Commentary, J Trauma Stress Disor Treat Vol: 10 Issue: 5
Stress Impact of Covid-19 in Patients with Spinal Cord Injury
Gabriella Fizzottia1*, Giovani Fassinab2, Livio Tronconib2 and Carla Rognonic3
1Spinal Unit, ICS Maugeri SPA SB, Institute of Pavia, IRCCS, Pavia, Italy
2IRCCS Mondino Foundation Pavia, University of Pavia, Pavia, Italy
3Centre for Research on Health and Social Care Management (CERGAS), SDA Bocconi School of Management, Milan, Italy
*Corresponding Author:Gabriella Fizzottia
Spinal Unit, ICS Maugeri SPA SB Institute of Pavia
IRCCS, Pavia, Italy
Tel: 3337315328
E-mail:gabriella.fizzotti@ icsmaugeri.it
Received: April 16, 2021 Accepted: May 03, 2021 Published: May 10, 2021
Citation: Fizzottia G, Fassinab G, Tronconib L, Rognonic C (2021) Stress Impact of Covid-19 in Patients with Spinal Cord Injury. J Trauma Stress Disor Treat 10:5.
Abstract
Introduction
Stress is classically described as a response to something novel, unpredictable and uncontrollable, all features of the global COVID-19 pandemic. A stressor event causes the hypothalamic secretion of corticotropin-releasing hormone and the stimulation of the medulla of the adrenal with increased catecholamines. One of the most relevant disabilities is caused by spinal cord injury (SCI). The study aimed to evaluate the blood values of stress neurotransmitters: ACTH, cortisol, prolactin, TSH, FT3 and FT4 in SCI patients infected by COVID -19, in order to measure the different ways of responding to stressor events.
Material and Method
We have evaluated 6 patients admitted to the Spinal Unit of IRCCS Maugeri Foundation in the period between February and September 2020. The blood determination of stress neurotransmitters was being carried out on the first day of hospitalization in Spinal Unit after recovery from COVID-19.
Results
The values of the stress neurotransmitters don’t show significant differences in comparison between all the considered SCI patients.
Conclusions
The results highlighted the presence of a physiological response to stress in SCI patients affected by COVID 19.
Keywords
Covid 19; Stress; Spinal cord injury (SCI)
Keywords: Covid 19, Stress, Spinal cord injury
Keywords
Covid 19; Stress; Spinal cord injury (SCI)
Introduction
In December 2019 a novel coronavirus emerged in Wuhan, China causing many cases of severe pneumonia. World Health Organization (WHO) named this disease Coronavirus Disease 2019 (COVID-19). The main routes of transmission are respiratory droplets and direct contact with infected people, so numerous prevention strategies are employed to mitigate the spread of disease, including social distancing and isolation. These prevention strategies developed not only a life crisis, but also incurred psychological stress: tension, anxiety, fear and despair among affected people. A nationwide survey reported that, under the threat of COVID-19, the prevalence of psychological distress is up to 35% among the general population in China [1,2]. On March 17, 2020, the first case of Covid-19 was confirmed at the Hospital Nacional de Parapléjicos (HNP) in Toledo Spain, a hospital dedicated to the rehabilitation of people with acute and/or chronic spinal cord injury SCI [3].
SCI represent one of the most relevant disabilities. Typical causes of spinal cord damage are trauma, disease, or congenital disorders. Tetraplegia, also known as quadriplegia, is a paralysis caused by illness or injury that results in the partial or total loss of use of all limbs and torso; paraplegia is similar but does not affect the arms. The loss is usually sensory and motor, which means that both sensation and control are lost [4].With the spread of the COVID-19 pandemic, serious concerns are arising for people with SCI [5,6,7]. According to the high-risk comorbidity, mostly due to the presence of respiratory failure as a result of thoraco-abdominal muscle weakness [8] and also because of systemic immunosuppression due to injury [9,10]. The pandemic highlights the importance of stress as a factor in everyday life. The clinical research community has emphasized the importance of considering the pandemic as a multidimensional stressor to understand mental health consequences. The fear of illness for ourselves and our loved ones for an unknown period of time has been combined with, for example, prolonged disruptions to daily routine, education, child care, occupation and income that have resulted from efforts to limit the spread of the virus [11]. Isolation and lack of social support can also trigger maladaptive coping behaviours such as increased substance use that can potentiate risk for COVID19related complications [12] and interact with stress pathways to alter brain circuitry and cognitive function [13]. The stress system, causes the hypothalamic secretion of corticotropin-releasing hormone and the stimulation of the medulla of the adrenal with increased catecholamines. Mutual interactions are present between the amygdala and the hippocampus and the stress system, which activates these centers and in turn is regulated by them [14,15].
The study aimed to evaluate the blood determination of stress parameters in order to measure quantitatively the different ways of responding to stressor events of SCI persons during COVID -19 pandemic.
Materials and Methods
Five males and one female, aged between 17 and 85, treated at the Spinal Unit of Maugeri IRCCS Foundation were recruited consecutively from February to June 2020.Spinal cord injuries were classified as complete and incomplete by the American Spinal Injury Association (ASIA) classification [16]. The ASIA scale grades patients based on their functional impairment from A to E, where A represents the greatest impairment and E represents the normal condition. All patients presented acute SCI: three post traumatic, two spondylodiscitis and one post Arnold Chiari disease. The level of injury was cervical in three patients and lumbar in the other three patients. The blood determination of stress neurotransmitters: ACTH, cortisol (Figure 1), prolactin, TSH, FT3 and FT4 in SCI patients was being carried out on the first day of hospitalization in Spinal Unit after clinical recovery from COVID-19 as indicated by negative oropharigealswab. At that time, our hospital’s procedures required the opinion of an pneumology disease specialists before requesting a nasopharyngeal swab for the detection of SARS-CoV-2.disease.
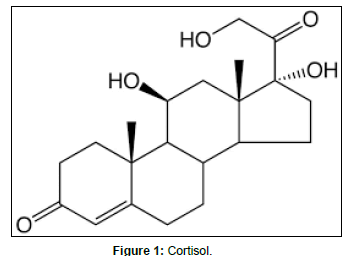
Figure 1: Cortisol.
Results
The blood values of the stress neurotransmitters don’t show any significant differences in comparison between all the patients in the acute phase. (AverageActh value:22,5pg/ml, Cortisol value: 12,8 mcg/ dl, mean Prolactin value: 12,9 ng/ml, mean FT3, FT4 values: 0,63 pg/ml and 1,54 pg/ml. Our results support the recommendation of restricting ormonmeasurements to the morning hours in all patients (Table 1).
Table 1: Measurements to the morning hours in all patients.
Discussion
The importance of an intact hypothalamic-pituitary axis for metabolic and immunological homeostasis during stress is well recognized. Our data provide preliminary evidence indicating that the values of stress neurotransmitters reporting no change after Covid-19 in SCI patients. According to the scanty available data from an Italian case report [17] and a Spanish series of seven SCI patients [18], COVID-19 evolution seems to be not so dramatic as expected. Other authors have hypothesized that people with SCI would be at increased risk of morbidity and mortality by COVID-19 [19,20] because the individuals with SCI develop many physiological changes that not only increase their risk of morbidity from COVID-19, but may also mask the presentation of an acute respiratory illness which can potentially delay the diagnosis of COVID-19. These include temperature dysregulation, impaired cough, and abnormal sensations at or below the neurological level of injury [21-24]. In this study all considered patients develop mild or uncomplicated illness, with a complete healing in little more than 2 weeks and no need for mechanical ventilation: this is in contrast with the acknowledged SCI induced immune depression syndrome [25]. A spinal cord injury determines a condition of severe disability with sudden onset with a consequent increase in stress: the person passes from a condition of total autonomy to a condition of total dependence having to face an important adaptive response. The stress response involves intricate interactions between the central nervous system (CNS), the peripheral nervous system and the rest of the body. The increase in cortisol is an essential part of the body’s stress response, triggering adaptive changes in metabolism, cardiovascular function, and immune regulation [26]. Bruce McEwen, demonstrated the presence of the receptors for corticosterone in the hippocampus in 1968 [27]. The portal of entry of the virus into the hypothalamuspituitary could be either directly thorough the cribriform plate via hematogenous route. Nevertheless, frank hypocortisolism has never been documented in patients with active SARS (or COVID-19). Rimesh evaluated serum cortisol and ACTH in patients with severe COVID-19 in a prospective study [28]. Tan and colleagues showed that cortisol concentrations in patients with COVID-19 were significantly higher than in those without COVID-19. [29]. Furthermore, other Authors found that high cortisol concentrations were associated with increased mortality and a reduced median survival, probably because this is a marker of the severity of illness [30]. Based on the expected response of the adrenal gland in stressful conditions such as infection, the past few years have seen some studies on the possibility of using the measurement of serum cortisol level as a potential biomarker that was associated with severity and deaths in community-acquired pneumonia (CAP). The nonsurvivors among patients with CAP had significantly higher serum cortisol level in comparison with survivors. This is in line with some previous studies in this area that revealed the role of cortisol in predicting deaths among these patients [31,32,33]. Stress is also an important physiologic cause of hyperprolactinemia, [34]. Some studies suggest that prolactin secretion during stress acts to maintain homeostasis within the immunesystem.Whilegluco-corticoids, also released in response to stress, are suppressive immune modulators, prolactin and growth hormone stimulate the immune system [35]. Considerable prolactin secretion occurs when animals are exposed to physical or psychological stress [36].Prolactin is a unique hormone in its wide reaching effects as well as its modulation by physical, psychological, and environmental factors. There is evidence that prolactin also mediates pathological effects of chronic stress. Chronic stress induces expression of prolactin receptors in choroid plexus cells [37]and upregulates prolactin receptor expression in the heart [38]. Min Chen et al.[39]. Found that the patients with COVID-19 had low TSH and TT3 levels, and the degree of the decreases in their TSH and TT3 levels positively correlated with the severity of their COVID-19. The fact that the serum TSH levels of the patients with COVID-19 were significantly lower in the severe and critical group compared with nonCOVID-19 pneumonia patients with a similar degree of severity also indicates there might be a unique effect of COVID-19 on TSH-secreting cells. Two possible mechanisms might account for these changes. One is a direct viral effect on the pituitary cells and another is an indirect effect wherein various systemic changes such as the activation of various proinflammatory cytokines caused by the virus infection [40,41] or its treatment led to hormonal changes in the pituitary–endocrine axis feedback loops. The observed decrease in TSH level in patients with COVID-19 could be induced by chronic stress from hypoxemia and the glucocorticoids with which most patients were treated, though the dosage was low. Another previous study showed that the TT3, TT4, and TSH levels of patients with SARS were considerably lower than those of controls in both the progression and recovery phases [42]. The neuroendocrine response to stress is a dynamic process [43]. The importance of an intact hypotalamycpituitary axis for metabolic and immunological homeostasis during stress is well recognized. In our study ACTH, Prolactin, Ft3 and Ft4 serum values were measured together and we thought it opportune in a contest from COVID-19 pandemic. The physiological blood levels of stress neurotrasmitters in the recruited patients could be justified by the condition of recovery from COVID-19 and because all considered patients develop mild or uncomplicated illness. Another possible explanation for the mild neuroendocrine response to stress impact to COVID-19 in this patient may be a postulated different susceptibility to SARS-CoV-2 based on genetic [44] and epigenetic [45] factors and the actual viral load that they received upon infection. Further studies are required for conclusion. There are several limitations to the described study. These findings must be replicated in a longer term study that has a larger sample, including a no-COVID-19, SCI control group. Further researches are needed in this direction to develop valid and reliable instruments to assess the health status in people with SCI. Our hope is that this pandemic will expose the need for universal health care and will mobilize public support for its implementation. In our study, serum cortisol levels were measured at the time of presentation: eight in the morning. Standardized stress ormons values determined at the same time of day in all patients would most probably have an even higher prognostic accuracy. On the contraryi it is also possible that serial measurements over the course of the disease may add prognostic information, and show differences in the values [46].
Conclusions
The results obtained showed the presence of a physiological response to stress in SCI patients without significant differences in the acute phase of SCI which may imply the same reactivity to stressor events.
Funding
This research received no specific grant from any finding agency in the public, commercial or not for profit sectors.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research authorship and/or publication of this article.
Patient Consent
Obtained.
The study was approved by the Ethics Committee of our Centre and all patients provided written informed consent before study treatment.
Provenance and Peer Review
Not commissioned; externally peer reviewed.
References
- Elizabeth V, Goldfarb, (2020) Partecipant stress in the COVID-19 era and beyound. Nature Reviews Neuroscience,663-664.
- Qiu J.Y, Shen B, Zhao M, Wang Z, Xie B, (2020) A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry, 33(2)
- Hopkins J, (2020) Coronavirus COVID-19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). JHU COVID-19 Resource Center. Coronavirus Resource Center,
- Kirshblum S, Campagnolo D, Delisa J, (2001) Spinal Cord Medicine. Lippincott Williams & Wilkins, 3(1): 108-122.
- Korupolu R, Stampas A, Gibbons C, Hernandez Jimenez I, Skelton F, et al (2020) COVID-19: screening and triage challenges in people with disability due to spinal cord injury. Spinal Cord Ser Cases, 6: 35.
- López-Dolado E, Gil-Agudo A, (2020) Lessons learned from the coronavirus disease 2019 (Covid-19) outbreak in a monographic center for spinal cord injury. Spinal Cord, 58: 517–519
- Dicks MA, Clements ND, Gibbons CR, Verduzco-Gutierrez M, Trbovich M, et al (2020) Atypical presentation of Covid-19 in persons with spinal cord injury. Spinal Cord Ser Cases, 6(1) :38.
- Shah A, Shem K, McKenna S, BerllyY M, (2011) Respiratory management of the spinal cord injured patients. In: Kirshblum S, Campagnolo DI, editors. Spinal cord medicine. Philadelphia: Lippincott Williams & Wilkins,
- Riegger T, Conrad S, Liu K, Schluesener HJ, Adibzahdeh M, et al (2007) Spinal cord injury-induced immune depression syndrome (SCI-IDS). Eur J Neurosci, 25 (6): 1743–1747.
- Kasinathan N, Vanathi MB, Subrahmanyam VM, Rao JV, (2015) A review on response of immune system in spinal cord injury and therapeutic agents useful in treatment. Curr Pharm Biotechnol, 16 (1): 26–34.
- Gruber J, (2020) Mental health and clinical psychological science in the time of COVID-19: Challenges, opportunities, and a call to action. Am. Psychol
- Volkow N. D, (2020) Collision of the COVID-19 and addiction epidemics. Ann. Intern. Med, 173 (1): 61–62.
- Wemm, S. E, Sinha R, (2019) Drug- induced stress responses and addiction risk and relapse. Neurobiol Stress, 10: 100148
- Benno R, Bruce S, McEwen, Sumantra C, (2009) Stress, memory and the amygdala. Nature Review. Neuroscience, 10 (6): 1364-1370.
- Chattarji S, Rajnish P, (2014) Resilience vs. susceptibility to stress: insights from blood-brain biomarkers. Proc. Natl. Acad. Sci, 37:13253-13254
- Kirshblum SC, Waring W, Biering-Sorensen F, (2011) revision of the International Standards for Neurological Classification of Spinal Cord Injury. J Spinal Cord Med, 34(6): 547-554
- Righi G, Del Popolo G, (2020) COVID-19 tsunami: the first case of a spinal cord injury patient in Italy. Spinal Cord Ser Cases, 6:22.
- Rodríguez-Cola M, Jiménez-Velasco I, Gutiérrez-Henares F, López-Dolado E, Gambarrutta-Malfatti C, et al.(2019) Clinical features of coronavirus disease (COVID-19) in
- a cohort of patients with disability due to spinal cord injury. Spinal Cord Ser Cases,6(1): 39
- Korupolu R, Stampas A, Gibbons C, Hernandez Jimenez I, et al (2020) COVID-19 screening and triage challenges in people with disability due to spinal cord injury. Spinal Cord Ser Cases, 6:35.
- López-Dolado E, Gil-Agudo A,(2020) Lessons learned from the coronavirus disease 2019 (Covid-19) outbreak in a monographic center for spinal cord injury. Spinal Cord, 58: 517–519
- Berlowitz DJ, Wadsworth B, Ross J, (2016) Respiratory problems and management in people with spinal cord injury. Breathe,12: 328–340.
- Cardozo CP, (2007) Respiratory complications of spinal cord injury. J Spinal Cord Med, 30 (4): 307–308
- Price MJ, Trbovich M, (2018) Thermoregulation following spinal cord injury. Handb Clin Neurol, 157: 799–820.
- Sezer N, Akkus S, Ugurlu FG, (2015) Chronic complications of spinal cord injury. World J Orthop, 6 (1): 24–33.
- Meisel C, Schwab JM, Prass K, Meisel A, Dirnagl U, et al (2005) Central nervous system injury-induced immune deficiency syndrome. Nat Rev Neurosci,6 (10): 775–86
- Teblick A, Peeters B, Langouche L, Van den Berghe G, (2019) Adrenal function and dysfunction in critically ill patients. Nat Rev Endocrinol, 15: 417–427.
- McEwen BS, Weiss JM, Schwartz LS, (1968) Selective Retention of Corticosterone by Limbic Structures in Rat Brain. NATURE, 220 (5170): 911-912.
- Rimesh P, (2020) COVID-19, hypothalamo-pituitary-adrenal axis and clinical implications. Endocrine 68 (2): 251-252.
- Tan T, Khoo B, Mills EG,(2020) Association between high serum total cortisol concentrations and mortality from COVID-19. Lancet Diabetes Endocrinol ,8 (8): 659–60.
- Christ-Crain M, Stolz D, Jutla S, (2007) Free and total cortisol levels as predictors of severity and outcome in community-acquired pneumonia. Am J Respir Crit Care Med , 176 (9): 913–20.
- Omelyanenko O, Makarevich A, Amelchenko E, Rybina T, (2011) Prognostic value of cortisol and adrenocorticotropic hormone (ACTH) in severe community-acquired pneumonia (SCAP) patients. Eur Respir J,38: 1473.
- Kolditz M, Höffken G, Martus P, Rohde G, Schütte H, et al. (2012) Serum cortisol predicts death and critical disease independently of CRB-65 score in community-acquired pneumonia: a prospective observational cohort study. BMC Infect Dis, 12:90.
- Lu H, Zeng N, Chen Q, Wu Y, Cai S, et al. (2019) Clinical prognostic significance of serum high mobility group box-1 protein in patients with community-acquired pneumonia. J Int Med Res,47 (3): 1232–1240.
- Jaroenporn S, Nagaoka K, Kasahara C, Ohta R, Watanabe G, et al (2007)“Physiological roles of prolactin in the adrenocortical response to acute restraint stress.” Endocrine Journal, 54( 5): 703-711
- Ochoa-Amaya J. E, Malucelli B. E, Cruz-Casallas P. E,(2010) “Acute and chronic stress and the inflammatory response in hyperprolactinemic rats.” Neuroimmunomodulation, 17(6): 386–395.
- T. Fujikawa H, Soya K. L. K, Tamashiro (2004)“Prolactin prevents acute stress-induced hypocalcemia and ulcerogenesis by acting in the brain of rat.” Endocrinology, 145(4): 2006–2013.
- Ochoa-Amaya J. E, Malucelli B. E, Cruz-Casallas P. E, (2010) “Acute and chronic stress and the inflammatory response in hyperprolactinemic rats.” Neuroimmunomodulation, 17( 6): 386–395.
- Song J, Wang X, Chenetal, (2016)“Prolactin mediates effects of chronic psychological stress on induction of fibro fatty cell sin the heart.”American Journal of Translational Research, 8 (2): 644-652
- Min C, Weibin Z, Weiwei X, (2020) Tyroid function analysis in 50 patients with Covid – 19: a retrospective study,Thyroid 00: 1-4
- Fliers E, Bianco AC, Langouche L, Boelen A, (2015) Thyroid function in critically ill patients. Lancet Diabetes Endocrinol,3(10): 816–825.
- Greet van den B, (2014) Non-thyroidal illness in the ICU: a syndrome with different faces. Thyroid,24 (10): 1456–1465.
- Wang W, Ye YX, Yao H, (2003) Evaluation and observation of serum thyroid hormone and parathyroid hormone in patients with severe acute respiratory syndrome. J Chin Antituberculous Assoc, 25:232–234.
- Greet Van den B
- Best Practice & Research: Clinical Endocrinology & Metabolism
- .Corley MJ, Ndhlovu LC, (2020) DNA methylation analysis of the COVID-19 host cell receptor, angiotensin I converting enzyme 2 gene (ACE2) in the respiratory system reveal age and gender differences. Preprints.
- Cai G, Cui X, Zhu X, Zhou J, (2020) A hint on the COVID-19 risk: population disparities in gene expression of three receptors of SARS-CoV. Preprints,2020020408.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi 
