Case Report, Int J Ophthalmic Pathol Vol: 10 Issue: 3
Successful Clinical and Demographic Profile of Vasculitis Retinae in a Tertiary Eye Care Centre of Bangladesh
Jasmin Ahmad1* and Sweety Barua2
1Department of Ophthalmology, Institute of Community Ophthalmology, Bangladesh
2Department of Surgery, Chittagong Eye Infirmary & Training Complex, Bangladesh
- *Corresponding Author:
- Dr. Jasmin Ahmad
Associate Professor, Department of Ophthalmology
Institute of Community Ophthalmology, Chattagram, Bangladesh
E-mail: drjasmin19@gmail.com
Received: February 23, 2021 Accepted: March 17, 2021 Published: March 24, 2021
Citation: Ahmad J, Barua S (2021) Successful Clinical and Demographic Profile of Vasculitis Retinae in a Tertiary Eye Care Centre of Bangladesh. Int J Ophthalmic Pathol 10:3.
Abstract
Aims: To evaluate the demographic and clinical pattern of vasculitis retinae along with outcome after appropriate management presenting in a tertiary eye care centre.
Methods: A retrospective record based case series of 17 eyes of 11 cases of vasculitis retinae presented at Chittagong Eye Infirmary & Training Complex (CEITC) from October 2015 to April 2019. The demographic features were noted. Data included detail history of systemic and ocular disease, result of clinical examination and ocular examination such as, Best Corrected Visual Acuity (BCVA), slit lamp biomicroscopy, indirect ophthalmoscopy, Fundus Fluorescein Angiography ( FFA ) , Optical Coherence Tomography (OCT) scan ,B scan ultrasonography were performed according to the cases. Data also include laboratory investigation, treatments details along with prognosis. An internet search (medline search) and review of current literature on vasculitis retinae was performed.
Results: 17eyes of 11 patients (54.50% had bilateral) presented with vasculitis retinae ,all of them were male with mean age of 26.9 ( ± 1.03) years.100% of them received topical and systemic steroids, sectoral and pan retinal photocoagulation due to new vessels formation and vitreous haemorrhage. 8(47.1%) eyes received intra vitreal injection of anti VEGF .Pars plana vitrectomy with endo laser was needed in one (5.88%) eye. Overall best corrected visual acuity improved from presentation to final follow up. 6/6 vision in 17.65% at presentation improved to 41.18 % at last follow up,6/9 to 6/18 vision 23.53% at presentation again improved to 35.29 % at last follow up. Vision equal and less than 6/24 is in 58.82 % eyes at presentation reduced to 23.53 % at mean follow up of 16.36 ( ± 1.5) months. During the follow up period out of 17 eyes, 8 (47.1%) eyes experienced visual acuity improvement of two or more lines on the Snellen chart. Conclusion: Appropriate treatment improving the overall outcome including vision.
Keywords: Vasculitis retinae; Vascular sheathing; Retinal haemorrhage; Vitreous haemorrhage
Keywords
Vasculitis retinae; Vascular sheathing; Retinal haemorrhage; Vitreous haemorrhage
Introduction
Retinal vasculitis represents a group of diseases characterized by inflammation of the retinal vasculature along with intra ocular tissue [1,2]. Both venular and arteriolar inflammation have nearly equal prevalence .3 It is fairly uncommon disease [2-4] that mostly occur as an isolated disorder5 or in association with other ocular diseases like a manifestation of infectious [5-7] ( tuberculosis ,syphilis, toxoplasmosis, lime disease, viral ARN )or neoplastic [7] disorders or with systemic inflammatory diseases like sarcoidosis, systemic lupus erythematosus [1,4]. But retinal vasculitis is not a part or rarely associate with systemic vasculities [4]. Immune process [5] (autoimmune mechanism [5, 8, 9] or against tubercular protein [6]) are thought to be responsible for retinal vasculitis occurs without systemic menifestations, but the exact etiology and pathogenesis remain unknown [4-6].
Retinal vasculitis is mostly an isolated idiopathic condition without any positive systemic correlation found in history, examination and laboratory tests, so the condition named as primary retinal vasculitis [1, 2, 5, 7].
Clinical menifeststions of retinal vasculitis demonestrable by retina examination include ophthalmoscopic examinations or fluorescein angiography includes perivascular sheathing or cuffing, vascular leakage and occlusion of vessels in association with intraocular inflammation [5-7, 10]. Optical coherence tomography is an effective method for the diagnosis and measurements of macular edema in micrometers; it has a great value in assessing the results of treatment [7]. The disease may be asymptomatic [5, 7] Patients are most commonly presented with blurring of vision, floaters and scotomata [5, 7].
To diagnose, find out an underlying etiology and to provide a proper management a meticulous workup should be undertaken based on a detailed medical history, thorough systems, and ocular examination, laboratory investigation of patients with retinal vasculitis is an essential component [1-3].
Although uncommon, it affect young adult (Third and fourth decade of life) [3, 6, 8] and is a potentially sight-threatening condition which needs prompt and appropriate management [4, 5].
Treatment of retinal vasculitis depend on stage of disease [8], at early stages the inflammatory process well respond to topical and systemic corticosteroid [11], even the vision threatening conditions that might respond to steroid but some time require aggressive immunosuppressant [4,5] Infectious causes of retinal vasculitis treated with additional antimicrobial therapy. The main causes of visual loss are cystoid macular edema, retinal ischemia and new blood vessel formation [3,7] can be treated with intravitreal anti VEGF injection and laser photocoagulation [8].
Good prognosis can be achieved with adequate treatment [5, 10, 11]. Poor visual outcome despite therapy often is associated with complications such as macular ischemia, retinal vein occlusion, branch retinal artery occlution, neovascuiarization, persistent vitreous hemorrhage and tractional retinal detachment [3, 5, 6, 10].
Retinal vasculatis is not common one, so there are only a limited number of publications over the past years [2] and most of the studies reported from the Indian subcontinent as the disease is more common here [1,3,6,8]. To our knowledge, no population based clinical studies or reports on Bangladeshi patients with vasculitis retinae have been yet published.
Our present study was done to analyze the patients with retinal vasculitis in a tertiary eye care center of Bangladesh. This study was aimed to provide a demographic, clinical menifestations, treatment and prognosis after proper treatment of vasculitis retinae.
Methodology
The medical records of 17 eyes of 11 patients who were diagnosed and treated as a case of vasculitis retinae visited at Chittagong Eye Infirmary & Training Complex (CEITC) from October 2015 to April 2019 were reviewed retrospectively. 6 patients had bilateral involvement rest 5 had unilateral. The demographic features like age, sex were noted. The data included detail medical history of systemic and ocular diseases, duration of symptoms with laterality, result of systemic and ocular examination. Ocular examination included best corrected visual acuity (BCVA), anterior segment slit lamp examination, and posterior segment slit lamp biomicroscopy, indirect ophthalmoscopy, applanation tonometry. Features of vasculitis retinae were noted from the standard fundus drawing made at the first visit. The noted signs were vascular sheathing/cuffing, occlusion of vessels, vitreous cells, retinal neovascularization, vitreous hemorrhage, status of the macula. Findings of Fundus Fluorescein Angiography (FFA) like vascular leakage, area of capillary non perfusion, Optical Coherence Tomography (OCT) scan for macular status, B scan ultrasonography for opaque media etcetera whenever performed according to the cases also recorded in the data sheet. Data also include tailored laboratory investigations (Table 1), treatments details along with prognosis. The mean follow up was 16.36 (± 1.5) months.
Table 1: Laboratory investigations performed for patients with vasculitis retinae.
| I .Routine tests | Complete Blood count with ESR |
| Random blood sugar | |
| X ray Chest | |
| Urine routine test | |
| II. Infectious Disease | Tuberculine skin test |
| VDRL | |
| TPHA | |
| FTA-ABS |
Note: ESR = Erythrocyte sedimentation rate ; VDRL = Venereal Disease Research Laboratory; TPHA = Treponema Pallidum Hemo Agglutination test; FTA-ABS = Fluorescent Treponemal Antibody Absorption Test
An internet search (med line search) and review of current literature on vasculitis retinae was performed.
Results
This study included seventeen eyes of eleven patients with vasculitis retinae. Among them 6 (54.50%) had bilateral involvement and 5 ( 45.50 %) had unilateral involvement (Table 2).
Table 2: Involved eye of the respondents
| Frequency | Percent | Valid Percent | Cumulative Percent | |
|---|---|---|---|---|
| Valid Bilateral | 6 | 54.5 | 54.5 | 54.5 |
| Unilateral | 5 | 45.5 | 45.5 | 100 |
| Total | 11 | 100 | 100 | - |
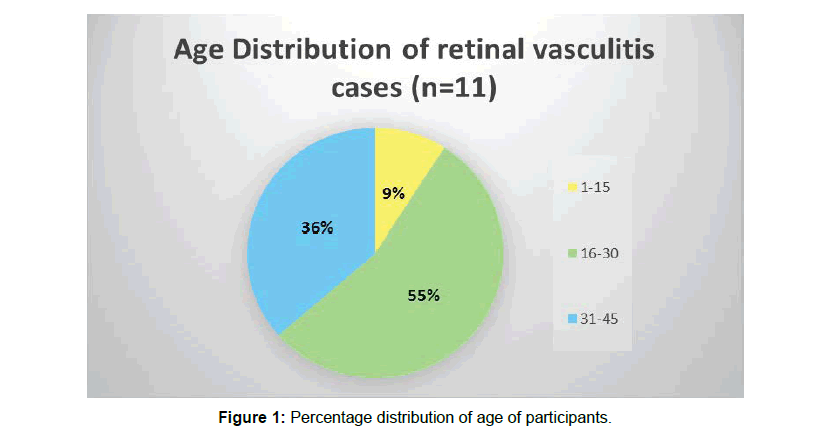
Mean age of the participants was 26.9091 (SD ± 1.03485E1) years (range 14–43 years) .55% of participants were within 16 to 30 years of age. Only 9% of them were bellow 15 years of age and 36% were above 30 years of age (Figure 1).
All of our study patients were male. Again all (100%) patients were presented with dimness of vision, 2 (11.76%) had pain and redness along with blurred vision. Mean duration of symptoms 4.73 weeks (SD ± 5.95) (range 01– 20 weeks) (Table 3)
Table 3: Duration of symptoms (week)
| N | Valid | 11 |
| Missing | 0 | |
| Mean | 4.7273 | |
| Median | 2 | |
| Std. Deviation | 5.95132 | |
| Minimum | 1 | |
| Maximum | 20 | |
We did not get any systemic association in our study cases except two ,one (9.09%) who had diabetis another one (9.09%) had asthma.
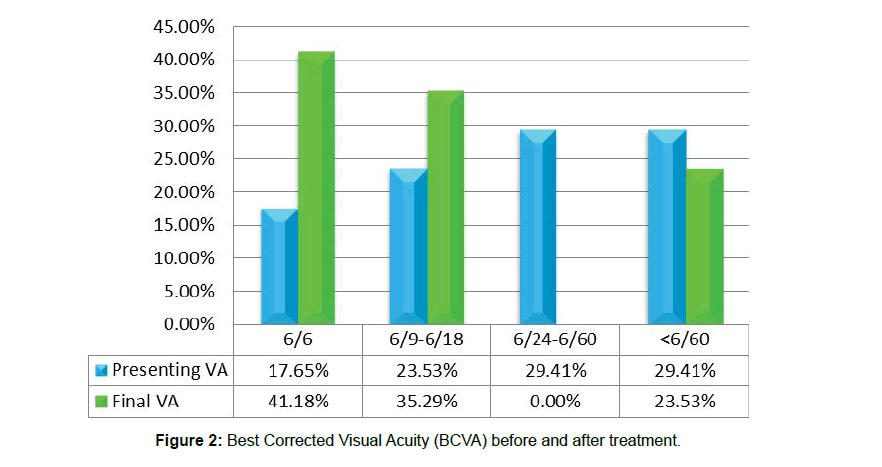
In this study at presentation 5 (29.41%) eyes showed BCVA less than 6/60, 5 (29.41%) eyes had BCVA 6/24 to 6/60, 4 (23.53 %) eyes had 6/9 to 6/18 and 3 (17.65%) eyes had 6/6. But after treatment 7 (41.18 %) eyes got 6/6 vision, 6 (35.29 %) eyes got 6/9 to 6/18 vision and 4 (23.53 %) eyes showed BCVA less than 6/60. (Table 4 and Figure 2). Three eyes of 2nd, 7th and 11th patients had lost vision up to 2/60, hand movement and 1/60 respectively due to NVG (New vascular Glaucoma) and RD (Retinal Detachment). Vision in 6 (35.29 %) eyes remain stable,1(5.88%) gain 2 lines,2 (11.76%) eyes gain 3 lines,2 (11.76%) eyes gain 4 lines, 2 (11.76%) eyes gain 5 lines, 1(5.88%) eye improved 7 lines on the Snellen chart during follow-up period. Anterior segment of study cases showed 1(5.88%) corneal oedema, Keratic Pricipitates in 3 (17.6%) eyes, 2 (11.88%) eyes showed Cells in Anterior chamber, 1(5.88%) eye had Posterior Synechiae , Rubeosis present in 2 (11.88%) eyes (Table 5 and Figure 3).
Table 4: BCVA Before and after treatment
| BCVA | At presentation | At last follow up | ||
|---|---|---|---|---|
| Before Treatment | After Treatment | |||
| Number of eyes(N) | % | Number of eyes (N) | % | |
| 6-Jun | 3 | 17.65 | 7 | 41.18 |
| 6/9-6/18 | 4 | 23.53 | 6 | 35.29 |
| 6/24-6/60 | 5 | 29.41 | - | - |
| >6/60 | 5 | 29.41 | 4 | 23.53 |
| Total | 17 | 100 | 17 | 100 |
Table 5: Anterior Segment of retina vasculitis cases (n=17)
| Anterior segment Segment | N | % |
|---|---|---|
| Cornel Oedema | 1 | 5.88 |
| Keratic Pricipitates (KP) | 3 | 17.6 |
| Cells (in Anterior chamber) | 2 | 11.8 |
| PS (Posterior Synechiae) | 1 | 5.88 |
| Rubeosis | 2 | 11.8 |
| NAD (No abnormalities Detected) | 7 | 41.2 |
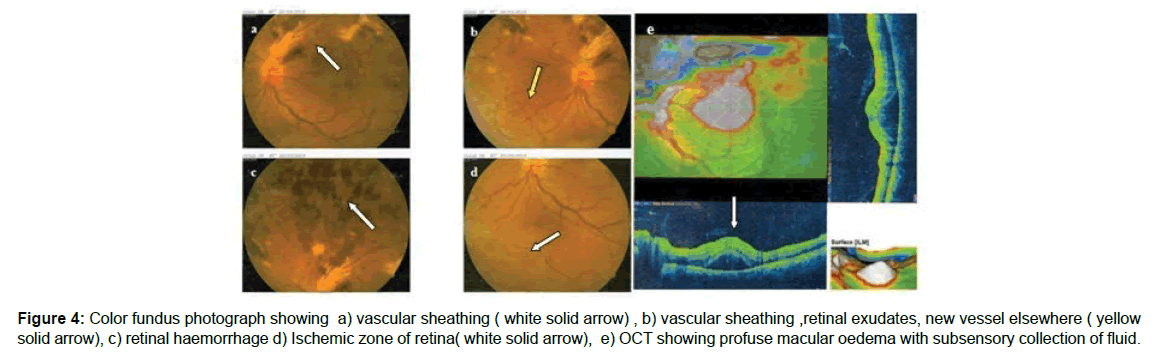
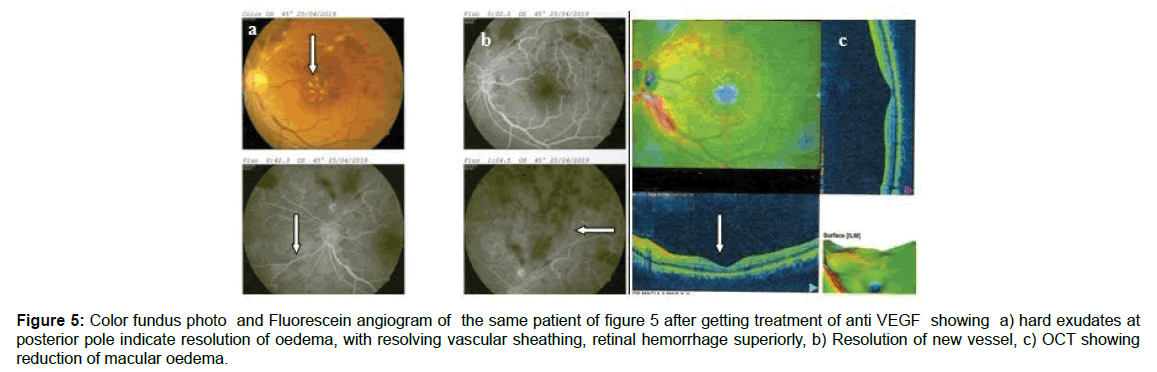
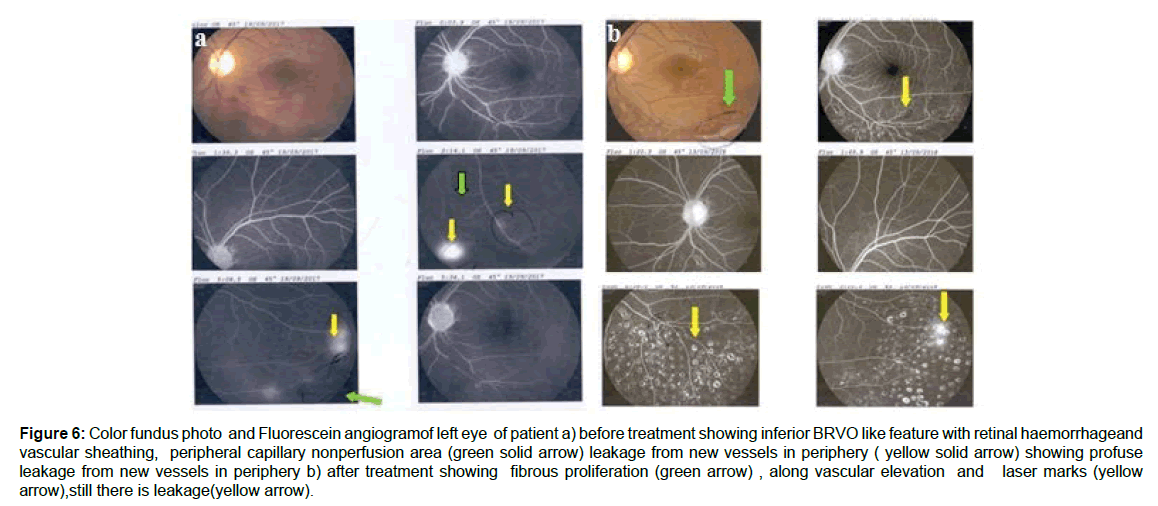
On posterior segment examination we found Vitreous hemorrhage in 6 (35%) eyes, vitreous cells in 7 (41.2 %), vitreous exudates in 3(17.6%) eyes, retinal haemorrhage in 5 (29.41%) eyes, retinal exudates in 3 (17.56%) eyes, out of 17 vascular sheathing found in only 9 (52.94%) eyes making it most common findings ,occluded vessel in 2 (11.76) eyes, disc oedema in 2 (11.76) eyes and macular oedema in one eye (5.88%).New vessels elsewhere found in one eye (5.88%) and Fibrovascular Proliferation in one eye (5.88%) (Table 6 and Figures 4- 6).
Table 6: Clinical Findings in retinal vasculitis eyes (n=17)
| Posterior Segment | N | % |
|---|---|---|
| Vitreous hemorrhage | 6 | 35.29 |
| Vitreous Cells | 7 | 41.18 |
| Vitreous exudates | 3 | 17.65 |
| Retina Haemorrhage | 5 | 29.41 |
| Retina exudates | 3 | 17.65 |
| Vascular sheathing | 9 | 52.94 |
| Occluded vessels | 2 | 11.76 |
| Disc Oedema | 2 | 11.76 |
| Macular Edema | 1 | 5.88 |
| Retinal Detachment | 1 | 5.88 |
| New Vessels else where | 1 | 5.88 |
| Fibrovascular Proliferation | 1 | 5.88 |
Figure 4: Color fundus photograph showing a) vascular sheathing ( white solid arrow) , b) vascular sheathing ,retinal exudates, new vessel elsewhere ( yellow solid arrow), c) retinal haemorrhage d) Ischemic zone of retina( white solid arrow), e) OCT showing profuse macular oedema with subsensory collection of fluid.
Figure 5: Color fundus photo and Fluorescein angiogram of the same patient of figure 5 after getting treatment of anti VEGF showing a) hard exudates at posterior pole indicate resolution of oedema, with resolving vascular sheathing, retinal hemorrhage superiorly, b) Resolution of new vessel, c) OCT showing reduction of macular oedema.
Figure 6: Color fundus photo and Fluorescein angiogramof left eye of patient a) before treatment showing inferior BRVO like feature with retinal haemorrhageand vascular sheathing, peripheral capillary nonperfusion area (green solid arrow) leakage from new vessels in periphery ( yellow solid arrow) showing profuse leakage from new vessels in periphery b) after treatment showing fibrous proliferation (green arrow) , along vascular elevation and laser marks (yellow arrow),still there is leakage(yellow arrow).
The men IOP (Intra Ocular pressure) of study cases at presentation were 16.76 (+_9.42) mm of hg with range (10 -40) mm of hg. .2nd case (Right eye) showed high IOP due to NVG,8th case left eye had high IOP 40 mm of hg and 10 patient (left eye) had 24 mm of hg ,other eyes showed normal IOP along their follow up period (Table 7).
Table 7: IOP of the respondents at presentation.
| N | Valid | 17 |
| Missing | 0 | |
| Mean | 16.7647 | |
| Std. Deviation | 9.4176 | |
| Minimum | 10 | |
| Maximum | 40 | |
In study cases we get glaucoma, retinal break, retinal detachment, vitreous haemorrhage, new vascular glaucoma, epiretinal membrane (Table 8). 2 patients (9th and 10 th) were steroid responder. Among the study cases 9(52.54%) eyes presented with vasculitis retinae (VR) ,4(23.53%) eyes presented with vitreous haemorrhage (VH), 2 (11.76%) eye came with NVG, 1 (5.88%) eye presented with BRVO (Branch Retinal Vein Occlusion), 1 (5.88%) eye presented with CRVO (Central Retinal Vein Occlusion)(Figure 7 and Table 9) None of our study case showed any abnormalities in laboratory investigation , no one showed high ESR (highest reading was 20 mm) also no one showed positive tuberculine test.
Table 8: Complications of retina vasculitis cases (n=17)
| Complication | N | % |
|---|---|---|
| Glaucoma | 1 | 5.88 |
| Retinal Break | 1 | 5.88 |
| Retinal Detachment | 1 | 5.88 |
| Vitreous Haemorrhage | 1 | 5.88 |
| New Vascular Glaucoma | 2 | 11.76 |
| Epi Retinal Membrane | 1 | 5.88 |
Table 9: First presentation of affected eye
| Frequency | Percent | Valid Percent | ||
|---|---|---|---|---|
| Valid | VR | 9 | 52.54 | 52.54 |
| VH | 4 | 23.53 | 23.53 | |
| NVG | 2 | 11.76 | 11.76 | |
| BRVO | 1 | 5.88 | 5.88 | |
| CRVO | 1 | 5.88 | 5.88 | |
| Total | 17 | 100 | 100 |
All of the patient (17 eyes, 100%) received topical and systemic (Oral) steroid. 5 (29.40 %) eyes of 3 patients (4th,7th,10th) get Immunosuppressive drugs in the form of Methotraxate, 2 (11.76%) eyes get anti glaucoma medication. Out of 17 eyes 9 (52.90%) eyes get laser photocoagulation, among them 4 (23.50%) eyes get sectoral laser and 5 (29.40%) eyes received Pan Retinal Photocoagulation(PRP). 8 (47.1%) eyes received intra vitreal injection of anti VEGF (anti vascular endothelial growth factor). Only one eye (5.88%) of 8th case needed pars plana vitrectomy surgery (Table 10). After receiving treatment 1st case (both eyes) became stable, 2nd (right eye) and 6th (both eyes) case become worst and rest of the cases (eyes) are improved. 3rd case ( left eye ) 9th case(right eye) showed recurrence. The mean follow up period of study cases were 16.36 ( ± SD 1.5) months with a range of 4 to 46 months (Table 11).
Table 10: Treatment for retinal vasculitis (n=17)
| Treatment | N | % |
|---|---|---|
| Topical steroid | 17 | 100 |
| Systemic Steroid | 17 | 100 |
| Immunosuppressive drugs (Methotraxate) | 5 | 29.4 |
| Anti-glaucoma medication | 2 | 11.76 |
| Sectoral Laser Photocoagulation | 4 | 23.5 |
| Pan Retinal Laser Photocoagulation | 5 | 29.4 |
| Anti-VEGF Injection | 8 | 47.1 |
| Pars Plana vitrectomy Surgery | 1 | 5.88 |
Table 11: Follow up period in months
N |
Valid | 11 |
| Missing | 0 | |
| Mean | 16.3636 | |
| Std. Error of Mean | 4.60093 | |
| Std. Deviation | 1.52596E1 | |
| Minimum | 4.00 | |
| Maximum | 46.00 | |
Discussion
Retinal vasculitis is rare but sight threatening disease affecting relatively healthy young patient [1-3, 10 ]. The peak age of onset is 20 to 30 years [3]. We also get similar result that the mean age of this present study cases was 26.9 ( ± 1.03) years. All participants of this study were male. Most of the literature showed male preponderance [1-3, 8-10].
The disease has four stages of natural course: I) Active Inflammatory stage: Involve small and large calibre vessel with superficial retinal haemorrhage II) Ischemic stage: Peripheral capillary non-perfusion III) Proliferative stage: Neovascularization (elsewhere and on disc), Fibrovascular proliferation and vitreous haemorrhage IV) stage of complication (non resolved massive VH, Rubeosis iridis leading to NVG, tractional RD and combined with rhegmatogenous Rd) [3,8,9].
Due to vascular inflammation there is development of retinal capillary closure and with progressive retinal non-perfusion and ischaemia stimulate to neovascular proliferationfrom perfused area usually at the junction of perfused and non-perfused retina. These new vessel resulting in vitreous haemorrhage, neovascular glaucoma, development of fibrosis cause tracrtional retinal detachment, retinal tear and rhegmatogenous retinal detachment and ultimate faded as blindness [3, 9].
At early stage patient may remain unaware as the central retina remain uninvolved even after extensive peripheral nonperfusion but macular oedema3 sometime develop result in drop down of vision and progress to ERM (Epi Retinal Membrane) formation .Vitreous haemorrhage from new vessels at proliferative stage and RD cases severe visual loss.NVG development is the most devastating causing worst prognosis. We get 4 (23.5%) eyes in stage I, 10 (58.8%) eyes in stage II to III, and 3 (17.6%) eyes with complications.
The etiology of retinal vasculitis may be immune-mediated, infectious or malignant one [10]. But there is a major group of retinal vasculitis where no positive clue of etiological agent found on history, clinical examination and laboratory investigations termed as primary retinal vasculitis [1-3].
All of our study cases were found to be primary retinal vasculitis similar to the findings of Saurabh K and his co-worker [1].
Most of this study patients (54.5%) had bilateral retinal vasculities which again consistant with findings of Saurabh K et al [1], they get 61.4% bilateral among 70 cases of retinal vasculitis in India. Saxena et al [9] also found bilateral involvement in most (71.94%) of the cases, Ali A et al. [10] found most of the cases were bilateral in their series of 56 patients. 70 to 80% of patients develop bilateral but asymitrical disease3.
In Saurabh K et al [1] clinical report most of the patients (78.6%) were from West Bengal. The Patient showed different clinical features at different stages and need different types of management at different stages.
Blurring of the vision was the most common symptom, that we have found in 100% of our study cases of retinal vasculitis, which is similar to the findings of Saurabh K et al [1] and Ali A et al [10].
Vascular sheathing is a pathognomic clinical findings of vasculitis retinae.10 The commonest fundus feature we have found in our case series is vascular sheathing (52.94%) followed by vitreitis (41.18%) then vitreous haemorrhage (39.29%). Saurabh K et al [1] Saxena et al [9] Ali A et al [10] and Abraham et a1 [12] found vascular sheathing as the most common sign of retinal vasculitis in their series of 113, 221,101 and 144 eyes respectively.
Saurabh K et al. [1] reported 72.6% vascular sheathing and 23% vitreous haemorrhage of their series of 113 eyes. Abraham et a1 [12] have noted vascular sheathing in 84% and vitreous haemorrhage in 34% of their series of 144 eyes. We get vascular sheathing in lesser number 52.94 % of eyes, and vitreous haemorrhage in greater number 39.29 % of eyes than that of Saurabh K et al. [1] and Abraham et a1. [12]. This indicates the late presentation of our cases. We get vitreitis (41.18%) more common than vitreous haemorrhage (39.29%) in our series which is consistant with findings of Saurabh K and his coworker [1].
This series also showed 1(5.88%) eye presented with BRVO and 1 1(5.88%) eye presented with CRVO (Table 9). Again 2(11.76%) eye presented with NVG which was devastating, but the eyes presented with CRVO&BRVO did not develop NVG, while Abu El-Asrar AM et al. [11] reported 2 cases of vasculities resembling CRVO developed NVG. Saurabh K et al. [1] found 30% mantoux test positive while we did not get any single positive case in 11 patients, probably due to small series of cases. Corticosteroid is the main stay of treatment in stage I and II vasculitis retinae [1, 3, 11].
Rosen and co-workers [13] reported retinal vasculitis with strongly positive Mantoux test was treated with systemic steroid. All our cases had received corticosteroid both topically and systemically. Five eyes of three of our patients get oral methotraxate because of poor response to corticosteroids,4.3% of Saurabh K et al. [1] series also received immunosuppressive.
Laser photocoagulation was used for retinal neovascularization and to the fibrovascular proliferations [1,9] Panretinal or sectoral scatter photocoagulation is the mainstay of treatment in the stage III ( proliferative stage) of vasculitis retinae [3]. This modalities was also found found beneficial in proliferative stage of vasculities retinae by Das TP and his associates [14]. Regression of retinal neovascularization, neovascular fronds have been observed in 89 % and 80% of cases, respectively [3, 14]. In this series 23.50% eyes get sectoral laser and 29.40% eyes received Pan Retinal Photocoagulation(PRP) which is quite higher than 27.1% of series reported by Saurabh K et al. 47.1% of eyes received intra vitreal injection of anti VEGF , again much more than 1.4% of reported series by Saurabh K et al. [1].
Pars plana vitrectomy is indicated in stage IV vasculities like unresolving vitreous haemorrhage [1], tractional retinal detachment involving the posterior pole,fibro vascular membranes with or without tractional retinal detachment, and combined tractional and rhegmatogenous retinal detachment [3] Only one eye (5.88%) of our series needed pars plana vitrectomy surgery (Table 10).
This medical record based retrospective study had some limitations like small number of participants, missing of informations in medical records. Again this study could not provide the prevalence of etiology of retinal vasculitis. But this present study provides first data on clinical profile of retinal vasculitis in our country.
Conclusion
Retinal vasculitis is a rare but sight threatening condition that has pathognomic identifiable clinical features. A thorough clinical work up is a mandatory for appropriate management which ensured a good outcome of this disease. As the condition is more common in this segment of the world, a further larger population-based study is needed to know the prevalence of the disease along it’s etiology in our country.
Acknowledgment
This work was supported by Researcher Md. Askander Hossan Wasim, Ms. Rahnoma Tarannom.
Financial Disclosure
None reported.
Support
Dr. Ahmadur Rahman Research Centre.
References
- Saurabh K, Das RR, Biswas J, Kumar A (2011) Profile of retinal vasculitis in a tertiary eye care center in Eastern India. Indian J Ophthalmol 59: 297–301.
- Walton RC, Ashmore ED (2003) Retinal vasculitis. Curr Opin Ophthalmol 14:413-419.
- Das T, Biswas J, Kumar A, Nagpal PN, Namperumalsamy P, et al. (1994) Eales' disease. Indian J Ophthalmol 42: 3-18.
- Rosenbaum JT, Jennifer Ku, Amro Ali, Choi D, Suhler EB (2012) Patients with Retinal Vasculitis Rarely Suffer from Systemic Vasculitis. Semin Arthritis Rheum 41: 859–865.
- Ku JH, Ali A, Suhler EB, Choi D, Rosenbaum JT (2012) Characteristics and visual outcome of patients with retinal vasculitis. Arch Ophthalmol 130:1261-1266.
- El-Asrar AA, Al-Kharashi SA (2002) Full panretinal photocoagulation and early vitrectomy improve prognosis of retinal vasculitis associated with tuberculoprotein hypersensitivity (Eales’ disease). Br J Ophthalmol 86:1248-1251.
- Abu El-Asrar AM, Herbort CP, Tabbara KF (2005) Retinal Vasculitis.Ocul Immunol Inflamm 13: 415–433.
- Biswas J, Sharma T, Gopal L, Madhavan HN, Sulochana KN et al. (2002) Eales disease--an update. Surv Ophthalmol 47: 197-214.
- Saxena S, Kumar D (2007) New classification system-based visual outcome in Eales’ disease. Indian J Ophthalmol 55: 267–269.
- Ali A, Ku JH, Suhler EB, Choi D, Rosenbaum JT (2014) The course of retinal vasculitis . Br J Ophthalmol 98 :785-789.
- Abu El-Asrar AM, Al-Obeidan SA, Abdel Gader AGM (2003) Retinal periphlebitis resembling frosted branch angiitis with nonperfused central retinal vein occlusion. Eur Journal Ophthalmol 13: 807-812.
- Abraham C, Baig SM, Badrinath SS (1977) Eales’ disease. Proc All India Ophthalmol Soc 33:226.
- Rosen PH, Spalton DJ, Graham EM (1990) Intraocular tuberculosis. Eye 4:486 -492
- Das TP, Namperumalsamy P (1990) Photocoagulation in Eales' disease. Results of prospective randomised clinical study. Presented in XXVI Int Cong Ophthalmol, Singapore.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi