Research Article, J Trauma Stress Disor Treat Vol: 6 Issue: 4
Psychobiological Resilience: A Longitudinal Qualitative Exploratory Approach
Mélanie Laurent1, Pierre Bustany2, Claude de Tychey3*, Joelle Lighezzolo-Alnot4, Jean Paysant5, Marianne Krier6 and Boris Cyrulnik7
1Department of clinical Psychology (Interpsy Laboratory)-University of Lorraine- France
2Department of Pharmacology-University of Caen Normandie-Service of Medical Pharmacology
3Department of clinical Psychology (Interpsy Laboratory)-University of Lorraine- France
4Department of clinical Psychology (Interpsy Laboratory)-University of Lorraine- France
5Department of functional Physical Medecine,Center of functional adults readaptation- Nancy France
6Clinical psychologist and Neuro psychologist-Center of functional adults readaptation
7Neuropsychiatrist.University of Toulon France
*Corresponding Author : Claude de Tychey
Professor of clinical psychology, University of Lorraine Nancy-France
Tel: 09 54 98 48 57
E-mail: claude. de-tychey@univ-lorraine.fr
Received: September 14, 2017 Accepted: October 17, 2017 Published: October 24, 2017
Citation: Laurent M, Bustany P, de Tychey C, Lighezzolo-Alnot J, Paysant J, et al.(2017) Psychobiological Resilience: A Longitudinal Qualitative Exploratory Approach. J Trauma Stress Disor Treat 6:4. doi: 10.4172/2324-8947.1000180
Abstract
Objective: To introduce researchers to a new qualitative method for longitudinally exploring the links between biological resilience and psychological resilience among adults having been confronted with the risk of death.
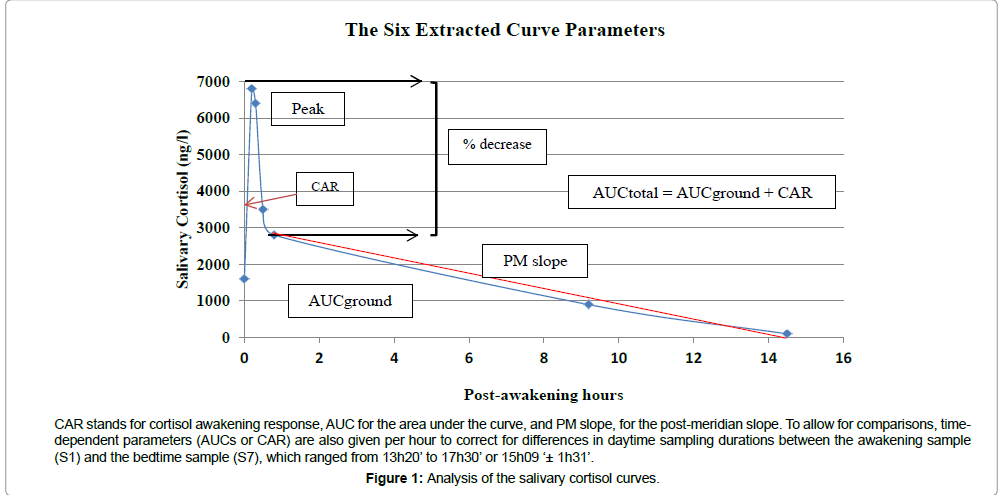
Methods: Biological resilience was assessed in three participants who were respectively resilient, non-resilient, and recovered, within two months following a traumatic event involving the risk of death, and then again after 10 months, 17 months, and 24 months. Various markers of diurnal cortisol, including CAR (cortisol awakening response), area under the curve (AUC), diurnal slope, peak, etc., were taken into account. Psychological resilience was approached via the absence of psychopathological symptoms of PTSD, anxiety, and/or depression, measured at the same times using the Damiani-Fradin Traumaq Scale, the Spielberger State-Trait Anxiety Questionnaire, and the Beck Depression Inventory (BDIII). We hypothesized that psychological resilience is determined by the quality of the imaginary space and the mentalization process measured on the Rorschach test.
Results: For the resilient and recovered subjects, psychological resilience preceded biological resilience, whereas for the nonresilient subject, the time curves of the biological and psychological markers were altered from the beginning and remained so.
Conclusion: The present study underlines the interest to study simultaneously biological and psychological parameters in view of accounting for interrelations between neurobiological resilience and psychological resilience. Further researches, involving this innovative approach, are suggested.
Keywords: Diurnal cortisol; Resilience; Trauma; Case studies-personality
Introduction
The present article is organized as follows. After a short review of the recent literature on the links between the neurobiology of cortisol levels and certain forms of psychopathology (PTSD, depression, anxiety disorders), we will briefly define the psychodynamic model of resilience [1,2] underlying this exploratory study. Next, we will present an original, longitudinal, qualitative, and exploratory research method, which, to our knowledge, has never been used in prior research. Our objective will be to address the relationships between the neurobiological and psychological characteristics of three individuals who underwent a traumatic, life-threatening event. After that, we will analyze and discuss the respective time courses of the psychological variables chosen to characterize these individuals, and the associated cortisol-related parameters reflecting the neurobiological impact of the trauma, in view of determining whether these two facets describe a parallel relationship of simultaneity or a dynamic process modulated by mutual interdependence. Lastly, we propose some potential avenues of research for testing the conclusions tentatively drawn here from the clinical cases presented. Future research could confirm their validity by comparing three subgroups of individuals presenting the differential characteristics possessed by the three subjects analyzed in this preliminary qualitative study.
The merits of using cortisol as a marker of chronic stress and psychiatric pathology have been demonstrated [3-5]. More specifically, the cortisol awakening response (CAR), and cortisol evolution throughout the day, has been widely studied, even though, as Dantzer and Kalin pointed out, the methods used by researchers to study CAR alterations as a function of psychosocial variables have been vastly different [6]. It has been shown, for example, that in cases where a traumatic event occurs, the presence of PTSD symptoms is correlated with cortisol levels [4], i.e., a low CAR and a smaller area under the curve [7-11].
On another level, CAR is also a useful neurobiological indicator of depression. A review of the literature by Herane et al. [4] brought out a strong link between high cortisol levels and depression. Several studies have confirmed this link. Herane et al. [4] themselves found high concentrations of cortisol in adults undergoing a major episode of depression; Van Santen et al. [12] showed that an elevated CAR was associated with the psychological trait of reactivity to despair, which is known to be correlated with depression and suicide; Morris and Rao [13], who compared adolescents presenting or not presenting a major depressive episode, found that depressed subjects had a higher cortisol peak and a greater area under the diurnal curve.
The links between cortisol levels and anxiety disorders is equally interesting. Mantella et al. [14] compared 71 adults over 60 years of age who exhibited a general anxiety disorder (assessed on the anxiety scale and on Hamilton’s depression scale) to 40 matched control subjects. The results showed that the anxious group had a higher baseline level of cortisol, higher peaks, and a greater area under the curve than the non-anxious subjects did. These three bodies of data suggest that it is useful to study cortisol levels to account for three major personality disorganization disorders (post-traumatic stress, depression, and anxiety) and their impact at the neurobiological level. We can contend, however, that not all individuals confronted with traumatic events necessarily develop disorganizations and upheavals at the neurobiological and psychopathological levels. Some individuals are able to withstand the traumas they undergo. The concept of resilience applies to this clinical reality. Binder and Holsboer [15] define resilience as the absence of psychiatric symptoms. This definition facilitates clinical evaluation as compared to the use of resilience scales, none of which can be related to our theoretical psychodynamic model. Resilience is posited to be a protective factor that modulates the negative consequences of chronic stress [16-19]. The neurobiological determinants of resilience have been widely researched [20]. A laboratory study conducted by Galatzer-Levy et al. [17] showed that police officers who exhibited significant increases in cortisol in response to experimental stress followed trajectories of resilience and recovery for four years, whereas those who exhibited no significant change in cortisol levels in response to the experimental situation followed trajectories of chronic increasing distress. For Mizuno et al. and Walker et al. [5,21], however, the existence of causal relationships between the neurobiological markers and psychological variables of individuals assessed in real life remains to be demonstrated, due to a scarcity of studies. Walker et al. [5] raised the unresolved fundamental research question, for example, of whether the observed neurobiological differences between healthy subjects and subjects with PTSD are the consequence of the psychological trauma, or of a preexisting low level of phenotypical resilience before the traumatic event. The only way to arrive at an answer to this question, both for these authors and for Mizuno et al. [21], would be to conduct prospective studies. This question underlies the first aim of the qualitative exploratory study presented here, which proposes a methodological model for future research designed to detect causality links or correlations between neurobiological resilience and psychological resilience. Neurobiological resilience will be assessed via longitudinal testing of cortisol levels among subjects exposed to a major traumatic event. Psychological resilience will also be assessed prospectively, firstly, using psychological questionnaires and a clinical interview aimed at testing for the absence or presence of symptoms after the traumatic event, and secondly, via a projective clinical investigation using the Rorschach test, to assess the two fundamental factors of intrapsychic functioning in our psychodynamic model of psychological resilience. This is an original research perspective which, to our knowledge, has never been implemented in this field. According to Widlöcher [22,23], its use in psychodynamic clinical research is fully justified. It relies on a comparative study of contrasted clinical cases and can be used to explore new problems with new hypotheses, hence serving as a basis for future quantitative research. On the theoretical level, we will base our study on the psychodynamic model of resilience developed in France [1,2]. This model posits, firstly, that one cannot speak of resilience unless there is prior confrontation with an actual, potentially traumatic event that differs from a simple state of minor existential stress [24]. To make it easier to operationalize resilience, and knowing that each individual may, in his or her life, encounter a large number of potentially traumatic situations, we chose one such situation that also has the quality of being initially non-representable (which grounds the reality of the trauma in our theoretical model): direct confrontation with the reality of death, as verbalized after the event by each subject studied.
In our model, the main protective intrapsychic factor that ensures short-term psychological resistance to the traumatic event is the defense mechanism, constituted by recourse to the imaginary space in the face of a traumatic reality that is too invasive [25]. The imaginary function allows individuals to immediately rid themselves of “the intolerable” by reconstructing a different reality and then fantasizing the steps needed to attain it, to make it concrete. Our first hypothesis, then, is that the richness versus paucity of the imaginary space should differentiate a subject who is initially psychologically resilient or becomes so, from a psychologically non-resilient one. The second intrapsychic factor that ensures long-term psychological resilience is the quality of the mentalization process. This concept has been given a number of complex definitions in clinical psychodynamics [26]. Our definition, based on Bergeret’s [25] model, is two-faceted. Mentalization is posited, first, to be the ability to transform inner drive excitations with a sexual or aggressive side, into internal representations of words that can be shared with another person. It then involves the ability to elaborate the intense displeasure affects (anguish, depression, rage, resentment, outrage, guilt, shame) that are unavoidably triggered by the traumatic situation, by putting them into words so that they can be linked to representations communicable via language to someone else and then symbolized. In this respect, mentalization (although much broader) can be related to the concept of mindfulness, a term employed today in the English-speaking clinical research [27,28]. Mindfulness is the ability to identify and describe one’s inner states and to accept negative thoughts and feelings. Empirical research seems to clearly argue in favor of an impact of mindfulness on psychological resilience. For Trousselard et al. [27], for instance, studies using various scales to measure mindfulness have found positive correlations with wellbeing, and negative correlations with neuroticism and measures of emotional disturbance [29-31]. According to Daubenmier et al.’s [28] review, the impact of mindfulness on neurobiological parameters has been demonstrated. In the studies conducted by that research team, CAR was linked to psychological distress solely in cases of a low dispositional level of mindfulness. Moreover, mindfulness has been said to permit deactivation of the medial prefrontal cortex in response to negative affective stimuli, suggesting reduced emotion-related rumination [32,33]. In other studies, high dispositional mindfulness was found to be correlated with reduced amygdala activity during rest and to a smaller volume of the right amygdala [34,35] . In the light of the above parallel, it seems legitimate to set forth a second hypothesis: mentalization — defined here in terms of the quality of the subject’s symbolization of representations and affects — should enable us to differentiate between resilient individuals, individuals who are nonresilient and remain so over time, and individuals who were nonresilient at the onset and then recover.
To detect causal relations between neurobiological resilience and psychological resilience, we will set forth our third hypothesis in the form of three mutually exclusive alternatives regarding what might happen during longitudinal follow-up: (1) Neurobiological change precedes and thus determines changes in psychological resilience or non-resilience. (2) Psychological resilience precedes and thus determines neurobiological resilience. (3) There is strict concomitance between psychological resilience and neurobiological resilience, and between neurobiological non-resilience and psychological nonresilience.
Materials and Method
Participants and procedure
This study was approved by the Northwest French Committee for Person Protection III (No. CPP A13-D01-Vol 15). All individuals contacted agreed to participate by signing a written consent form. Clinical neurobiological data and psychological data were analyzed separately, in a double blind procedure, by one member of each of the two research teams. The coders were unaware of the subjects’ clinical status (resilient, non-resilient and recovered). Each subject was assessed longitudinally four times: T1 within two months after the traumatic event, T2 after 10 months, T3 after 17 months, and T4 after 24 months.
Measuring biological resilience via salivary cortisol levels
In order to control for variations in diurnal cortisol levels, cortisol was measured seven times using 0.5 ml cortisol Salivettes (five samples in the morning: one upon awakening and then every 15 minutes for one hour; one at 6 p.m., and one at bedtime). Based on the available literature, we excluded subjects presenting any of the following: subjects being treated with corticosteroids or beta-blockers or who had been taking Ibuprofen for more than three days; subjects with a BMI over 35; subjects with a history of chronic, disabling psychiatric disorders who were under long-term treatment; brain-damaged (past or recent) subjects who had gone into a coma or lost consciousness for more than 15 minutes; subjects with chronic alcoholism; and past or present hard-drug users. We also wanted to eliminate the gender factor, known to affect cortisol levels, so we chose only men for the clinical comparisons, as in other quantitative studies [36,37].
We were unable to use all of the indicators proposed by Charney [38] to study neurobiological resilience because they are too complex to assess outside of a laboratory. On the other hand, we followed Walker et al. [5] recommendation to not settle for only one cortisol indicator (e.g., CAR) so as to be able to better account for the resilience or non-resilience of each subject. We therefore analyzed all of the cortisol-related indicators in order to determine the most discriminating ones. We then compared the data of our three subjects to the reference values in this domain, based on the hypothesis that the values of a non-resilient subject should be significantly different from the reference values, that is, at least twice as high or twice as low [39].
Presentation of the three subjects
Mister K, age 42, was injured in a car accident caused by ice on the road. He was convinced right after the accident that he would die on the pavement while waiting for help. He explained that this conviction was related to a similar, serious accident his brother had had a few years earlier, at which time the doctors had said he would not survive. Mister K suffered multiple fractures (in the neck, femoral bone, and right arm) and three fingers had to be amputated.
Mister B, a young 22-year-old bachelor, was injured in a motorcycle accident at an intersection where the driver of a car failed to stop at the stop sign. He too was convinced that he might die. He also suffered multiple fractures (upper and lower limbs). Several nerves were severed during the accident, so he could no longer work in his trade (ornamental metal casting).
Mister M, a 39-year-old bachelor with no children, was injured in a car accident while attempting to avoid an animal on an expressway. The accident resulted in a pile-up in which other individuals were also injured and which caused Mister M to believe he had looked death in the face. His physical injuries included multiple fractures (pelvis, several vertebrae, and leg and arm bones). The final outcomes of some of his fractures are still unknown since they are not yet fully healed. Mister M is a traveling salesman, but this event has made him aware that he no longer wants to risk his life daily on the road, for an occupation that provides him with little personal fulfillment.
Measures of psychological resilience and its two intrapsychic factors
Resilience was defined above as the ability to withstand a trauma involving a genuine risk of death, like that undergone by each the subjects in our study. It was assessed here via the absence of symptoms of disturbances in the three major psychological spheres likely to be affected: post-traumatic stress, anxiety, and depression. Each subject was given the battery of psychological tests presented below at four times during the 24 months of follow-up. Post-traumatic stress was measured using the validated French questionnaire called Trauma [40]. The questionnaire contains ten scales measuring immediate physical and psychic reactions during the event, current feelings since the event occurred, sleep disorders, insecurity and phobic avoidance, irritability and hypervigilance, psychosomatic reactions and physical problems, cognitive impairment, depressive disorders, guilt feelings or shame, low self-esteem, and quality of life. The raw scores obtained on each scale are combined to give an overall score that places each subject in one of five classes. Class 1 corresponds to the absence of trauma, Class 2 to a slight impact of the trauma, Class 3 to a significant impact, Class 4 to a strong impact, and Class 5 to a very strong impact. We hypothesized that a resilient subject would fall into Class 1, a recovered subject would start off in a higher class and then gradually move down to Class 1, and a non-resilient subject with a set of symptoms indicative of a PTSD type of disorganization would fall into Class 3, 4, or 5.
Anxiety was assessed using the validated French version of Spielberger et al.’s [41] State-Trait Anxiety Questionnaire. The total raw score on the STAY questionnaire was converted into a T-score that differentiated subjects with a normal level of trait and state anxiety (assumed to be the case of resilient subjects or ones having recovered) from subjects with a pathological level of anxiety, whose T-note indicated a high or very high degree of anxiety. The upper and lower limits of the anxiety scores were defined as follows: anxiety was considered very low if the T-score was less than or equal to 35, low if between 36 and 45, moderate if between 46 and 55, high if between 56 and 65, and very high if above 65. We hypothesized that a nonresilient subject with an anxious side to his/her disorganization would have a pathological state- and/or trait-anxiety score. Depressive disorders were assessed using the validated French version of the Beck Depression Inventory or BDI-II [42]. A T-score below 11 points is a very low number of depressive symptoms that falls within the normal range (resilient or recovered subjects should get such a score). A T-score between 12 and 19 corresponds to a slight degree of depression. Starting at a T-score between 20 and 27, we speak of major depression of moderate severity. A T-score between 28 and 63 characterizes subjects suffering from a severe, major depressive episode. We hypothesized that a non-resilient subject with a depressive side to his/her disorganization would get a score above 11 and most likely even above 19.
To measure the two intrapsychic factors chosen as determinants of a subject’s degree of psychological resilience, we used a projective test, the Rorschach, coded and interpreted in line with the Parisian School [43,44]. In the present article, we focus on two main indicators. The first measures the richness versus paucity of the imaginary space; the second measures the mentalization process, assessed in terms of the quality of the symbolization of contents related to sexual and aggressive drives.
The Rorschach test contains ten inkblots, which by definition are static. The subject is asked to imagine what the blots might represent. The most frequent type of response is based on the blot’s shape. Subjects with alexithymia — also called “operatory functioning” in psychoanalytic psychology — usually exhibit a severe deficit of the imaginary and are bogged down by concrete thoughts; this may lead to responses based solely on the inkblot’s shape and insensitivity to its other dimensions [45]. In contrast, a subject with a rich imaginary space will be capable, according to the Parisian school, of imprinting motion onto these static blots, and in doing so, of seeing moving contents, be they human beings or animals, objects, or things in nature. In this view, the richer the subject’s imaginary, the greater the total number of movement responses; and the more impoverished the subject’s imaginary, the lower the total number of movement responses. We thus hypothesized that resilient or recovered subjects would produce a much higher number of movement responses than non-resilient subjects would, insofar as imaginary functioning is the foremost mechanism permitting not only an attenuated impact of the initial trauma-induced shock, but also the ability to disengage from the intrusive reality undergone and fantasize a different one, thereby establishing short-term resilience.
To assess the possibility of long-term psychological resilience, the second intrapsychic factor we chose was the quality of the symbolization of contents related to sexual and aggressive drives, based on Cassiers’s [44] validated study on the risk of acting out. This author compared the symbolic elaborations of projected contents produced respectively by adult psychopathic subjects, adults presenting other types of mental pathologies, and healthy subjects. He showed that each of the tested personalities likely to become disorganized, with a risk of acting out, produced Rorschach test responses indicating altered symbolization of sexual/aggressive contents. In order for a subject to produce Rorschach responses that have a sexual or aggressive valence but are not crude (meaning that they are not close to the drive excitations that generated them) but well symbolized instead (meaning that the accompanying displeasure affects have been sufficiently elaborated and are far from the drive excitations that generated them), he/she must be able to distance him/herself from the drives implied in the projected Rorschach contents. This is done via the construction of a representation that is far-removed from the generating drive excitations and that potentially ends up including overdetermined and added meanings. Cassiers [44] distinguished four levels of increasing symbolization, ranging from the crudest (failure to symbolization: E and D responses) to the most elaborate (B and C responses); neutral responses void of a sexual or aggressive valence (such as banalities) are not coded. Below, we illustrate the coding process with an example for sexual-valence contents and an example for aggressive-valence contents.
Along the axis of sexual-valence contents, looking at the central black detail in the upper part of card 6, one could give a male-sex response that is crude, with no distancing from the drive excitation that generated it; this would be scored as poor symbolization, worth -2 points. A response of “organ” for the same part of the card remains relatively close to the drive excitation that generated it, but it is a little farther away (because “organ” does not necessarily mean sex organ and can refer to another part of the body) [44]. Sexual symbolization in this response remains deficient and would be scored D (worth -1 point). If the subject responds “stick”, for example, sexual symbolization is better and would be scored C (worth +1 point). This response is clearly farther away from the sexual drive excitation that generated it, since it can symbolize the male sex but is removed from the body and can have other meanings (i.e., a stick can be used to hit, be a tool to lean on, etc.). An even more complete level of sexual symbolization could be attained by a level B response (worth +2 points) such as “totem pole”, which is even farther from the body and depicts phallic power in a more highly symbolized way, all the while introducing a sacralized meaning not present in the preceding response.
Along the axis of responses referring to the aggressive dimension, we will now briefly illustrate Cassiers’s [44] four levels of symbolization, from the highest (B then C) to the lowest (D then E, the worst level), based on the same criteria of distance from the initial drive excitation. Consider the side blots in pink on card 8 of the test. The response “two pools of blood” would correspond to the crudest level of symbolization, the one closest to the initial excitation of the aggressive bodily drive; it would be scored E (worth -2 points). The response “two crushed cats” is farther from the initial aggressive bodily excitation but nevertheless translates a projection of it that remains crude; it would be scored D (worth -1 point). A response like “two fighting animals” translates a better mental elaboration of the initial aggressive drive excitation, with a charge of lesser intensity; it would be scored C (worth +1 point). The response “two tigers” would correspond to better symbolization of the aggressive drive excitation (level B, worth +2 points), with much more mental elaboration and a greater distance, afforded by the choice of animals symbolically known to be ferocious.
Cassiers [44] and other authors who have used his grid have obtained a high agreement rate among scorers [46,47]. Note that predetermined lists of how to code a large number of responses have been supplied by these authors to researchers interested in having an overall index of symbolic elaboration of aggressive and sexual drives. This index offers major advantages, including its correlation with the risk of aggressive self- or other acting out starting at a certain threshold, and also, at a more general level, with the risk of psychological behavior disorganization. It therefore seemed legitimate to choose this parameter as the central measure of mentalization, in view of establishing resilience or non-resilience among subjects having undergone a traumatic experience.
In theory, optimal symbolization should enable a subject to continuously produce symbolizations of sexual or aggressive contents at the most elaborated level, B, which would give a high symbolic elaboration index (SEI) of +2. In reality, no human subject can sustain such a high level throughout the test. At the other extreme, Cassiers [44], along with other authors who have worked with this grid, have shown that the symbolization capacity on the Rorschach breaks down among subjects who decompensate or act out, dropping in the worst of cases to a mean score of -2 when all test responses are very crude. Comparative studies have shown that, on a continuum ranging from -2 to +2 points, the cutoff point for identifying subjects at risk for behavioral decompensation is a mean SEI score below +0.5 points [44]. For the present study, then, we hypothesized that resilient subjects would maintain a score above 0.5 throughout the test, whereas initially non-resilient subjects in the process of recovering would reach this level at the time of recovery. As for non-resilient subjects, they should have a very problematic SEI score throughout the follow-up, a major sign of non-mentalization of the trauma.
Results
For each subject, we will begin with a table of six cortisol parameters derived from the salivary cortisol curves at the four assessment times during the follow-up period (Figure 1). We will compare these values to the normal ones and give the statistical significance levels in percentile distance to the mean (Table 1). Then in a second table, we will give each subject’s psychological resilience scores (Table 2).
| MEAN 50th percentile | 25th-75th percentiles (p ≤ 0.25) | 10th-90th percentiles (p ≤ 0.10) | Units | |
|---|---|---|---|---|
| AUC total AUC total/h | 14097 783 | 8949-22036 497-1224 | 5600-34990 311-1944 | ηg.h/l ηg/l |
| Peak % Decrease | 2990 69.6 | 1912-4599 68.0-69.5 | 1211-7079 67.2-69.6 | ηg/l % |
| CAR CAR/h | 2820 705 | 1636-4310 409-1077 | 1043-6659 261-1665 | ηg.h/l ηg/l |
| AUC ground AUC ground/h | 11296 628 | 7321-17750 407-986 | 4556-28377 253-1576 | ηg.h/l ηg/l |
| PM slope | -68.1 | -49.2 - -107.1 | -32.7 - -160.5 | ηg/l.h |
Calculated from CIRCORT data curves, R. Miller et al., 2016.
Table 1: Normal Cortisol Parameter Values and Percentiles.
| Months after TRAUMA | T1 | T2 | T3 | T4 | Units |
|---|---|---|---|---|---|
| 2 | 10 | 17 | 24 | ||
| AUC total AUC total/h | 16322 N NS 1070 x1.5 NS | 26440 x2 >p75 1511 x2 >p75 | 7728 /2 <p25 572 /1.5 NS | 9580 /1.5 NS 718 /N NS | ηg.h/l ηg/l |
| Peak % decrease | 5486 x2 >p75 78.8 N >p90 | 7421 x2.5 >p90 63.3 N- <p10 | 3990 x1.5 NS 87.4 x1.5 >p90 | 4687 x1.5 >p75 81.4 N+ >p90 | ηg/l % |
| CAR CAR/h | 2059 /1.5 NS 1373 x2 >p75 | 2411 N NS 1378 x2 >p75 | 3594 x1.5 NS 1797 x2.5>p90 | 2467 N NS 1346 x2 >p75 | ηg.h/l ηg/l |
| AUC ground AUC ground/h | 14263 x1.5 NS 935x1.5 NS | 24029 x2 >p75 1373 x2 >p75 | 4134 /2 <p10 306 /2 <p25 | 7113 /2 <p25 533 /1.5 NS | ηg.h/l ηg/l |
| PM slope | -68.5 N NS | -160.8 x2.5 >p90 | -37.8 /2 <p10 | -57.9 N- NS | ηg/h.l |
Table 2: Mister K's Biological Data.
Mister K’s biological and psychological data
Biological data: AUCtotal — rather, its AUCground component — was initially high at T1, continued to be high at T2, and then returned to a completely normal value at T3 and T4. The CAR area stayed normal throughout the follow-up, probably linked to the good resilience exhibited by this subject from the start. More specifically, the CAR rise in the morning took place in less time for this patient, as evidenced by its high peak and CAR/h for a normal CAR. These two parameters changed little and remained at twice the normal value throughout the two-year follow-up. The slope aligned accordingly after a rise at T1 and especially at T2, where AUCground increased notably, became normal, and then fell to a low level at T3 and T4. This is in line with the return of AUCground to values in the lower part of the normal range: the HPA axis is back to a basal level by T3, keeping a normal, unchanged CAR from the beginning, and decreasing the AUCground part.
Psychological data: Mister K’s Psychological Data (Table 3). Mister K’s scores on the three questionnaires indicate psychological resilience right from T1 (normally low anxiety scores on the STAY anxiety scale and on the BDI-II depression questionnaire that remained so throughout the follow-up period). The impact of the trauma on psychotraumatic sequels was low at T1 (score of 2 on the Traumaq questionnaire), disappeared altogether by T2, and stayed so until T4, thereby allowing him to fall into Class 1. We also see a total lack of depression already at T1 and all the way through to T4.
| T1 | T2 | T3 | T4 | |
|---|---|---|---|---|
| Months | 2 | 10 | 17 | 24 |
| STAY E | 40 | 39 | 41 | 39 |
| STAY T | 32 | 37 | 31 | 31 |
| T | 2 | 1 | 1 | 1 |
| BDI-II | 2 | 0 | 1 | 0 |
| SUM M | 2 | 2 | 2 | 4 |
| Symbolization (SEI) | +0.8 | +1.3 | +1.3 | +1.4 |
Analysis of Mister K's Psychological Resilience Indicators at the Four Follow-up Times
Table 3: Mister K's psychological data.
If we look simultaneously at Mister K’s biological and psychological indicators, we can see that psychological resilience in his case slightly preceded neurobiological modifications, since his cortisol levels only become normal between T2 and T3 whereas psychological resilience was fully confirmed at T2. His Rorschach indicators were satisfactory, with a spared SEI by T2 signaling the subject’s good symbolic elaboration capacity.
Note also that imaginary functioning was present in Mister K (two movement responses on the Rorschach between T1 and T3), and although still inhibited at T4, it was more developed (four movement responses). Symbolization quality, as assessed by SEI, appears to be an essential intrapsychic factor for the mental elaboration of trauma. Indeed, Mister K, who presented slight psychotraumatic sequels on the Traumaq at T2 (with a total score placing him in Class 2) saw his symbolization ability maintained on the Rorschach (mean SEI of +0.8) at T1, which is above the cutoff point for the absence of mental disorganization. The mental elaboration of psychotraumatic sequels was complete at T2 (Class 1), with no problematic trait or state anxiety and no depressive symptoms throughout the follow-up. In parallel, we find a mean symbolization index on the Rorschach indicating good symbolization that stayed so between T2 and T4, going from +0.8 at T1, to +1.3 at T2 and T3, and to +1.4 at T4.
Clinically speaking, Mister K displayed quite remarkable resistance to the traumatic intrusion already by T1, which was sustained until two years post-accident (T4). We can see that this man has a great ability to share his emotions and inner feelings. Regarding his current social and professional adaptation, Mister K heads a firm that he started up himself. He is highly engaged in his work, which he resumed, and is obviously proud of what he does.
Mister B’s biological and psychological data
Mister B’s biological data: Mister B exhibited highly abnormal cortisol levels at study inclusion (T1) (Table 4). His AUCtotal was elevated and then dropped dramatically at T2, with a strong decrease in its daytime component AUCground, which stayed very low, i.e., at a third or half of the normal level for the first three follow-up times. Therefore the much higher percent of decrease than normal and a flattened daytime slope seen at all three of these measurement times. This seems to be related to the patient’s very high state of anxiety at T1. His CAR remained markedly below the normal by a factor of 2 to 5 from T1 to T3, which is a sign of initial exhaustion of the HPA axis. The complete return to normal at T4 of CAR, daytime slope, and AUCtotal, which rose slowly, is indicative of a notable biological improvement that had started by T3, in parallel with the subject’s favorable psychological evolution already on the way at T2.
| Months after TRAUMA | T1 | T2 | T3 | T4 | Units |
|---|---|---|---|---|---|
| 2 | 10 | 17 | 24 | ||
| AUC total AUC total/h | 15238 N NS 1069 x1.5 NS | 4864 /3 <p10 290 /3 <p10 | 7405 /2 <p25 529 /1.5 NS | 9269 /1.5 NS 618 /N- NS | ηg.h/l ηg/l |
| Peak % decrease | 5124 x1.5 >p75 50.2 /1.5 <p10 | 2774 N NS 86.6 N+ >p90 | 2142 /1.5 NS 63.1 N- <p10 | 3080 N NS 75.5 N >p90 | ηg/l % |
| CAR CAR/h | 1063 /2 <p25 1063 x1.5 NS | 1245 /2 <p25 1245 x2 >p75 | 618 /5 <p10 309 /2.5 <p25 | 2592 N- NS 1244 x2 >p75 | ηg.h/l ηg/l |
| AUC ground AUC ground/h | 14175 x1.5 NS 995 x1.5 >p75 | 3619 /3 <p10 216 /3 <p10 | 6787 /2 <p25 485 /1.5 NS | 6677 /2 <p25 445 /2 NS | ηg.h/l ηg/l |
| PM slope | -195.9 x3 >p90 | -13.0 /5 <p10 | -60.1 N- NS | -54.9 /1.5 NS | ηg/h.l |
Mister B's Salivary Cortisol Parameters (left in cells) at the Four Follow-up Times and comparisons to normal values (ratios given right in the cells, before percentiles probability)
Table 4: Mister B's biological data.
Mister B’s psychological data: Looking at the scores obtained on the three scales — anxiety, post-traumatic sequels, and depression — we can see a much greater impact of the trauma at T1 for Mister B than for Mister K, which was paralleled by his more abnormal cortisol levels than Mister K’s (Table 5). Again, unlike Mister K, Mister B’s anxiety on the STAY scale (representing his state at the time) reached a high pathological level (score of 53) and his trait anxiety was even higher (score of 59). The same held true for post-traumatic sequels on the Traumaq questionnaire, where he fell into Class 3 and stayed there throughout the follow-up period. He described sleep disturbances, difficulty concentrating, and feelings of violent hatred, among other things. Clearly, Mister B was unable to engage in a resilient process at T1, when his anxiety scores were very high. He manifested slight depressive symptoms on the BDI-II at every evaluation time (T1 to T4), although his depression scores did decrease and become normal between T3 and T4 (BDI-II score dropping from 15 to 6). State anxiety and depressive disturbances decreased by T2, persisted between T1 and T3, and were finally elaborated at T4, when the only remaining problem was moderate post-traumatic sequels, which were stable from T1 to T4. For Mister B, then, it seems legitimate to speak of recovery — albeit not total even 24 months after the accident — and to advance that psychological recovery mainly took place between T3 and T4, in parallel with biological recovery.
| T1 | T2 | T3 | T4 | |
|---|---|---|---|---|
| Months | 2 | 10 | 17 | 24 |
| STAY E | 53 | 42 | 42 | 42 |
| STAY T | 59 | 52 | 52 | 52 |
| T | 3 | 3 | 3 | 3 |
| BDI-II | 11 | 14 | 15 | 6 |
| SUM M | 5 | 2 | 8 | 5 |
| Symbolization (SEI) | +0.3 | +1.4 | +1.8 | +1.5 |
Table 5: Mister B's psychological data.
Regarding the intrapsychic factors enabling trauma elaboration, it is interesting to note that Mister B’s biological and psychological markers had a clearly greater impact at T1 than for Mister K. This forced Mister B to mobilize his imaginary space in a much more defensive way to cope with this intrusive reality: the total number of movement responses on the Rorschach test was much higher at T1 than for Mister K, and was to remain so (except at T2). His mentalization, assessed in terms of symbolization quality (mean SEI of +0.3), was more deficient at T1 than Mister K’s, due to the accident’s greater traumatic impact for Mister B, but it was largely recovered by T2 (SEI of +1.4). So our initial conjecture, which granted mentalization a critical role in psychological recovery, was confirmed here throughout the follow-up, thus allowing Mister B’s recovery, even if not yet complete.
Clinically speaking, the impossibility for Mister B to resume his former occupation after the accident lowered his self-esteem, so he had to work much harder on accepting this fact. By T4, recovery was manifest, which for this subject also, translated into plans to change occupations and to attend professional training courses in his new field.
Mister M’s biological and psychological data
Mister M’s biological data: The AUCtotal more than doubled during the follow-up, with a concomitant twofold increase in CAR, whose peak height rose by T2 (Table 6). This follows from the fact that his depressive symptoms got much worse at T2 and stayed so until T4. However, the CAR was hidden by an increasingly elevated AUCground already in the morning, the percent of decrease remained so significantly low. The daytime slope ended up gradually rising just as much, especially at T3 and T4. Over the two-year follow-up period, this patient had abnormally high cortisol levels that got worse over time and accompanied both his psychological deterioration and the impact of the non-elaborated trauma.
| Months after TRAUMA M | T1 | T2 | T3 | T4 | Units |
|---|---|---|---|---|---|
| 2 | 10 | 17 | 24 | ||
| AUC total AUC total/h | 12238 N- NS 731 N- NS | 12563 N- NS 897 N NS | 20164 x1.5 NS 1415 x2 >p75 | 26691 x2 >p75 1540 x2 >p75 | ηg.h/l ηg/l |
| Peak % decrease | 3013 N- NS 51.6 /1.5 <p10 | 5308 x2 >p75 80.0 N >p90 | 3896 x1.5 NS 54.0 /1.5 <p10 | 5025 x1.5 >p75 50.1 /1.5 <p10 | ηg/l % |
| CAR CAR/h | 884 /3 <p10 663 N- NS | 3425 N+ NS 1713 x2.5 >p90 | 2047 /1.5 NS 1365 x2 >p75 | 3811 x1.5 NS 1270 x2 >p75 | ηg.h/l ηg/l |
| AUC ground AUC ground/h | 11353 N 678 N NS | 9137 N- NS 653 N NS | 18117 x1.5 >p75 1271 x2 >p75 | 22880 x2 >p75 1320 x2 >p75 | ηg.h/l ηg/l |
| PM slope | -94.2 x1.5 NS | -69.9 N NS | -125.0 x2 >p75 | -174.8 x2.5 >p90 | ηg/h.l |
Table 6: Mister M's biological data
Mister M’s psychological data: Mister M exhibited a lack of psychological resilience that was already manifested at T1, where he presented several disabling symptoms that increased throughout the follow-up period (Table 7). However, his post-traumatic sequels, assessed using the Traumaq scale, were relatively weak and stable over time (Class 2 from T1 to T4). In contrast — unlike Mister K, the resilient subject who exhibited no anxiety, no post-traumatic sequels, and no depression from T1 to T4, and unlike Mister B, the recovered subject who saw his high levels of state and trait anxiety at T1 on the STAY scale drop down to normal on the following stages, and whose depressive symptoms assessed on the BDI-II decreased over time, reflecting high quality mental elaboration — the time courses of Mister M’s anxiety and depression scores followed inverse curves. Trait anxiety was maintained at a high, pathological level from T1 to T4; state anxiety, directly linked to the experienced trauma, rose between T1 and T4 and became pathological. The same curve was observed for his depressive symptoms, which were slight at T1, became severe and very pathological at T2 and T3, and were still high at T4. We can see here that Mister M’s psychological markers (indicative of nonresilience) moved in parallel with his neurobiological markers.
| T1 | T2 | T3 | T4 | |
|---|---|---|---|---|
| Months | 2 | 10 | 17 | 24 |
| STAY E | 40 | 45 | 55 | 54 |
| STAY T | 59 | 59 | 59 | 55 |
| T | 2 | 2 | 2 | 2 |
| BDI-II | 9 | 27 | 27 | 25 |
| SUM M | 1 | 2 | 2 | 1 |
| Symbolization (SEI) | -0.1 | -0.5 | -1.1 | 0.0 |
Analysis of Mister M's Psychological Resilience Indicators at the Four Follow-up Times
Table 7: Mister M’s psychological data.
Mister M’s failure to mentally elaborate the trauma at the psychological level was confirmed by both of the intrapsychic parameters we chose. Unlike the resilient subject — whose imaginary space increased at T4 and who, already at T1, possessed a good symbolization capacity (SEI of +0.8 that improved after that) — Mister M’s imaginary space was equally small at T1 and T4 (only one movement response on the Rorschach), and his symbolization capacity remained very deficient between T1 and T4 (negative SEI throughout). In contrast, the subject who recovered at both the biological and psychological levels, Mister B, had a very rich imaginary space upon which he relied heavily at T1, T3, and T4 and which made him much more able to get rid of the intrusive realities he had undergone. Although Mister B’s symbolization capacity was deficient at T1 (SEI of +0.3), albeit to a lesser extent than Mister M’s (SEI of -0.1), it rapidly began to increase between T2 to T4, whereas Mister M’s remained completely deficient all the way through the follow-up period.
Clinically, Mister M displayed a core of strong guilt and anxiety about the future. This contributed to accentuating his depressive symptoms and justified a proposal of therapy.
Conclusion
In a recent article published in Nature, King [18] stressed that resilience, defined as the ability to withstand severe stress, is a key concept in current research. Here, we present a new and original qualitative method for evaluating resilience. We used this longitudinal method in a two-year follow-up of three subjects confronted with the risk of death, who presented either resilience to the trauma, a time course leading to psychopathology, or recovery after a phase of psychopathological upheaval. To our knowledge, this preliminary study is the first to compare and relate neurobiological resilience, assessed using not one but several indicators of diurnal cortisol, to psychological resilience, assessed doubly by the absence of symptomatic perturbations and by the two intrapsychic factors that underlie our theoretical psychodynamic model: the quality of the imaginary space, and mentalization as measured by the subject’s symbolization capacity after the traumatic event. This approach seems to be the only one capable of addressing the interconnections between the neurobiological sphere and the psychological sphere.
A comparative analysis of how the data from these two spheres evolved over the follow-up period suggested that for the resilient subject and for the recovered subject studied here, psychological resilience preceded neurobiological resilience. In the non-resilient subject after the breakdown, the two spheres evolved in the same direction from the beginning. In the resilient and restored subjects, the quality of the imaginary space, via its defensive and protective function, appeared to be a fundamental factor for coping with the trauma . This factor induced a return back to normal of the AUCground in the diurnal cortisol. It seems that trauma cannot be elaborated unless the symbolization capacity takes over, either at the onset as in our resilient subject, or later as in our recovered subject. In the non-resilient subject, these two essential factors of intrapsychic functioning remained deficient, even in the long run. These psychological findings for adults align with the clinical results of other comparative, qualitative studies of resilient and non-resilient children subjected to the risk of death [48].
The present study also pointed out the merits of studying multiple parameters of diurnal cortisol in view of accounting for neurobiological resilience or non-resilience to trauma. For the three subjects compared here, the cortisol awakening response (CAR) supplied interesting information but the area under the curve also furnished some indicators that helped further differentiate the subjects. CAR and basal cortisol level, more specifically AUCground, can be assessed independently, and a modification of one of these parameters is not necessarily linked to a variation in the other. CAR seems to be very sensitive to the patient’s psychological deterioration and depression. And it can evolve independently of AUCground. This last parameter seems to be related more specifically to the patient’s state of anxiety (see Mister B). In any case, for Misters K and B, positive psychological improvement took place before neurobiological normalization.
We are fully aware of the limitations and biases inherent in our qualitative exploratory approach. The most important one concerns the small number and single gender of the subjects studied. The second has to do with the fact that, despite considerable effort to control a large number of variables likely to interfere with a subject’s cortisol levels, we did not fully abide by Stalder et al.’s [49] expert consensus guidelines, which recommend sampling cortisol levels several days in a row in order to average the values obtained and ensure their consistency. This point is certainly applicable to experimental studies in a laboratory, but it does not seem feasible for repeated follow-up of subjects in their everyday lives over a period as long as 24 months, given that the duration of re-hospitalization must be reduced to a minimum.
We would like to remind our readers that the main objective of this study was to offer to the many clinicians and researchers working in this field a new methodological model for use in quantitative clinical research, one that would allow for generalization of the tentative conclusions drawn here with three subjects. This option may turn out to difficult to implement for several reasons. Firstly, in using the neurobiology/psychology interface outlined here, it is important to compare groups of subjects who are resilient-recovered or nonresilient over a potentially longer period than ours, to better ensure the stability of the subjects’ clinical-psychological and neurobiological status. It nevertheless seems very difficult to simultaneously control the entire set of factors that might alter cortisol levels, in a uniform way for all subjects in their everyday life situations (as we did here). Some of the important parameters pointed out recently by Elder et al. [50] likely to considerably modify the stability of the cortisol awakening response are the type of exposure to light, strict observance of awakening time, number of hours of sleep, and number of times the subject wakes up during the night. Controlling all of these parameters, indispensable for ensuring within- and between-group homogeneity, is a tremendous challenge for quantitative studies. On the other hand, one could also contend that if these biological parameters change on the very day of the six-month sampling, even though the person’s life itself is not notably different — which in effect is what we are assessing — then it is precisely because the subject’s state itself has enabled or induced those changes.
References
- Lighezzolo J, De Tychey C (2004) La résilience; se (re)construire après le traumatisme. Resilience: Self-Reconstruction after Trauma, Paris.
- Cyrulnik B, Duval P (2006) Psychanalyse et résilience. Psychoanalysis and Resilience, Odile Jacob, Paris.
- O’Brien KM, Tronick E, Moore CL (2013) Relationship between Hair Cortisol and Perceived Chronic Stress in a Diverse Sample. Stress Health 29: 337-344.
- Herane A, de Angel V, Papadopoulos A, Strawbridge B, Wise T, et al. (2015) The relationship between cortisol, stress and psychiatric illness: New insights using hair analysis. J Psychiatr Res 70: 38-49.
- Walker FR, Pfingst K, Carnevali L, Sgoifo A, Nalivaiko E (2017) In the search for integrative biomarker of resilience to psychological stress. Neurosci Biobehav Rev 74: 310-320.
- Dantzer R, Kalin N.H (2015) The cortisol awakening response at its best. Psychoneuroendocrinology 63: 412-413,
- Yehuda R, McFarlane A, Shalev A (1998) Predicting the Development of Posttraumatic Stress Disorder from the Acute Response to a Traumatic Event. Biol Psychiatry 44: 1305-1313.
- Delahanty DL, Raimonde AJ, Spoonster E (2000) Initial Posttraumatic Urinary Cortisol Levels Predict Subsequent PTSD Symptoms in Motor Vehicle Accident Victims. Biol Psychiatry. 48: 940-947.
- Wessa M, Rohleder N, Kirschbaum C, Flor H (2006) Altered cortisol awakening response in posttraumatic stress disorder. Psychoneuroendocrinology 31: 209-215.
- Wahbeh H, Oken B (2013) Salivary Cortisol Lower in Posttraumatic Stress Disorder. J Trauma Stress 26: 241-248.
- Keeshin BR, Strawn JR, Out D, Granger DA, Putnam FW (2014) Cortisol awakening response in adolescents with acute sexual abuse related post-traumatic stress disorder. Depress Anxiety 31:107-114.
- Van Santen A, Vreeburg SA, Van der Does AW, Spinhoven P, Zitman FG, et al. (2011) Psychological traits and the cortisol awakening response: Results from the Netherlands Study of Depression and Anxiety. Psychoneuroendocrinology 36: 240- 248.
- Morris MC, Rao, U (2014) Cortisol response to psychosocial stress during a depressive episode and remission. Stress 17: 51-58.
- Mantella RC, Butters MA, Amico JA, Mazumdar S, Rollman BL, et al.(2008) Salivary cortisol is associated with diagnosis and severity of late-life generalized anxiety disorder. Psychoneuroendocrinology 33: 773-781.
- Binder EB, Holsboer F (2012) Low Cortisol and Risk and Resilience to Stress-Related Psychiatric Disorders. Biol Psychiatry 71: 282-283.
- Ruiz-Robledillo N, De Andres-Garcıa S, Perez-Blasco J, Gonzalez-Bono E, Moya-Albiol L (2014) Highly resilient coping entails better perceived health, high social support and low morning cortisol levels in parents of children with autism spectrum disorder. Res Dev Disabil 35: 686-695.
- Galatzer-Levy I, Steenkamp M, Brown A, Qian M, Inslicht S, et al. (2014) Cortisol response to an experimental stress paradigm prospectively predicts long-term distress and resilience trajectories in response to active police service. J Psychiatr Res 56: 36-42.
- King A (2016) Rise of resilience. Nature 531: S18-S19.
- Meggs J, Golby J, Mallett CJ, Gucciardi DF, Polman RC (2015) The Cortisol Awakening Response and Resilience in Elite Swimmers. Int J Sports Med 37: 169-174.
- Bustany P, Laurent M, Cyrulnik B, De Tychey C (2015) The Neurobiological Determinants of Resilience. Viol Resil 18-55.
- Mizuno Y, Hofer A, Suzuk T, Frajo-Apor B, Wartelsteiner F, et al.(2016) Clinical and biological correlates of resilience in patients with schizophrenia and bipolar disorder: A cross-sectional study. Schizophr Res 175: 148-153.
- Widlöcher D (1990) Le cas au singulier. Nouvelle Revue de Psychanalyse 42: 282-302.
- Widlöcher D (1999) La méthode du cas. Monographies de Psychopathologie 1: 191-200.
- Patterson JM (1995) Promoting resilience in families experiencing stress. Pediatr Clin North Am 42: 47-63.
- Bergeret J (1972) Abrégé de psychologie pathologique [Short Guide to Pathological Psychology]. Masson, Paris.
- Tychey C, Diwo R, Dollander M (2000) Mentalization: Theoretical and Clinical Projective Approach Using the Rorschach Test. Bulletin de Psychologie 448 :469–480.
- Trousselard M, Steiler D, Raphel C, Cian C, Duymedjian R, et al. (2010) Validation of a French version of the Freiburg Mindfulness Inventory - short version: relationships between mindfulness and stress in an adult population. BioPsychoSocial Medicine 4 :1–11.
- Daubenmier J, Hayden D, Chang V, Epel E (2014) It’s not what you think, it’s how you relate to it: Dispositional mindfulness moderates the relationship between psychological distress and the cortisol awakening response. Psychoneuroendocrinology 48:11–18.
- Brown KW, Ryan RM (2003) The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol 84: 822–848.
- Walach H, Buchheld N, Buttenmüller V, Kleinknecht N, Schmidt S (2006) Measuring mindfulness - the Freiburg Mindfulness Inventory (FMI). Personality and Individual Differences 40:1543-1555.
- Baer RA, Smith GT, Allen KB (2004) Assessment of mindfulness by self-report: the Kentucky Inventory of mindfulness Skills. Assessment 11: 191–206.
- Kross E, Davidson M, Weber J, Ochsner K (2009) Coping with emotions past: the neural bases of regulating affect associated with negative autobiographical memories. Biol Psychiatry 65: 361–366.
- Taylor VA, Grant J, Daneault V, Scavone G, Breton E , et al. (2011) Impact of mindfulness on the neural responses to emotional pictures in experienced and beginner meditators. Neuroimage 57: 1524–1533.
- Way BM, Creswell JD, Eisenberger NI, Lieberman M (2010) Dispositional mindfulness and depressive symptomatology: correlations with limbic and self-referential neural activity during rest. Emotion 10: 12–24.
- Taren AA, Creswell JD, Gianaros PJ (2013) Dispositional mindfulness co-varies with smaller amygdala and caudate volumes in community adults. PLoS ONE 8: e64574.
- Dekel S, Einâ€ÂDor T, Gordon KM, Rosen JB, Bonanno G.A (2013) Cortisol and PTSD Symptoms Among Male and Female Highâ€ÂExposure 9/11 Survivors. Journal of Traumatic Stress 26: 621-625.
- Duan H, Yuan Y, Zhang L, Qin S, Zhang K, et al. (2013) Chronic stress exposure decreases the cortisol awakening response in healthy young men. Stress 16: 630–637.
- Charney D (2004) Psychobiological mechanisms of resilience and vulnerability: Implications for successful adaptation to extreme stress. Am J Psychiatry 161: 195–216.
- Miller R, Stalder T, Jarczok M, Almeida DM, Badrick E, et al. (2016) The CIRCORT database: Reference ranges and seasonal changes in diurnal salivary cortisol derived from a meta-dataset comprised of 15 field studies. Psychoneuroendocrinology 73:16–23.
- Damiani C, Pereira-Fradin MP (2006) Traumaq: A Trauma Assessment Questionnaire. Les Éditions du Centre de Psychologie Appliquée, Paris.
- Spielberger C, Gorsuch RL, Lushene RE, (1997) STAY: the State-Trait Anxiety Scale. ECPA, Paris.
- Beck AT, Steer RA, Brown GK (1998) Beck Depression Inventory (BDI-II) (ECPA), Paris.
- Rausch de Traubenberg, N (1990) Practical Guide to Using the Rorschach. P.U.F, Paris.
- Cassiers L (1968) The Delinquent Psychopath. Charles Dessart, Bruxelles.
- Tychey C, Garnier S, Lighezzolo J, Claudon P, Rebourg –Roesler, C (2010) An accumulation of negative life events and the construction of alexithymia: a longitudinal and clinical approach J Pers Assess 92:189–206.
- Burnel F, Helleringer M, Heidel A, Kahn M, De Tychey C (1991) Symbolic Elaboration Capacity and Manifest Aggressiveness: Comparative Approach Using the Rorschach Test with 8- to 12-Year-Old Children. Neuropsychiatrie de l’enfance et de l’adolescence 39 : 99–104.
- Tychey C, Cahen T, Sagnes L (1991) Depression and Suicide Risk: Comparative Approach Using the Rorschach Test. Revue Européenne de Psychologie Appliquée 41 : 181–188.
- Tychey C, Lighezzolo J, Claudon, P, Garnier S, Demogeot N (2012) Resilience, Mentalization, developmental tutor: a psychoanalytic and projective approach. Rorschachiana 33: 49–77.
- Stalder T, Kirschbaum C, Kudielka BM, Adam EK, Pruessner JC, et al. (2016) Assessment of the cortisol awakening response: Expert consensus guidelines. Psychoneuroendocrinology 63:414–432.
- Elder GJ, Ellis JG, Barclay NL, Wetherell MA (2016) Assessing the daily stability of the cortisol awakening response in a controlled environment. BMC Psychology 4:3.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi