus type 16-negative head and neck cancers. J Natl Cancer Inst 100: 407-420.
- Haddad RI (2017) Human papillomavirus associated head and neck cancer 2017. Wolters Kluwer, USA.
- Sturgis EM, Ang KK (2011) The epidemic of HPV-associated oropharyngeal cancer is here: is it time to change our treatment paradigms? J Natl Compr Canc Netw 9: 665-673.
- Chenevert J, Chiosea S (2012) Incidence of human papillomavirus in oropharyngeal squamous cell carcinomas: Now and 50 years ago. Hum Pathol 43: 17-22.
- Habbous S, Chu KP, Qiu X, La Delfa A, Harland LT, et al. (2013) The changing incidence of human papillomavirus-associated oropharyngeal cancer using multiple imputation from 2000 to 2010 at a Comprehensive Cancer Centre. Cancer Epidemiol 37: 820-829.
- Moore KA, Mehta V (2015) The Growing Epidemic of HPV-Positive Oropharyngeal Carcinoma: A Clinical Review for Primary Care Providers. J Am Board Fam Med 28: 498-503.
- Yom SS (2015) HPV and oropharyngeal cancer: Etiology and prognostic importance. Semin Cutan Med Surg 34: 178-181.
- Chaturvedi AK, Anderson WF, Lortet-Tieulent J, Curado MP, Ferlay J, et al. (2013) Worldwide trends in incidence rates for oral cavity and oropharyngeal cancers. J Clin Oncol 31: 4550-4559.
- Deschler DG, Richmon JD, Khariwala SS, Ferris RL, Wang MB (2014) The "new" head and neck cancer patient-young, nonsmoker, nondrinker, and HPV positive: evaluation. Otolaryngol Head Neck Surg 151: 375-380.
- Pytynia KB, Dahlstrom KR, Sturgis EM (2014) Epidemiology of HPV-associated oropharyngeal cancer. Oral Oncol 50: 380-386.
- Elrefaey S, Massaro MA, Chiocca S, Chiesa F, Ansarin M (2014) HPV in oropharyngeal cancer: The basics to know in clinical practice. Acta Otorhinolaryngol Ital 34: 299-309.
- Lewis A, Kang R, Levine A, Maghami E (2015) The New Face of Head and Neck Cancer: The HPV Epidemic. Canc Network 29: 616-626.
- Dalianis T (2014) Human papillomavirus (HPV) and oropharyngeal squamous cell carcinoma. Presse Med 43: e429-34.
- Fischer CA, Kampmann M, Zlobec I, Green E, Tornillo L, et al. (2010) p16 expression in oropharyngeal cancer: Its impact on staging and prognosis compared with the conventional clinical staging parameters. Ann Oncol 21: 1961-1916.
- Hafkamp HC, Manni JJ, Haesevoets A, Voogd AC, Schepers M, et al. (2008) Marked differences in survival rate between smokers and nonsmokers with HPV 16-associated tonsillar carcinomas. Int J Cancer 122: 2656-2664.
- Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, et al. (2010) Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med 363: 24-35.
- Broglie MA, Soltermann A, Rohrbach D, Haile SR, Pawlita M, et al. (2013) Impact of p16, p53, smoking, and alcohol on survival in patients with oropharyngeal squamous cell carcinoma treated with primary intensity-modulated chemoradiation. Head Neck 35: 1698-1706.
- Fakhry C, Westra WH, Li S, Cmelak A, Ridge JA, et al. (2008) Improved survival of patients with human papillomavirus-positive head and neck squamous cell carcinoma in a prospective clinical trial. J Natl Cancer Inst 100: 261-269.
- Lassen P, Eriksen JG, Hamilton-Dutoit S, Tramm T, Alsner J, et al. (2009) Effect of HPV-associated p16INK4A expression on response to radiotherapy and survival in squamous cell carcinoma of the head and neck. J Clin Oncol 27:1992-1998.
- Nichols AC, Dhaliwal SS, Palma DA, Basmaji J, Chapeskie C, Dowthwaite S, et al. (2013) Does HPV type affect outcome in oropharyngeal cancer? J Otolaryngol Head Neck Surg 42: 9.
- Petrelli F, Sarti E, Barni S (2014) Predictive value of human papillomavirus in oropharyngeal carcinoma treated with radiotherapy: An updated systematic review and meta-analysis of 30 trials. Head Neck 36: 750-759.
- Psyrri A, Rampias T, Vermorken JB (2014) The current and future impact of human papillomavirus on treatment of squamous cell carcinoma of the head and neck. Ann Oncol 25:2101-2115.
- Wang MB, Liu IY, Gornbein JA, Nguyen CT (2015) HPV-Positive Oropharyngeal Carcinoma: A Systematic Review of Treatment and Prognosis. Otolaryngol Head Neck Surg 153: 758-769.
- Weinberger PM, Merkley MA, Khichi SS, Lee JR, Psyrri A, et al. (2010) Human papillomavirus-active head and neck cancer and ethnic health disparities. Laryngoscope 120: 1531-1537.
- O'Rorke MA, Ellison MV, Murray LJ, Moran M, James J, et al. (2012) Human papillomavirus related head and neck cancer survival: a systematic review and meta-analysis. Oral Oncol 48: 1191-1201.
- An Y, Holsinger FC, Husain ZA (2016) De-intensification of adjuvant therapy in human papillomavirus-associated oropharyngeal cancer. Cancers of the Head & Neck 1: 18.
- Gregoire V, Lefebvre JL, Licitra L, Felip E, Group E-E-EGW (2010) Squamous cell carcinoma of the head and neck: EHNS-ESMO-ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 21 Suppl 5: v184-186.
- Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17: 1471-1474.
- Masterson L, Moualed D, Liu ZW, Howard JE, Dwivedi RC, et al. (2014) De-escalation treatment protocols for human papillomavirus-associated oropharyngeal squamous cell carcinoma: a systematic review and meta-analysis of current clinical trials. Eur J Cancer 50: 2636-2648.
- Rosenthal DI, Lewin JS, Eisbruch A (2006) Prevention and treatment of dysphagia and aspiration after chemoradiation for head and neck cancer. J Clin Oncol 24: 2636-2643.
- Setton J, Lee NY, Riaz N, Huang SH, Waldron J, et al. (2015) A multi-institution pooled analysis of gastrostomy tube dependence in patients with oropharyngeal cancer treated with definitive intensity-modulated radiotherapy. Cancer 121: 294-301.
- Panwar A, Batra R, Lydiatt WM, Ganti AK (2014) Human papilloma virus positive oropharyngeal squamous cell carcinoma: a growing epidemic. Cancer Treat Rev 40: 215-219.
- Urban D, Corry J, Rischin D (2014) What is the best treatment for patients with human papillomavirus-positive and -negative oropharyngeal cancer? Cancer 120: 1462-1770.
- Cmelak AJ, Li S, Goldwasser MA, Murphy B, Cannon M, Pinto H, et al. (2007) Phase II trial of chemoradiation for organ preservation in resectable stage III or IV squamous cell carcinomas of the larynx or oropharynx: results of Eastern Cooperative Oncology Group Study E2399. J Clin Oncol 25: 3971-3977.
- Laskar SG, Swain M (2015) HPV positive oropharyngeal cancer and treatment deintensification: how pertinent is it? J Cancer Res Ther 11: 6-9.
- Marur S, Li S, Cmelak AJ, Gillison ML, Zhao WJ, et al. (2017) E1308: Phase II Trial of Induction Chemotherapy Followed by Reduced-Dose Radiation and Weekly Cetuximab in Patients With HPV-Associated Resectable Squamous Cell Carcinoma of the Oropharynx- ECOG-ACRIN Cancer Research Group. J Clin Oncol 35: 490-497.
- Vokes EE, Agrawal N, Seiwert TY (2015) HPV-Associated Head and Neck Cancer. J Natl Cancer Inst 107: djv344.
- Hoff CM (2012) Importance of hemoglobin concentration and its modification for the outcome of head and neck cancer patients treated with radiotherapy. Acta Oncol 51:419-32.
- Hoff CM, Grau C, Overgaard J (2012) Effect of smoking on oxygen delivery and outcome in patients treated with radiotherapy for head and neck squamous cell carcinoma: A prospective study. Radiother Oncol 103: 38-44.
- Rugg T, Saunders MI, Dische S (1990) Smoking and mucosal reactions to radiotherapy. Br J Radiol 63: 554-556.
- Chen SC, Lai YH, Huang BS, Lin CY, Fan KH, Chang JT (2015) Changes and predictors of radiation-induced oral mucositis in patients with oral cavity cancer during active treatment. Eur J Oncol Nurs 19:214-219.
- Porock D, Nikoletti S, Cameron F (2004) The relationship between factors that impair wound healing and the severity of acute radiation skin and mucosal toxicities in head and neck cancer. Cancer Nurs 27: 71-78.
- Dautzenberg B (2012) Methods and results of smoking cessation in cancer smoker's. Bull Cancer 99: 1007-10015.
- de Bruin-Visser JC, Ackerstaff AH, Rehorst H, Retel VP, Hilgers FJ (2012) Integration of a smoking cessation program in the treatment protocol for patients with head and neck and lung cancer. Eur Arch Otorhinolaryngol 269: 659-665.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi