Case Report, Int J Ophthalmic Patho Vol: 11 Issue: 6
Surgical Outcome of Maximal Levator Resection in Congenital Ptosis with Poor Levator Function
Rofadun Nisa*
Department of surgery, Government Medical College, Srinagar, Jammu and Kashmir, India
*Corresponding Author: Rofadun Nisa Department of Surgery, Government Medical College, Srinagar, Jammu and Kashmir, India; E-mail: rufaidnisa@gmail.com
Received: 22 October, 2020, Manuscript No. IOPJ-20-21024; Editor assigned: 27 October, 2020, Manuscript No. IOPJ-20-21024 (PQ); Reviewed: 10 November, 2020, QC No. IOPJ-20-21024; Revised: 20 July, 2022, QI No. Q-21024; Manuscript No. IOPJ-20-21024 (R); Published: 17August, 2022; DOI: 10.4172/2324-8599.11.6.113
Citation: Nisa R (2022) Surgical Outcome of Maximal Levator Resection in Congenital Ptosis with Poor Levator Function. Int J Ophthalmic Patho 11:6.
Abstract
Ptosis is defined as an abnormally low-lying upper eyelid margin with eyes in primary position of gaze. Ptosis is considered congenital if present at birth or if it is diagnosed within the first year of life. Congenital ptosis is generally unilateral (70%) but may be bilateral, and can be isolated or associated with disease of one or more of the extra ocular muscles and/or other systemic conditions. More severe forms may involve hypoplasia of the levator palpebrae superioris muscle or tendon with a minimal or absent eyelid crease. The superior branch of the third Cranial Nerve (CN III) is involved in the contraction of the levator palpebrae superioris muscle which is responsible for the elevation of the eyelids. The uncorrected severe ptosis leads to impairment of vision due to deprivational amblyopia
Keywords: Ptosis, Cranial Nerve, Fasenellaservat, Frontalis sling, Conjunctival mullerectomy
Introduction
In congenital myogenic ptosis LPS fibres are dystrophic and replaced by fibrous tissue [1]. Unlike acquired ptosis, congenital ptosis has different key muscle does not relax normally) and the eyelid crease is absent in most cases [2]. The preferred technique for ptosis correction and its outcomes depends on the type of ptosis, LPS function, and the surgeon’s preference. The most common procedures are frontalis sling; levator aponeurosis resection; fasenellaservat; muller’s muscle resection (conjunctival mullerectomy). A prospective study, conducted in the post graduate department of Ophthalmology, SMHS Hospital, Srinagar, which is a tertiary care referral for Kashmir Valley.
Case Presentation
Patients with simple congenital ptosis with poor levator function were diagnosed clinically on the basis of history, old photographs and clinical signs i.e. ptosis, absence of lid crease and defective (poor) levator function. General examination and detailed ocular examination including visual acuity, refraction, dilated fundus examination and SLE were done. The evaluation of ptosis was done by taking lid measurements such as Palpebral Fissure Height (PFH), Marginal Reflex Distance (MRD1), Marginal Reflex Distance 2 (MRD2), Marginal Limbal Distance (MLD), Marginal Crease Distance (MCD) and Levator Function (LF) were done. Levator function was classified by Berke’s Method as:
• Good, if it is 8 mm or more
• Fair, if it is from 5 mm to 7 mm, and
• Poor, if it is 4 mm or less
Ptosis was graded as:
Mild ptosis-drooping of lid 2 mm or less from the normal position.
Moderate ptosis-drooping of lid 3 mm from the normal position.
Severe ptosis-drooping of lid equal to or more than 4 mm from the normal position.
Intra-operatively patients were subjected to maximal levator resection.
Surgical steps of maximal levator resection via skin approach
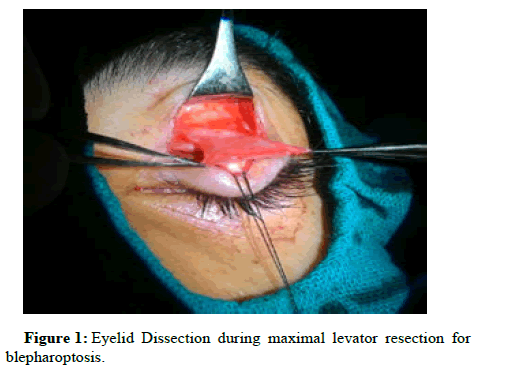
All surgeries were performed under general anesthesia for children and local anaesthesia for adults. An upper eyelid incision was made at either 1mm-2 mm above the cilia line or at the desired crease line when the patient desires a post-operative lid crease. A small strip of skin and orbicularis was excised. An inferior skin and orbicularis muscle flap were dissected from the tarsal plate. The orbital septum was opened and the preaponeurotic fat was identified. The levatoraponeurosisis dissected to above Whitnall’s ligament. Excessive preaponeurotic fat was then excised orshrunk with electro cauterization. The levator aponeurosis and muller muscle were dissected from the superior border of the tarsal plate carefully using a handheld cautery device. The dissection was carried out superiorly along the layer beneath the levator aponeurosis without transecting the medial and lateral horns [3,4]. Central fixation suture at the level of or above Whitnall’s ligament was provisionally inserted from the tarsal plate with a temporary knot to obtain the desired lid level (Figure 1).
The height of the eyelid was adjusted by adaptation of the position of the suture. The medial and lateral sutures were used to create a satisfactory lid contour. The redundant levator complex was excised. The positioning of the upper lid margin was at the superior limbus in patients with general anaesthesia and 1 mm greater than contralateral eyelid height in patients with local anaesthesia. Lid creases were formed by fixing the subcutaneous tissue of the inferior skin flap to the tarsal plate. Three or four interrupted sutures (skin-tarsus and levator muscle-orbicularis-skin) were placed to prevent upper eyelid to prevent upper eyelid entropion. The skin was closed by continuous running suture [5].
Post-operatively patients were assessed for ptosis correction, presence of any complication of visual significance and cosmetic appearance to define success of the surgery. The post-operative correction in amount of blepharoptosis in our study as shown in Table 1 was defined as excellent, good, poor [6-9].
| Surgical Outcome | Unilateral Ptosis | Bilateral Asymmetric Ptosis |
|---|---|---|
| Excellent | MRD1 was ≤ 1 mm compared with the opposite eye | MRD1 was ≥2 mm in each eye and MRD1 was ≤1 mm compared with the opposite eye |
| Good | MRD1 was ≤ 2 mm lower than the opposite eye | MRD1 was ≥1 mm or<2 mm and MRD1 was ≤2 mm lower than the opposite eye |
| Poor | MRD1 was >1 mm(overcorrection)or <2 mm compared with the opposite eye | MRD1 was <1 mm or >1 mm(overcorrection) or MRD1 is >2 mm lower than the opposite eye |
Table 1: The post-operative correction in amount of blepharoptosis in our study.
All complications of blepharoptosis were noted in the form of cosmetic appearance, under correction, over correction, lid crease asymmetry, lidlag, lagophthalmos, entropion, prolapse of the fornix, over correction and exposure keratitis. Patients had a follow up and note was made on every visit at 1st post-operative day, 1 week, 3 week and 3 months regarding the amount of palpebral fissure height obtained marginal reflex distance 1 and the other associated complications [10,11].
Results
In our study 15 eyes of 13 patients had congenital ptosis with poor levator function. Mean age of the patients was 17.3 ± 6.58 (6-25) years. Among the 13 patients, 07 (53.8%) were females and 06 (46.2%) were males indicating no preponderance for any gender. Among the 13 patients, 07 (53.8%) patients had Right sided ptosis, 04 (30.8%) patients had Left sided ptosis and 02 (15.4%) patients had bilateral ptosis. In our study there was a statistically significant difference (p<0.002 and <0.001) in the values of MRD1 and LPSF improving from -0.27 ± 1.53 to 2.8 ± 1.7 mm and from 3.53 ± 0.52 to 7.6 ± 2.995 respectively (Table 2) [12-14].
| Ptosis Measurements | Pre-operative | Post-operative | |||
|---|---|---|---|---|---|
| (At 03 months follow up) | P-value | ||||
| Mean | SD | Mean | SD | ||
| MRD1 (mm) | -0.27 | 1.534 | 2.8 | 1.699 | 0.002* |
| LPSF (mm) | 3.53 | 0.516 | 7.6 | 2.995 | <0.001* |
Table 2: Pre and postoperative Ptosis measurements. Note: *Statistically Significant Difference (P-value<0.05); P-value by paired t-test.
The study also revealed improvement in MLD, MCD and PFH after maximal levator resection. The difference pre and post- operatively was statistically significant. There were only few complications after maximal levator resection [14-16].
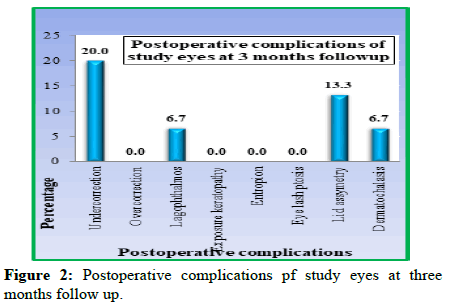
The most common complication was under-correction in 03 (20%) patients, followed by lid asymmetry in 02 (13.3%) patients. Only 01 patient had lagophthalmos and dermatochalasis (6.7%) each (Figure 2).
The prognosis after maximal levator resection was good in our study. It was excellent in 03 (20%), good in 10 (66.7%) and poor in only 02 (13.3%) indicating that Maximal Levator Resection is an excellent procedure for patients of blepharoptosis with poor levator function (Table 3) [17-20].
| Surgical outcome | Frequency | Percentage |
|---|---|---|
| Excellent | 3 | 20 |
| Good | 10 | 66.7 |
| Poor | 2 | 13.3 |
| Total | 15 | 100 |
Table 3: Surgical outcome in study eye safter levator resection.
Discussion
The surgical treatment of choice for patients with unilateral congenital ptosis with poor levator function remains controversial. There are two main procedures: Frontalis suspension operation and maximal levator resection. In general, frontalis suspension operation was regarded as most effective treatment for severe congenital ptosis. For management of congenital ptosis, severity of ptosis, levator function, laterality, associated diseases (blepharophimosis) and surgeon experience should be conside red in the decision. Levator resection is usually performed for patients with fair-to-good levator function more than 4 mm, and frontalis suspension is reserved for patients with poor levator function. Frontalis suspension has frequently been recommended for patients of severe congenital ptosis with poor levatorfunction. In previous studies where frontalis suspension was used for treatment of congenital ptosis with poor levator function, satisfactory outcomes varied from 77.0% to 95.0% and depended on a surgical techniques and materials. Various suspensory materials have been used, which can yield several problems including brow scars. Frontalis suspension using autologous fascia lata requires a harvesting surgery and subjects the patient to donor-site morbidity. Alternative substances are readily available and can shorten operative times, but can also lead to recurrence of ptosis or complications related to allogeneic materials such as infection, graft exposure, rejection and granuloma formation. As an alternative procedure for severe ptosis with poor levator function, maximum levator resection was introduced. Maximum levator resection unlike frontalis suspension, does not introduce any exogenous suspension material into the upper lid, thereby avoiding the risk of infection, extravasation, and extrusion of suspension material. It does not require autogenous fascia lata thereby avoiding the creation of a scar and multiple incision sites, as well as reducing operating time, which is the major concern with young children. In addition, this procedure creates an upper lid crease that produces a more normal appearing upper eyelid. However, the frequent complication of levator resection is under correction (Figure 3).
Conclusion
Maximal Levator resection is an effective alternative procedure to frontalis sling suspension for congenital ptosis in patients with poor levator function. Besides excellent ptosis correction the procedure provides improved cosmesis a more natural lid contour and avoids brow scar. It provides an excellent long term surgical and cosmetic outcome for congenital ptosis with poor levator function as the lagophthalmos in the downgaze has been observed to decrease gradually with time. However, the long-term results of the study can be evaluated by having a larger sample size and longer duration of study keeping in view the low prevalence of blepharoptosis.
References
- Beard C (1981) Types of ptosis. Beard C, editors. In: Ptosis. 3rd ed. St. Louis: Mos by 39-76.
- Sakol PJ, Mannor G, Massaro BM (1999) Congenital and acquired blepharoptosis. Curr Opin Ophthalmol 10: 335–339.
[Crossref] [Google Scholar] [PubMed]
- Smith B, McCord CD, Baylis H (1969) Surgical treatment of blepharoptosis. Am J Ophthalmol 1969: 92–99.
[Crossref] [Google Scholar] [PubMed]
- Gureico JR, Martyn LJ (2007) Congenital Malformation of eye and orbit. Otolaryngol Clinic North Am 40:113-140.
- Von Noorden GK, Maumenee E (1968) Clinical observations on stimulus deprivation amblyopia (amblyopia ex anopsia). Am J Ophthalmol 65: 220–224.
[Crossref] [Google Scholar] [PubMed]
- Baldwin HC, Manners RM (2002) Congenital blepharoptosis: A literature review of the histology of levator palpebrae superioris muscle. Ophthalmic Plast Reconstr Surg 18: 301-307.
[Crossref] [Google Scholar] [PubMed]
- Meyer DR, Rheeman CH (1995) Downgaze eyelid position in patients with blepharoptosis. Ophthalmol 102: 1517-1523.
[Crossref] [Google Scholar] [PubMed]
- Finsterer J (2003) Ptosis: Causes, presentation, and management. Aesthetic Plast Surg 27: 193-204.
[Crossref] [Google Scholar] [PubMed]
- Allard FD, Durairaj VD (2010) Current techniques in surgical correction of congenital ptosis. Middle East Afr J Ophthalmol 17: 129-133.
[Crossref] [Google Scholar] [PubMed]
- Beard C (1966) The surgical treatment of blepharoptosis: A quantitative approach. Trans Am Ophthalmol Soc 64: 401–487.
[Google Scholar] [PubMed]
- Harvey DJ, Iamphongsai S, Gosain AK (2010) Unilateral congenital blepharoptosis repair by anterior levator advancement and resection: An educational review. Plast ReconstrSurg 126: 1325–1231
[Crossref] [Google Scholar] [PubMed]
- Crawford JS (1977) Repair of ptosis using frontalis muscle and fascia lata: A 20-year review. Ophthalmic Surg 8: 31–40.
[Crossref] [Google Scholar] [PubMed]
- Bernardini FP, Cetinkaya A, Zambelli A (2013) Treatment of unilateral congenital ptosis: putting the debate to rest. Curr Opin Ophthalmol 24: 484–487.
[Crossref] [Google Scholar] [PubMed]
- Bernardini FP, Devoto MH, Priolo E (2007) Treatment of unilateral congenital ptosis. Ophthalmol 114: 622–623.
[Crossref] [Google Scholar] [PubMed]
- Deenstra W, Melis P, Kon M (1996) Correction of severe blepharoptosis. Ann Plast Surg 36: 348–353.
[Crossref] [Google Scholar] [PubMed]
- Kersten RC, Bernardini FP, Khouri L (2005) Unilateral frontalis sling for the surgical correction of unilateral poor-function ptosis. Ophthal Plast ReconstrSurg 21: 412–416
[Crossref] [Google Scholar] [PubMed]
- Arajy ZY (2012) Open loop fascial sling for severe congenital blepharoptosis. J Craniomaxillofac Surg 40: 129–133.
[Crossref] [Google Scholar] [PubMed]
- Bagheri A, Ahadi H, Babsharif B (2012) Direct tarsus to frontalis muscle sling without flap creation for correction of blepharoptosis with poor levator function. Orbit 31:48–52.
[Crossref] [Google Scholar] [PubMed]
- Yoon JS, Lee SY (2009) Long-term functional and cosmetic outcomes after frontalis suspension using autogenous fascia lata for pediatric congenital ptosis. Ophthalmology 116: 1405–1414
[Crossref] [Google Scholar] [PubMed]
- Epstein GA, Putterman AM (1984) Super-maximum levator resection for severe unilateral congenital blepharoptosis. Ophthalmic Surg 15:971–979.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi