Case Report, Int J Ophthalmic Pathol Vol: 7 Issue: 3
Primary Invasive Orbital Aspergillosis in an Immunocompetent Patient
Sonia Phulke*
Department Occuloplastics and Glaucoma Services, Drishti Eye Hospital, Panchkula-134106, Haryana, India
*Corresponding Author : Sonia Phulke
Department Occuloplastics and Glaucoma Services, Drishti Eye Hospital, Panchkula-134106, Haryana, India
Tel: + 91-9876641140
E-mail: soniavaidya2010@yahoo.com
Received: February 02, 2018 Accepted: May 16, 2018 Published: May 23, 2018
Citation: Phulke S (2018) Primary Invasive Orbital Aspergillosis in an Immunocompetent Patient. Int J Ophthalmic Pathol 7:2.doi: 10.4172/2324-8599.1000226
Abstract
Primary invasive orbital aspergillosis is a rare but fatal entity. It is commonly seen in immunocompromised patients with sinus pathology. The clinical spectrum of disease is variable which could delay in diagnosis and management of patients. Treatment includes surgical excision and systemic antifungals. Here we report a case of primary invasive orbital aspergillosis an immune-competent patient who managed successfully with surgical excision and a course of oral antifungal. The patient had not shown any recurrence in follow up period of one year.
Keywords: Orbital; Aspergillosis; Antifungals
Introduction
Orbital Aspergillosis is relatively uncommon, but a fatal and lifethreatening condition commonly reported in immune-compromised patients. It is very rarely being reported in immune-competent patients. Clinical presentation of the disease is variable, which could delay in diagnosis and management. The mainstays of treatment include debridement or excision with systemic antifungal. Here we report a case of primary invasive orbital Aspergillosis in which location was very unusual and the patient was neither immunecompromised nor having any sinus pathology.
Case Report
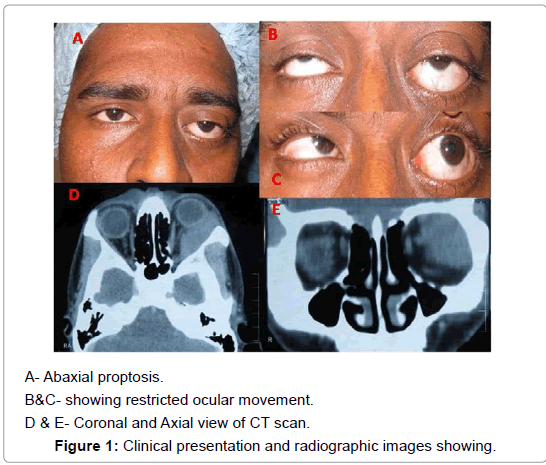
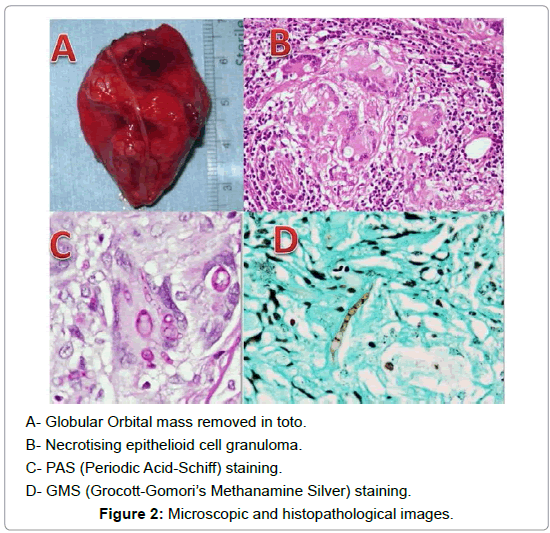
A 23-year-old Indian male presented in Oculoplastic services with chief complaints of forward protrusion of left eye for nine months. The protrusion was gradually progressive and painless. It was associated with diplopia in lateral gaze. There was no significant history of any systemic disease and or sinusitis; however, he gave the history of alcohol intake, smoking, and addiction to locally prepared flavoured tobacco leaves called` Khaini` a year prior to developing symptoms. On ocular examination, his best corrected visual acuity was 20⁄20 and 20⁄30 OD and OS respectively. The left eye ball was proposed forwards and displaced upward. On palpation a firm, nontender, non-pulsatile, non-compressible mass was felt in the superiortemporal quadrant of the left eye. Its anterior surface was lobular, approximately 4 cm in size and extended below the lateral canthus.The medial border was abutting the globe and its posterior extent could not be reached. The overlying skin was free. Trans illumination was absent. Hertel exophthalmometry was 18 mm in the right eye and 25 mm in left eye Ocular movements were restricted laterally and in up gaze (Figures 1A-1C). Intraocular pressures were 12 mmHg and 14 mmHg OD and OS, respectively. Anterior and posterior segment examination was normal in both eyes. In view of the long duration of symptoms, absence of pain, palpation of the mass in the superior-temporal quadrant with inferomedial displacement of the globe, a provisional diagnosis of benign lacrimal gland tumour was made. A contrast-enhanced computer tomography (CECT) scan of the orbit and head showed a well-defined, homogenous mass in the superior-temporal and lateral quadrant, involving extraconal as well as intraconal. Compartment in the left eye. It was indenting the globe medially and posteriorly just reaching up to the orbital apex (Figures 1D and 1E). A supero-lateral route was taken to approach the orbit and total mass excision done. Intraoperative it was found to be loosely adherent to the surrounding fat and firmly to the orbital apex. On gross examination, the specimen was fusiform in shape with broad anterior and tapering posterior end, measuring 4.5 cm in maximum dimension (Figure 2A). There was a long thick nerve along its lateral surface. Its external surface was congested. Microscopy showed multiple coalescent necrotizing epithelia cell granulomas along with multiple langhan type multinucleated giant cells (Figure 2B). The necrotizing process caused entrapment of nerves and involved the adjacent adipose tissue. Giant cells showed engulfment of fungal hyphae, which were septate, slender and had acute angle branching consistent with the morphology of Aspergillums (Figures 2C and 2D). Postoperatively there was a minimal restriction of lateral gaze. Magnetic resonance imaging (MRI) was planned and did not show any nasal pathology. He was put on oral voriconazole and his liver function tests were monitored on regular basis for drug toxicity. Two months later, the drug was switched over to oral Itraconazole. Since no recurrence of the disease was found on further follow-up, antifungals were stopped after four months of surgery.
Discussion
Aspergillus is a ubiquitous organism, usually found in soil. Other than Aspergillus fumigates, Aspergillus flavus, Aspergillus niger, Aspergillus. oxyzae are the common pathogens seen in affected human being. The orbital aspergillosis can be primarily orbital, sino-orbital or with central nervous system involvement. It could be an invasive and non-invasive type and both types can occur in immune-compromised as well as in immune-competent individuals [1]. The etiologic behind the primary orbital aspergillosis is not clear, but reports from tropical countries suggest an important role of hot humid climate in fungal growth [2,3]. Mortality and morbidity rates are higher in invasive orbital Aspergillosis than non-invasive one.
Cases of isolated orbital Aspergillosis in healthy immunecompetent patients are sparse in literature. Orbital Aspergillosis is generally a disease of elderly; however, Asians patients have shown younger age (mean 36.8 years) of presentation [4-7]. The difference could be because of climatic conditions and work profiles of the patients. Sinusitis is a well-established risk factor for orbital aspergillosis [8]. Orbital aspergillosis usually has an insidious course, may be confused with other orbital inflammatory pathologies like temporal arteritis, pseudotumors, orbital cellulitis and sometimes with malignancy [9-12]. The most common presentation is painless or painful progressive apoptosis with restricted extra ocular movements. The chronic orbital aspergillosis may cause local tissue destruction without actual invasion by the organism, such type of presentation carries good prognosis [13]. Pushker et al. [5] reported 15 cases of primary invasive orbital aspergillosis in immunocompetent healthy individuals, among them three did not have any signs of associated sinusitis or any other systemic disease. Similarly, among the 35 cases of primary orbital aspergillosis by Mody KH et al, five did not have any sinus or other systemic involvement [6]. Other than sinusitis, trauma, facial surgery, immunocompromised states including acquired immunodeficiency syndrome, neutropenia and diabetes mellitus are also well-known risk factors [14,15]. Imaging features sinoorbital or orbital aspergillosis are nonspecific, although subtle signs of sinus involvement like mucosal thickening can be effectively picked up by MRI. Sivak Callcott et al. [13] suggested that sphenoid sinus assessment on MRI scan can be helpful in early detection of lesions. Incisional biopsy along with microbiological workup is essential for definitive diagnosis. The fine needle aspiration cytology could be an important tool for diagnosis, but its role remains unclear.
Our case is unique due to the fact that this lesion was occupying the superotemporal orbit with no proximity to the adjacent sinuses and just sparing the apex. Because of its location and clinical features, a diagnosis of lacrimal gland fossa mass, with a high possibility of lacrimal gland tumor was kept.
No definitive treatment protocol is set for treatment of orbital aspergillosis. Amphotericin B is being considered as a gold standard treatment for orbital aspergillosis. However, its use is limited because of its associated systemic toxicity. Initial treatment with high dose of amphotericin B followed by a long course of Itraconazole is most commonly used for treatment. But recent reports have shown successful results with no recurrence of the disease by complete surgical excision of mass with the postoperative course of newer antifungal drugs like voriconazole [7,15]. Our patient was also treated with voriconazole without any recurrence or fresh symptoms.
Conclusion
This case is being reported due to its rarity as in this case, the atypical location of mass was in the lacrimal gland fossa of the orbit without any proximity to sinus or its involvement. The author per se could not find any previously published case report having unilateral, painless superior-temporal orbital mass in a young patient, who recovered completely by surgical excision of mass with no recurrence of the disease in follow up period.
References
- Levin LA, Avery R, Shore JW, Woog JJ, Baker AS (1996) The spectrum of orbital aspergillosis: A clinicopathologic review. Surv Ophthalmol 41: 142-154.
- Hedges TR, Leung LS (1976) Parasellar and orbital apex syndrome caused by aspergillosis. Neurology 26: 117-120.
- Green WR, Font RL, Zimmerman LE (1969) Aspergillosis of the orbit: Report of ten cases and review of the literature. Arch Ophthalmol 82: 302-313.
- Hutnik CM, Nicolle DA, Munoz DG (1997) Orbital aspergillosis a fatal masquerade. J Neuroophthalmol 17: 257-261.
- Pushker N, Meel R, Kashyap S, Bajaj MS, Sen S (2011) Invasive aspergillosis of orbit in immunocompetent patients: Treatment and outcome. Ophthalmology 9: 1886-1891.
- Mody KH, Ali MJ, Vemuganti GK, Nalamada S, Naik MN, et al (2014) Orbital aspergillosis in immunocompetent patients. Br J Ophthalmol 98: 1379-1384.
- Aggarwal E, Mulay K, Menon V, Sundar G, Honavar SG, et al (2016) Isolated orbital aspergillosis in immunocompetent patients: A Multicenter Study. Am J Ophthalmol 165: 125-132.
- Whitehurst FO, Liston TE (1981) Orbital aspergillosis: Report of a case in a child. J Pediatr Ophthalmol Strabismus18: 50-54.
- Spoor TC, Hartel WC, Harding S, Kocher G (1982) Aspergillosis presenting as a corticosteroid-responsive optic neuropathy. J Clin Neuroophthalmol 2: 103-107.
- Austin P, Dekker A, Kennerdell JS (1983) Orbital aspergillosis: Report of a case diagnosed by fine needle aspiration biopsy. Acta Cytol 27: 166-169.
- Yumoto E, Kitani S, Okamura H, Yanagihara N (1985) Sino-orbital aspergillosis associated with total ophthalmoplegia. Laryngoscope 95: 190-192.
- Denning DW (2000) Aspergillus species. In Principle and practice of infectious disease (5th edtn), Churchill Livingstone, Elsevier, Philadelphia.
- Sivak-Callcott JA, Livesley N, Nugent RA, Ramussen SL, Saeed P et al. (2004) localized invasive sino-orbital aspergillosis;characteristic features. Br J Ophthalmol 88: 681-687.
- DeShazo RD, Chapin K, Swain RE (1997) Fungal sinusitis. N Engl J Med 337: 254-259.
- De Sarro A, La Camera E, Fera MT (2008) New investigational triazole agents for the treatment of invasive fungal infections. J Chemother 20: 661-671.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi