Case Report, J Pulm Med Vol: 5 Issue: 1
Sarcomatoid Carcinoma in a Filipino Patient: Case Report and Review of Literature
Catherine Jordan*, Steffanie Charlyne Tamayo, Raiza Marave, Rex Santiago, Ma. Janeth Samson, Agnes Gorospe
Institute of Pulmonary Medicine, St. Luke’s Medical Center, Manila, Philippines
*Corresponding Author: Catherine EJ, Institute of Pulmonary Medicine, St. Luke’s Medical Center, Manila, Philippines, Tel: +639175172764; E-Mail: ceeejordan@yahoo.com
Received Date: 14 November, 2020; Accepted Date: 28 November, 2020; Published Date: 05 December, 2020
Citation: C Jordan , SC Tamayo , RMarave, MJ Samson, A Gorospe, et al. (2021) Sarcomatoid Carcinoma in a Filipino Patient: Case Report and Review of Literature. J Pulm Med 5:1
Abstract
We report a case of an 82-year old Filipino male who initially presented with chronic cough, weight loss, and hemoptysis. Work-ups lead to a diagnosis of metastatic non-small cell carcinoma, favoring adenocarcinoma, in a subcarinal lymph node that was compatible with a pulmonary primary. There was persistence of symptoms and severe atelectasis, which prompted clinicians to perform rigid and repeat flexible bronchoscopy with Holmium laser ablation to debulk the endobronchial mass. Our patient had a non-small cell carcinoma with pleomorphic features stage IV (cT4 N0 M1c) with bone, brain and pleural metastases. Biomarker testing did not show EGFR mutation, ALK was negative and PDL-1 immunohistochemistry showed tumor proportion score of 20-30%. He received one cycle of Pemetrexed therapy. However, he expired on the 39th hospital day due to acute right cerebellar and left parieto-occipital hemorrhage. The recognition of this rare histologic subtype is important because of its generally aggressive nature and limited treatment options.
Keywords: Lung cancer; Non-small cell carcinoma; Sarcomatoid carcinoma; Pleomorphic carcinoma
Introduction
Lung cancer is the most commonly diagnosed cancer (11.6% of the total cases) and the leading cause of cancer death (18.4% of the total cancer deaths) in both sexes combined worldwide according to the Global cancer statistics 2018 [1]. Lung cancers are very heterogenous histopathologic entities, with adenocarcinoma comprising the most common histologic subtype [2]. However, rarer subtypes may be encountered during routine clinical practice and the recognition of these variants is important due to their unique clinical, radiologic, and pathologic features. Herein we present the case of an 82-year old male with a lung mass who had a subcarinal lymph node biopsy, which showed metastatic pulmonary adenocarcinoma. Subsequent biopsy of the lung mass showed features compatible with pleomorphic carcinoma.
Case Report
We report the case of an 82-year old Filipino male who presented with a two and a half-month history of non-productive cough, accompanied by unquantified weight loss and hemoptysis. He had a 30 pack-year smoking history. There is no known family history of malignancy. He was previously treated with antibiotics and anti-tuberculosis medications at a local hospital; however, persistence of symptoms and subsequent development of shortness of breath in association with paroxysms of cough prompted consult at our institution.
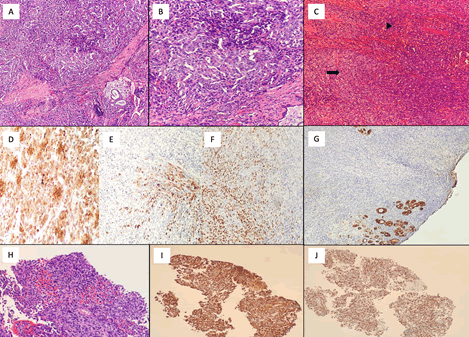
High Resolution Computed Tomography of the chest showed an 8.9 x 11 x 10 cm ill-defined heterogenous mass on the left hilar area and enlarged lymph nodes. The patient underwent fiberoptic bronchoscopy with biopsy and endobronchial ultrasound-guided transbronchial needle aspiration (EBUS TBNA), wherein tissue samples from the left upper lung mass and subcarinal lymph node were sent for histopathology. Microscopic sections showed polygonal cells in loose to cohesive clusters and scattered singly. These had round to ovoid, hyperchromatic, moderately to highly pleomorphic nuclei, occasional prominent nucleoli, irregular nuclear membranes, and ample, eosinophilic cytoplasm. Mitotic Figures 1 and 2 and focal areas of necrosis were appreciated. Immunohistochemical stains showed that these cells were diffusely positive for CK and TTF-1, and negative for Napsin A and p40. The findings were compatible with a poorly-differentiated adenocarcinoma.
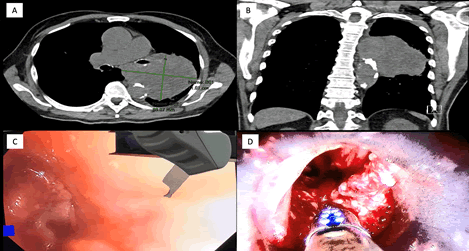
Figure 1: (A) Coronal and (B) sagittal sections from the High resolution CT-scan shows a large ill-defined mass extending into the subcarinal region and partially encasing the aortic arch as well as the left bronchial tree; (C) Bronchoscopy shows an endobronchial tumor completely obstructing the distal third of left main bronchus causing severe atelectasis; (D) Debulking of the endobronchial tumor using Holmium Laser ablation.
Figure 2: (A) and (B) Microsections of the endobronchial tumor biopsy shows a biphasic population of cells. The epithelioid component is composed of cells with round to ovoid, vesicular to hyperchromatic nuclei and ample, eosinophilic cytoplasm, whereas the mesenchymal component is composed of round to spindle cells with ovoid, hyperchromatic nuclei, inconspicuous nucleoli, and indistinct cytoplasm. (C) In most of the tumor, the epithelioid areas (arrow) are intimately associated with the spindle cells (arrowhead). (D) By immunohistochemistry, the tumor is positive for CAM 5.2. (E) CK and (F) TTF-1 shows patchy positive expression, predominantly in the epithelioid-looking areas. (G) Cytokeratin is mostly negative in the sheets of round to spindle cells. (H) The metastatic tumor in the subcarinal (station 7) lymph node is predominantly epithelioid in morphology without an obvious or readily identifiable spindle cell component. It shows diffuse positivity for CK (I) and TTF-1 (J).
During the course of his hospital stay, the patient developed atelectasis of left lung for which he underwent rigid and flexible bronchoscopy with Holmium laser ablation of endobronchial mass. It was noted that an endobronchial tumor was completely obstructing the distal third of the left mainstem bronchus. There was more tissue available for histologic examination with this procedure and it was noted that apart from the epithelioid component seen in the previous biopsy, there were also areas that demonstrated solid sheets of round to spindle cells. The spindle cells were mostly negative for CK and TTF-1 on immunohistochemistry. Other immunohistochemical stains such as Napsin A, p40, chromogranin, synaptophysin, CD56, and NKX3.[1] were negative. As such, the presence of a dual population of epithelioid/polygonal cells and spindle cells on both morphology and immunohistochemistry is compatible with a primary pulmonary pleomorphic carcinoma.
Our patient has a non-small cell carcinoma with pleomorphic features stage IVB (cT4 N2 M1c) with bone, brain and pleural metastases. As per WHO recommendations, the specimen was sent for biomarker testing. No EGFR mutations were detected while ALK was negative by immunohistochemistry. PD-L1 immunohistochemistry showed a tumor proportion score of 20%-30%. Thus, the patient received 1 cycle of Pemetrexed (500 mg/m2) chemotherapy and was supposed to receive targeted immunotherapy. However, on the 39th hospital day, he complained of diffused headache with a VAS score of 8/10 (0=no pain, 10=worst pain) with associated non-projectile vomiting episode. Plain cranial computed tomography was done which showed right cerebellar and left parieto-occipital hemorrhage. He was transferred to neurology critical care unit and eventually developed bradycardia and subsequent cardiopulmonary arrest.
Discussion
Pulmonary pleomorphic carcinoma (PPC) remains a rare histopathologic type of pulmonary malignancy, comprising less than one percent of cases 2. It is grouped under sarcomatoid carcinomas of the lung, along with carcinosarcoma and pulmonary blastoma[2]. They are composed of a non-small cell carcinoma component (adenocarcinoma, squamous cell carcinoma, or undifferentiated non-small cell carcinoma) with at least 10% spindle and/or giant cells [2]. The epidemiology of these tumors is similar to other non-small cell carcinomas, being that they are commonly found in smokers.
The epithelioid component in pleomorphic carcinoma, as seen in this case, most commonly shows adenocarcinoma [2]. The non-epithelial component on the other hand, most commonly shows spindle cells that resemble fibroblasts or myofibroblasts [3]. Because of the heterogeneity in the morphology and distribution of these components, the diagnosis of these lesions, particularly on small biopsies, can be challenging. As seen in this case, the initial biopsy of the lung mass and the subcarinal lymph node only showed the epithelial component; the spindle cell areas were identified in the larger tissues submitted after Holmium laser ablation.
In general, molecular testing is geared towards the expected genetic abnormality associated with the differentiated component, such as EGFR mutations and ALK rearrangements for tumors with areas showing an adenocarcinoma [2]. In this case, in spite of the presence of an adenocarcinoma component, no EGFR mutations or ALK rearrangement was identified. The absence of these mutations does not automatically exclude the patient from receiving targeted therapy however, as more recent studies show a high association of MET exon 14 skipping mutations with tumors with sarcomatoid histologies [4,5]. This then highlights the importance of identifying the spindle cell component of sarcomatoid carcinomas even on small biopsies, especially in the setting of a developing country wherein comprehensive genomic profiling is not routinely performed on every tumor. In such cases, a more extensive biomarker panel may be suggested. Although further biomarker testing was recommended in our patient, he expired before his specimen could be sent for additional tests.
Sarcomatoid carcinomas have also been found to have higher expression of PD-L1 compared to other NSCLC6. In concordance with this, the tumor in this case had a PD-L1 expression of 20-30%, making the patient eligible for immunotherapy. Unfortunately, though chemotherapy with Pemetrexed was started for this patient, he expired after 39 days due to brain herniation syndrome secondary to acute tumor bleed on the Left parieto-occipital and right cerebellar areas.
Most clinical trials on lung cancer are concentrated on adenocarcinoma or squamous cell carcinoma; however, pathological sub-classifications are becoming increasingly important for treatment decisions. Cytotoxic agents used for the treatment of NSCLCs are the same as those used for sarcomatoid carcinomas. Overall, pulmonary sarcomatoid carcinoma was found to be resistant to conventional chemotherapy [6] and was associated with non-respondence to palliative chemotherapy [7]. Therapies targeting the PD-1/PD-L1 pathway are an emerging treatment for lung cancer. PD-L1 expression was higher in PSC than in NSCL[6]. The study Vieira et. al showed that the presence of tumor-infiltrating lymphocytes as a marker of a preexisting immune response with an associated positive PD-L1 expression, is currently the best known predictive factor of efficacy of these therapies [8]. This result provided a basis for the potential use of immunotherapy targeting immune checkpoints such as PD-1/PD-L1 inhibitors for this otherwise difficult to treat disease [9,10,11].
Conclusion
We have presented a case of an 82-year old male smoker with lung cancer that demonstrated a rare histologic subtype, pleomorphic carcinoma. In the Philippines, there is limited data on the incidence of this tumor subtype as local cancer registries do not specify histologic subtype or only include data for adenocarcinoma, squamous cell carcinoma, and small cell carcinoma, with other tumor types lumped together under a single category. However, it is important to recognize pleomorphic carcinomas as they are aggressive tumors that commonly present with distant metastases. Currently, there are few treatment options for these lesions and most studies have only shown, at most, a marginal benefit in survival. More research and clinical trials are needed to further our understanding and management of this disease.
References
- Bray F, Ferlay J, Soerjomataram I, Siegel R, Torre L, et al. (2018) Global Cancer Statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians
- Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG, et al. (2015) WHO Classification of Tumours of the Lung, Pleura, Thymus and Heart, 4th edn. IARC 88â??94.
- Borczuk AC (2018) Uncommon types of lung carcinoma with mixed histology. Archives of Pathology and Laboratory Medicine. 142: 914-915.
- Schrock AB, Frampton GM, Suh J, Chalmers ZR, Rosenzweig M, et al. Characterization of 298 Patients with Lung Cancer Harboring MET Exon 14 Skipping Alterations. J Thoracic Oncology
- Reungwetwattana T, Liang Y, Zhu V, Ignatius S (2013) The race to target MET exon 14 skipping alterations in non-small cell lung cancer : The Why, the How, the Who, the Unknown, and the Inevitable. Lung Cancer
- Viera T, Antoine M, Hamard C, Fallet V, Duruisseaux M, et al. (2016) Sarcomatoid lung carcinomas show high levels of programmed death ligand-1 (PD-L1) and strong immune-cell infiltration by TCD3 cells and macrophages. Lung Cancer
- Bae HM, Min HS, Lee SH, Kim DW, Chung DH, et al. (2007) Palliative chemotherapy for pulmonary pleomorphic carcinoma. Lung Cancer 58:112â??5.
- Vieira T, Antoine M, Hamard C (2016) Sarcomatoid lung carcinomas show high levels of programmed death ligand-1 (PD-L1) and strong immune-cell infiltration by TCD3 cells and macrophages. Lung cancer 98:51-8.
- Esteban D, Laudico A, Uy N, Benabay L (2001) Cancer registration in the Philippines. Asian Pacific J Cancer Prev 2: 55-60.
- Mapua C, Laudico A, Lumague M, Redaniel M, Patama T, et al. (2015) Cancer in the Philippines volume V.
- Cancer Registry Philippines. (2019). Cancer Database.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi