Case Report, J Clin Exp Oncol Vol: 6 Issue: 7
Successful Treatment of a Progressive Primary Cutaneous Diffuse Large B-Cell Lymphoma of the Leg (PCLBCL-LT) with Hyperthermic Isolated Limb Perfusion
Ioannis Karampinis1, Laura Schwarzwaelder1, Martin Hoffmann2, Timo Gaiser3, Kai Nowak1, Peter Hohenberger1 and Jens Jakob1*
1Division of Surgical Oncology, Department of Surgery, Mannheim University Medical Centre, University of Heidelberg, Germany
2Division of Haematology and Oncology, Klinikum Ludwigshafen, Ludwigshafen, Germany
3Pathological Institute, Mannheim University Medical Centre, University of Heidelberg, Germany
*Corresponding Author : Jens Jakob, MD
Department of Surgery, Mannheim University Medical Centre, University of Heidelberg, Theodor-Kutzer-Ufer 1-3, 68167 Mannheim, Germany
Tel: +49-621-383-2225
E-mail: jens.jakob@umm.de
Received: October 04, 2017 Accepted: October 23, 2017 Published: October 30, 2017
Citation: Karampinis I, Schwarzwaelder L, Hoffmann M, Gaiser T, Nowak K, et al. (2017) Successful Treatment of a Progressive Primary Cutaneous Diffuse Large B-Cell Lymphoma of the Leg (PCLBCL-LT) with Hyperthermic Isolated Limb Perfusion. J Clin Exp Oncol 6:6. doi: 10.4172/2324-9110.1000207
Abstract
Purpose: Hyperthermic isolated limb perfusion (ILP) is a highly effective treatment option for locally advanced soft tissue sarcoma and in-transit metastasized malignant melanoma of the extremities. The role of the hyperthermic isolated limb perfusion in the treatment of aggressive cutaneous b-cell lymphoma (PCLBCL-LT) is unknown.
Methods: This is a case presentation of a 65 year old woman with a multifocal recurrence of a cutaneous b-cell lymphoma of leg type successfully treated by hyperthermic isolated limb perfusion with melphalan. Preoperative regimens included systemic chemotherapy and irradiation.
Results: An isolated limb perfusion was performed (100 mg of melphalan, heating 38.5°, cannulation of the superficial femoral artery). One year after the operation a complete response of the disease could be observed.
Conclusion: Regional treatment by hyperthermic isolated limb perfusion with melphalan does lead to local tumor control in relapsed cutaneous lymphoma of the extremities. Therefore, ILP should be considered as a possible alternative treatment in selected cases of chemotherapy resistant PCLBCL-LT.
Keywords: Hyperthermic isolated limb perfusion; Cutaneous lymphoma;Melphalan; TNF-α
Introduction
Lymphomas are a heterogeneous group of malignant processes of lymphatic origin and are divided into Hodgkin and non-Hodgkin lymphomas. Primary cutaneous lymphomas represent an extranodal manifestation of non-Hodgkin lymphomas. About 25% of them are B-cell derived and are classified into primary cutaneous follicle center lymphoma, primary cutaneous diffuse large B-cell lymphoma of the leg (PCLBCL-LT) and primary cutaneous marginal zone lymphoma [1].
The cutaneous B-cell lymphoma of leg type is an aggressive, rare type of cutaneous B-cell lymphomas which predominantly affects elderly females and is associated with a poor prognosis [2]. The indicated treatment for patients with PCLBCL-LT is Rituximab- CHOP immuno-chemotherapy [1,3]. However, only a small number of patients can achieve a long disease free survival after completion of a chemotherapeutic course and most patients relapse after several months [1]. Radiation can be considered as an additional treatment modality for patients with localized bulky disease who are resistant to chemotherapy [4].
Hyperthermic isolated limb perfusion with recombinant human TNF- α and melphalan is a well-established treatment modality for patients with locally advanced soft tissue sarcoma and in- transit metastasized malignant melanoma of the extremity [5]. During the procedure, the limb is isolated from the circulation; the main artery and vein are cannulated and connected to a cardiopulmonary bypass machine with an oxygenating membrane. After establishment of a stable flow, high dose of chemotheraputic agents can be administered directly to the limb, avoiding systemic toxicity.
Case Presentation
A 65 year old Caucasian woman was first diagnosed on December 2014 with an aggressive primary diffuse large B-cell lymphoma of the leg; stage IV according to the Ann Arbor classification [3]. The first manifestation of the disease was located on the inner side of the left lower extremity. The primary histological examination of a biopsy of the primary described an ulcerated blastic B-cell lymphoma in form of a diffuse, big cell B-cell lymphoma of leg type.
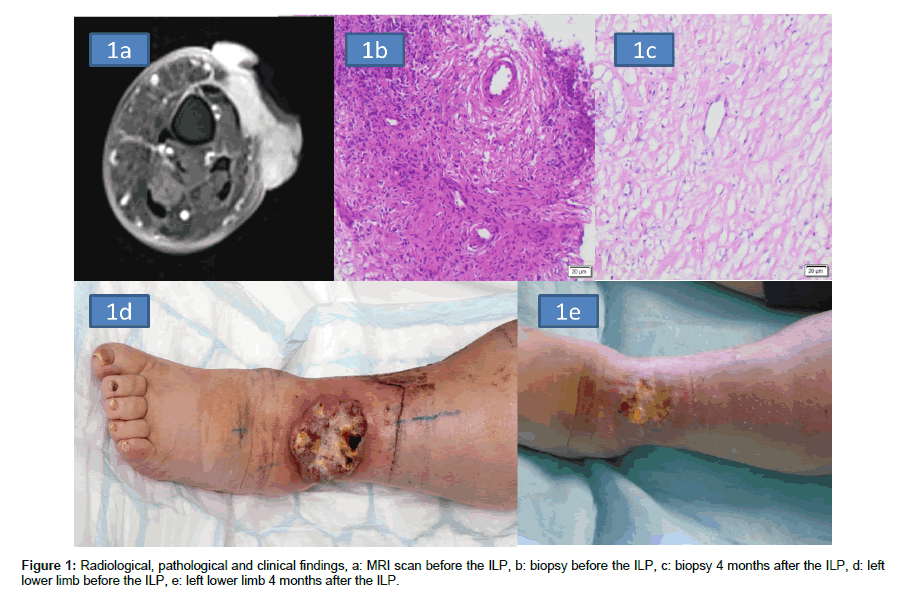
The immune-histological examination revealed b-blasts positive for CD20 and CD79a with a few non neoplastic mature T-cells (CD 3 and CD 5) without CD 5 co-expression, CD 30 was also not positive. The proliferative compartment was almost 90 % (Ki 67, Figure 1a). Staging revealed enlarged lymph inguinal nodes. No biopsy was taken of these.
The treatment history of the patient is listed in Table 1. The patient was initially treated with systemic chemotherapy with prednisolone followed by 3 courses of chemotherapy with rituximab plus cyclophosphamide, doxorubicin, vincristine and prednisolone according to the R-CHOP-14 schema [3]. Restaging after three cycles demonstrated partial remission and chemotherapy was continued. However, Vincristine was stopped because of a chemotherapy induced neuropathy on the fingers. Re-staging revealed a complete remission and the patient received adjuvant involved-field radiotherapy of the lower left extremity. Clinically and on imaging studies no inguinal lymphadenopathy was present at that time.
| Time interval | Treatment | Response | |
|---|---|---|---|
| Primary tumor (diagnosed 12/2014) | 01-05/2015 | Systemic Chemotherapy (6 cycles R-CHOP) |
Complete remission |
| 05-06/2015 | Adjuvant Radiotherapy | Maintenance of CR | |
| Local recurrence | 09/2015 | Restaging | |
| 09-10/2015 | Systemic Chemotherapy (2 courses of DHAOx) |
No response | |
| 10-12/2015 | Systemic hemotherapy with surface RT | No response | |
| 12/2015 | ILP | Complete remission |
Table 1: Treatment history.
Three months later the patient was re-administered to the oncological department with two new exulcerated wounds in the same location as the primary ulcer. Restaging did not demonstrate any other tumor manifestations. After discussing the case in the multidisciplinary team meeting, the patient received a pre-phase treatment with prednisolone followed by 2 courses of rituximab with high dose cytarabine and oxaliplatin according to the DHAOx schema.
The chemotherapy was continued until October 2015. Restaging revealed local progress of the disease (Figure 1b) and again systemic therapy was administered, although with a different regimen (rituximab, ifosfamide, carboplatin and etoposide). The chemotherapy was accompanied by a surface radiotherapy of the left lower extremity. However, local control could not be achieved and the patient suffered from progressing ulcerations (Figure 1c).
On December 2015 the patient was referred to the department of surgical oncology to evaluate the possibility of a surgical therapy. Considering the high malignant potential of the disease as well as the absence of response to systemic chemotherapy and irradiation, we discussed with the patient the possibilities of major amputation or isolated limb perfusion as an alternative, limb-salvage option. The patient refused categorically any mutilating surgery or amputation and agreed to the off label treatment with isolated limb perfusion.
During the operation the femoral artery and vein were accessed through the adductor canal. The vessels were cannulated using two 12 Charriere silicon catheters and were connected to a standard cardiopulmonary bypass machine. After establishment of a stable blood flow of 280 ml/min and exclusion of a relevant leakage we started the heating phase achieving an average temperature of 38.5°C. A cumulative dose of 100 mg melphalan was administered. The limb was perfused for 90 minutes followed by a wash out using hydroxyl ethyl in order to ensure a melphalan free circulation. After catheter removal we performed the vascular repair and the operation was ended. The histological report from a biopsy taken directly after the end of the operation described a diffuse lymphoblastic infiltration of the connective tissue with cytopathological changes (condensed chromatin, small cytoplasma).
After 24 h of monitoring in our intermediate care unit the patient was transferred to the surgical ward. No postoperative complications were observed and no systemic or local toxicity of the ILP was monitored.
The postoperative course was uneventful and the patient could be dismissed 12 days after the operation with slight oedema of the left lower extremity (grade II toxicity according to the Weiberdink classification). No further chemotherapy was performed. Five months after the ILP we performed a re-staging of the disease. No relapse of the disease was observed. The oedema of the leg had receded completely.
In order to evaluate the outcome of the ILP for the lymphoma we performed a clinical follow-up with a new biopsy 4 months after the operation. The histological report revealed tumor-free connective tissue without presence of lymphoblastic cells (Figure 1d).
Macroscopically we could observe an excellent response of the main tumor to the ILP with significant shrinking of the exulcerated area. The other ulcers which were located on the medial site of the lower extremity had completely receded (Figure 1e). After one year free of recurrence the patient developed a local recurrence.
Discussion
Cutaneous B-cell lymphoma of leg type is associated with a poor prognosis since the overall 5 year survival rate of the patients presenting with multifocal disease is 0% and the relapse rates after complete remission are up to 69.4% [2]. Initial response rates to chemotherapy are good but most patients relapse after discontinuation of treatment, or even develop resistance during chemotherapy [3].
Here we report a case of 65 year old woman with a chemotherapy and radiotherapy resistant cutaneous B-cell lymphoma of the left leg that was treated with isolated limb perfusion with melphalan in our department. The patient achieved a complete clinical remission for 1 year after the ILP.
4 cases of treatment of PCLBCL-LT with regional chemotherapy have been reported to date [6-9]. In 3 cases the patients were treated with isolated limb perfusion and in one case with isolated limb infusion.
Jansen was the first to use ILP with melphalan for the treatment of a chemotherapy resistant PCLBCL-LT. His team performed two courses of ILP with an interval of 10 days from each other achieving a disease free survival of 7 months [6].
The second case was reported by Paramo, 15 years later [7]. Using ILP with melphalan they achieved a significant tumor response with tumor necrosis and improvement of the skin lesions. However, the patient developed pathological fractures and could not avoid the amputation. The third case was published two years later from Elhassadi, who used isolated limb infusion with melphalan achieving a notable improvement of the disease with a disease free survival of 6 months [8]. In the last case, the patient was treated with ILP with 120 mg of melphalan accomplishing a complete response for 8 months [9].
Of note, hyperthermic ILP usually includes the administration of rhTNF-α additionally to melphalan if given for locally advanced STS. Considering the strong immune-modulatory action of rhTNF-α and the lack of experience in the treatment PCLBCL-LT we chose not to administer it here.
Conclusion
The review of the existing literature provides adequate clinical evidence that the isolation of the limb from the circulation, the heating and the perfusion with high doses of melphalan can lead to a tumor response with an acceptable morbidity.
Concerning the high malignant potential of the disease and the absence of an effective treatment when chemotherapy and radiotherapy have failed, we recommend the isolated perfusion of the limb as a considerable treatment since it can achieve disease control and is probably better tolerated than a series of systemic multi-agent chemotherapies. Even a phase I/II trial evaluating the toxicity of melphalan based ILP and its preliminary efficacy seems to be worth thinking of.
References
- Wilcox RA (2015) Cutaneous B-cell lymphomas: 2015 update on diagnosis, risk-stratification and management. Am J Hematol 90: 73-76.
- Senff NJ, Hoefnagel JJ, Jansen PM, Vermeer MH, van Baarlen J, et al. (2007) Reclassification of 300 primary cutaneous B-Cell lymphomas according to the new WHO-EORTC classification for cutaneous lymphomas: Comparison with previous classifications and identification of prognostic markers. J Clin Oncol 25: 1581-1587.
- Tilly H, Gomes da Silva M, Vitolo U, Jack A, Meignan M, et al. (2015) Diffuse large B-cell lymphoma (DLBCL): ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 5: v116-125.
- Held G, Murawski N, Ziepert M, Fleckenstein J, Pöschel V, et al. (2014) Role of radiotherapy to bulky disease in elderly patients with aggressive B-cell lymphoma. J Clin Oncol 32: 1112-1118.
- Smith HG, Cartwright J, Wilkinson MJ, Strauss DC, Thomas JM, et al. (2015) Isolated limb perfusion with melphalan and tumour necrosis factor alpha for in-transit melanoma and soft tissue sarcoma. Ann Surg Oncol 3:S356-S3561.
- Jansen RF, van Geel BN, Hagenbeek A, Levendag PC (1989) Intractible cutaneous non-Hodgkin's lymphoma of the lower limb. Complete remission after sequential regional isolated hyperthermic perfusion and perfusion with 1-phenylalanine-mustard (melphalan, L-Pam). Cancer 64: 392-395
- Paramo JC, Benavides C, Tang LW, Martinez A, Cabello-Inchausti B, et al. (2004) Complete remission of previously intractable peripheral cutaneous T-cell lymphoma of the lower extremity using isolated hyperthermic limb perfusion with melphalan (1-phenylalanine mustard). Cancer Invest 22: 545-549.
- Elhassadi E, Egan E, O'sullivan G, Mohamed R (2006) Isolated limb infusion with cytotoxic agent for treatment of localized refractory cutaneous T-cell lymphoma. Clin Lab Haematol 28: 279-281.
- Kobold S, Killic N, Lütkens T, Bokemeyer C, Fiedler W (2010) Isolated limb perfusion with melphalan for the treatment of intractable primary cutaneous diffuse large B-cell lymphoma leg type. Acta Haematol 123: 179-181.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi