Case Report, J Liver Disease Transplant Vol: 7 Issue: 2
Primary Hepatic Neuroendocrine Tumor: An Usual Tumor At An Unusual Site
Sugi RV*, Jeswanth S, Prabhakaran R, Senthil kumar P, Sugumar C and Ravichandran P
Institute of Surgical Gastroenterology & Liver Transplant, Government Stanley Medical College, Chennai, Tamil Nadu, India
*Corresponding Author : Sugi R V Subramaniam
Institute of Surgical Gastroenterology & Liver Transplant, Government Stanley Medical College, Chennai, Tamil Nadu, India
Tel: 917299058581
E-mail: drrvsugi@gmail.com
Received: May 14, 2018 Accepted: June 11, 2018 Published: June 16, 2018
Citation: Sugi RV, Jeswanth S, Prabhakaran R,Senthil kumar P, Sugumar C, et al. (2018) Primary Hepatic Neuroendocrine Tumor: An Usual Tumor at an Unusual Site. J Liver Disease Transplant 7:2. doi: 10.4172/2325-9612.1000163
Abstract
Primary hepatic neuroendocrine tumors (PHNETs) are extremely rare and asymptomatic. It is radiologically difficult to distinguish from other liver tumors, such as hepatocellular carcinoma (HCC) and intra hepatic cholangiocarcinoma. A 26 year old man who was referred to us for a liver mass which was discovered during evaluation for altered bowel habits. On abdominal computed tomography and MRI could not offer a conclusive diagnosis. Multiple biopsies were taken from the liver mass elsewhere, which offered variable diagnoses. Immunohistochemical examination revealed a grade 1 neuroendocrine tumor. Serum Chromogranin was grossly elevated. A search for a abdominal primary elsewhere with Esophagogastroduodenoscopy and colonoscopy was negative. A Ga 68 DOTONAC was done which confirmed the presence of liver only lesion. The patient underwent right hepatectomy. PHNETs are extremely rare, with only over 100 cases reported in literature. Because of the rarity of PHNETs, its clinical presentation, diagnosis and treatment outcomes are not well understood. Here, we report our experience with PHNET and its successful management with the help of immunohistochemistry and Ga 68 DOTONAC
Keywords: Primary hepatic neuroendocrine tumors (PHNETs); Hepatocellular carcinoma; Ga 68 DOTONAC
Introduction
Neuroendocrine tumors (NETs) primarily arising in the bronchopulmonary or gastrointestinal tracts including pancreas (GEP NETs) account for two third of all NETs found in the body [1]. There are two types of NETs namely neural neuroendocrine tumors and epithelial neuroendocrine tumors. Primary hepatic neuroendocrine tumor [PHNETs] was first reported by Edmondson in 1958 [2]. Since then only close to a hundred cases of PHNETs have been documented in literature [3]. These tumors develop in intrahepatic bile duct epithelium and have an extremely low incidence of 0.17% [4]. The peculiar characteristics of PHNETs are that they occur at a relatively young age, with no known gender predominance, mostly asymptomatic, require immunohistochemistry for diagnosis and have multiple therapeutic approaches including hepatectomy, transhepatic arterial chemoembolization, radiofrequency ablation and even liver transplantation.
Case Presentation
26 Year old young male presented with complaints of altered bowel habits for 6 months; passing semisolid stools immediately after taking food. He gave history of significant loss of weight with no loss of appetite. No c/o abdominal pain, distension or vomiting. No other specific complaints were present. He was a known hypothyroid and was on Thyronorm. He was not suffering from any other comorbid illnesses.
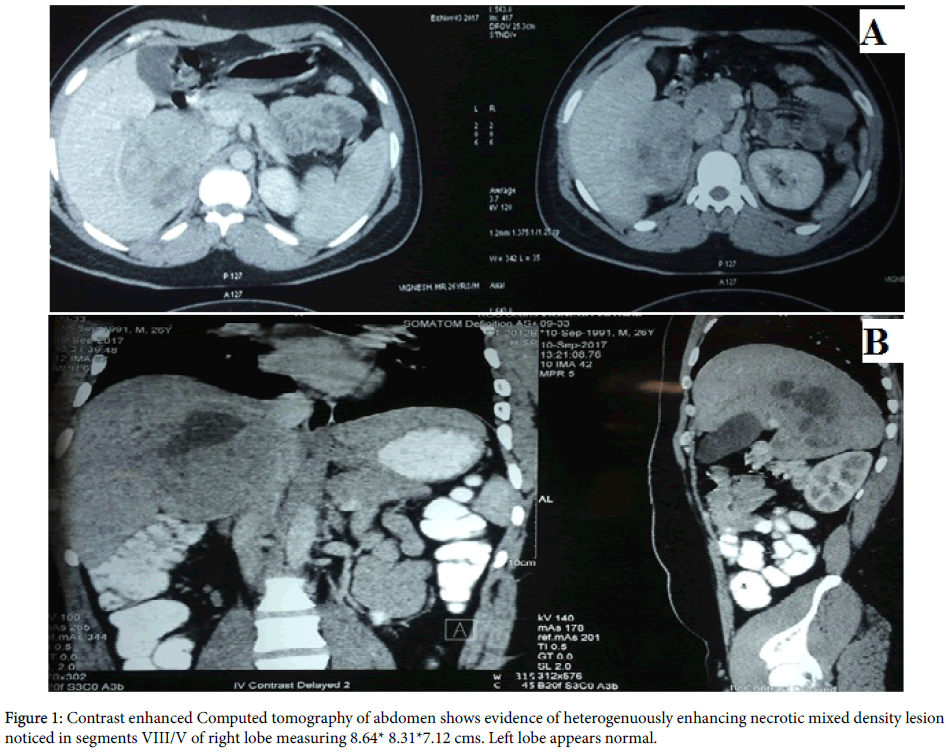
He did not undergo any previous abdominal surgeries. On examination his general condition was good. He was neither pale nor icteric. He was well preserved and well nourished. His abdominal examination revealed a soft abdomen with no palpable mass or organomegaly. Other system examinations were normal. Patient was evaluated elsewhere with contrast enhanced computed tomography of the abdomen which showed an heterogenuously enhancing necrotic mixed density lesion noticed in segments VIII/V of right lobe measuring 8.64 × 8.31 × 7.12 cms (Figure 1). Left lobe appeared normal. There was no dilation of intra hepatic biliary radicles. He was already subjected to multiple biopsies within a short span of 12 days at various hospitals due to inconsistent findings.
His initial FNAC was suggestive of a benign lesion. He underwent percutaneous liver biopsy which was suggestive of either a Hepatocellular carcinoma or Hepatoblastoma with macrotrabecular pattern. A repeat biopsy was done which was in favour of a round cell tumor. Immunohistochemical staining features were consistent with Grade 1, Neuroendocrine tumor. His blood investigations were normal. His liver function tests were also normal. Serum Alpha Feto Protein was within normal limits [1.59 ng/ml]. Serum Chromogranin A was elevated [638 ng/ml].
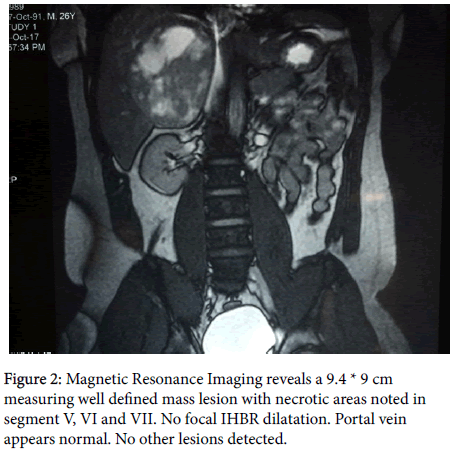
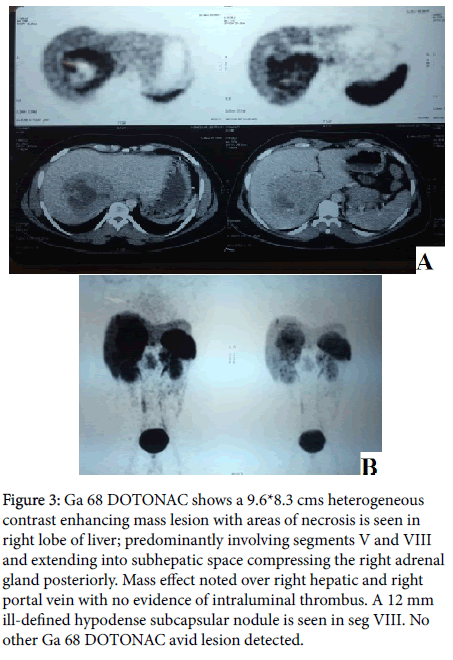
Upper Gastrointestinal endoscopy was normal. Colonoscopy revealed a normal study upto caecum. Magnetic Resonance Imaging (Figure 2) of the abdomen revealed a 9.4 × 9 cm measuring well defined mass lesion with necrotic areas noted in segment V, VI and VII; no focal IHBR dilatation. Portal vein appeared normal. No other focal lesions were detected. With the strong suspicion of neuroendocrine tumor of liver, given the very rare incidence of primary neuroendocrine tumour of liver, we proceeded with Ga 68 DOTONAC PET/CT to rule out presence of NET elsewhere in the abdomen (Figure 3). It revealed a 9.6*8.3 cm heterogenous contrast enhancing mass lesion with areas of necrosis is seen in right lobe of liver; predominantly involving segments V and VIII and extending into sub hepatic space compressing the right adrenal gland posteriorly. Mass effect was noted over right hepatic and right portal vein with no evidence of intraluminal thrombus. A 12 mm ill-defined hypodense subcapsular nodule was seen in segment VIII. No other Ga 68 DOTONAC avid lesion detected. On exploration, 12 × 12 cm sized space occupying lesion predominantly involving caudate lobe and segment VII.
Figure 3: Ga 68 DOTONAC shows a 9.6*8.3 cms heterogeneous contrast enhancing mass lesion with areas of necrosis is seen in right lobe of liver; predominantly involving segments V and VIII and extending into subhepatic space compressing the right adrenal gland posteriorly. Mass effect noted over right hepatic and right portal vein with no evidence of intraluminal thrombus. A 12 mm ill-defined hypodense subcapsular nodule is seen in seg VIII. No other Ga 68 DOTONAC avid lesion detected.
Another 2 × 2 cm sized lesion was noted in segment VIII. Segments V and VI were relatively free of tumor. Hilar pedicle was pushed anteriorly by the caudate lobe lesion. Right hepatic duct, confluence and common hepatic duct were thinned out and compressed by the tumor. Middle hepatic vein [MHV] was coursing over the tumor border. Numerous peritumoral vessels were present. Left lobe was adequate with absence of any surface lesion. There was no aberrant vascular anatomy. Right hepatectomy with caudate lobe excision with preservation of MHV has done. On histopathological examination it was a multifocal tumor with two lesions about 11 × 7 cm in caudate lobe and 1 × 1 cm in segment VIII. It was a Neuroendocrine tumor with low mitotic rate and Ki67 labelling index. Lymphovascular and perineural invasion was not identified. Three isolated lymph nodes showed reactive follicular hyperplasia. Final impression was a Primary hepatic neuroendocrine tumor (PHNETs).
Discussion
Primary NETs are most commonly seen in the lung and other parts of gastrointestinal tract including pancreas. However primary NETs arising from liver are extremely rare. Recent WHO Classification of NETs classifies into three grades. G1 and G2 NETs are low grade neoplasms with good prognosis, whereas neuroendocrine carcinomas (NECs) are G3 neoplasms which are structurally similar to NETs [5]. Synaptophysin (Syn) and chromogranin A (CgA) are diffusely expressed by these tumours. Nuclear atypia, focal necrosis, high mitosis rate (>20/10 HPF) are characteristics of malignancy. PHNETs have a better prognosis than Hepatocellular carcinoma. Characteristic local invasion, metastases, and serious complications of carcinoid syndrome contribute to the poor outcome. Carcinoid syndrome seen in <10% of patients with gastrointestinal NETs associated with liver metastasis, rarely observed in PHNET patients [6].
Positive staining for chromaffin granule (CgA), synaptophysin (Syn), and neuron specific enolase (NSE) are important in pathological diagnosis. Non-specific symptoms, such as abdominal pain and distension, may be associated with the early stages of this disease. As PHNETs are rare, slow growing and asymptomatic, early stage diagnosis may be difficult. PHNETs are usually seen in fifth decade.
This lesion is most commonly located in the right lobe of the liver [7]. It slowly metastasizes to the other lobe. PHNETs can be multifocal at times, but are usually solitary space occupying lesions of liver [8]. Origin of PHNETs is believed to be the NET cells which may spread to the intrahepatic biliary tract and undergo malignant transformation [9]. Other possible explanations are that malignant stem cells may be transdifferentiated to NET cells or hepatocellular carcinomas might undergo neuroendocrine differentiation [10].
Immunohistochemical analysis is the most effective method using CK AE1̸AE3, synaptophysin, chromogranin A and CD56. A definitive diagnosis of PHNETs can be made with tumour markers synaptophysin and chromogranin A [11]. Quantification of chromogranin A in the plasma used for the follow up evaluation of NETs. Surgical treatment is the only curative treatment with a 5 and 10 year survival rates of 78 and 59% respectively [12].
Factors associated with best prognosis includes the absence of lymph nodal metastases and distant metastases. PHNETs that are advanced or metastatic need alternate therapies. TACE performed with cisplatin was proven to be the most effective therapy for PHNETs with intrahepatic metastasis [13]. Radio Frequency Ablation has been successfully employed for smaller lesions <3 cm [14]. A liver Transplantation can be done in extreme cases which are nonmetastatic and unresectable [15].
Conclusion
PHNETs is not common, hence it is commonly misdiagnosed. Early diagnosis is crucial although early recognition is not that easy. Primary hepatic neuroendocrine tumor of liver should still be considered as a possible differential diagnosis of liver space occupying lesions. When hepatic tumor is considered to be NET, first a detailed systemic search for a primary tumor is mandatory to exclude metastatic NET, as primary hepatic NETs are very rare compared to metastatic ones. Imaging with Ga 68 DOTONAC and Immunohistochemistry are crucial for diagnosis. Upon exact diagnosis of primary hepatic NET, liver resection should be the treatment of choice for successful longterm treatment, with TACE and RFA reserved for unresectable PHNETs.
References
- Modlin IM, Sandor A, Tang LH, Kidd M, Zelterman D (1997) A 40-Year Analysis of 265 Gastric Carcinoids. Am J Gastroenterol 92: 633-638.
- Edmondson H (1958) Tumor of the Liver and Intrahepatic Bile Duct: Atlas of Tumor Pathology Section 7, fascicle 25. Armed Forces Institute of Pathology, Washington.
- Schwartz G, Colanta A, Gaetz H, Olichney J, Attiyeh F (2008) Primary Carcinoid Tumors of the Liver. World J Surg Oncol 6: 91.
- Gravante G, Liguori CN, Overton J, Manzia TM, Orlando G (2008) Primary Carcinoids of the Liver: A Review of Symptoms, Diagnosis and Treatments. Dig Surg 25: 364-368.
- Bosman FT, Carneiro F, Hruban RH, Theise ND (2010) WHO Classification of Tumours of the Digestive System, WHO, Geneva, Switzerland.
- Mehta DC, Warner RR, Parnes I, Weiss M (1996) An 18-year Follow-Up of Primary Hepatic Carcinoid With Carcinoid Syndrome. J Clin Gastroenterol 23: 60-62.
- Gurung A, Yoshida EM, Scudamore CH, Hashim A, Erb SR, et al. (2012) Primary Hepatic Neuroendocrine Tumour Requiring Live Donor Liver Transplantation: Case Report and Concise Review. Ann Hepatol 11: 715-720.
- Zhu Z, Zhao XM, CW Z (2010) Imaging Features of Primary Hepatic Endocrine Carcinoma. Chin J Med Imaging Technol 26: 721-723.
- Kaya G, Pasche C, Osterheld MC, Chaubert P, Fontolliet C (2001) Primary Neuroendocrine Carcinoma of The Liver: An Autopsy Case. Pathol Int 51: 874-878.
- Zhao M, Laissue JA, Zimmermann A (1993) “Neuroendocrine” Differentiation in Hepatocellular Carcinomas (Hccs): Immunohistochemical Reactivity Is Related To Distinct Tumor Cell Types, But Not To Tumor Grade. Histopathol 8: 617-626.
- Sundin A, Eriksson B, Bergström M, Långström B, Oberg K, et al. (2004) PET in the Diagnosis of Neuroendocrine Tumors. An NY Acad Sci 14: 246-257.
- Knox CD, Anderson CD, Lamps LW, Adkins RB, Pinson CW (2003) Long-term Survival after Resection for Primary Hepatic Carcinoid Tumor. Ann Surg Oncol 10: 1171-1175.
- Yao KA, Talamonti MS, Nemcek A, Angelos P, Chrisman H, et al (2001) Indications And Results Of Liver Resection And Hepatic Chemoembolization For Metastatic Gastrointestinal Neuroendocrine Tumors. Surgery 130: 677-682.
- Gamblin TC, Christians K, Pappas SG (2011) Radiofrequency Ablation of Neuroendocrine Hepatic Metastasis. Surg Oncol Clin N Am 20: 273-279.
- Gurung A, Yoshida EM, Scudamore CH, Hashim A, Erb SR, et al. (2012) Primary hepatic neuroendocrine tumour requiring live donor liver transplantation: Case report and concise review. Ann Hepatol 11: 715-720.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi