Research Article, J Pulm Med Vol: 5 Issue: 5
The aging lung face to COVID-19
Rouatbi Sonia1,2,3
1Physiology and functional explorations laboratory, Farhat Hached Hospital, Sousse, Tunisia
2Physiology and functional explorations laboratory, Faculty of Medicine, Sousse, Tunisia
3Research Laboraory of cardiac failure ''LR12SP09
*Corresponding author:
Sonia R,Physiology and functional explorations laboratory, Farhat Hached Hospital, Sousse, Tunisia Physiology and functional explorations laboratory, Faculty of Medicine, Sousse, Tunisia Research Laboraory of cardiac failure ''LR12SP09
Tel. (+216) 97644064
E-mail: Sonia.rouatbi@gmail.com
Abstract
Coronavirus disease 2019 (COVID-19) has so far killed many people; with the majority of deaths occurring in people over the age of 65 years. It has been noted that the severity and outcome of COVID-19 depends in part on the patient’s age. The combination of three factors could explain this ascertainment: the first is linked the lung aging, the second is the associated comorbidities in elderly subjects and the third is the particularities of COVID-19. Here we emphasize the modifications linked to pulmonary aging and their role in worsening the COVID-19 disease.
Keywords: COVID-19, lung aging, pulmonary functions, ACE2, co-morbidities
Introduction
Among COVID-19 patients, elderly patients have a higher mortality rate and symptomatic infection rate. Approximately 80% and 90% of deaths have occurred in patients aged >70 years and ≥60 years in Korea and Italy, respectively (1, 2).
Why is the high mortality of COVID-19 so strongly associated with age? The answer probably lies in the combination of three factors: the first factor is linked to the aging process especially of the lungs (pulmonary aging), the second is linked to associated co morbidities in elderly subjects and the third is linked to the particularities of COVID-19.
Pulmonary aging can be of intrinsic (genetic) or extrinsic (environmental) origin. The lung is the most vulnerable organ to extrinsic aging since it is in direct contact with environmental factors: tobacco, air pollution, occupational exposure. Indeed exposure to cigarette smoke and other environmental stressors over the life span accelerate biologic processes associated with normal aging. In addition, the elderly are often the subject of several chronic diseases (obesity, diabetes, and cardiovascular conditions) which tend to accelerate the general aging of the individual (3-5).
Methods
A literature search, which covered the period 1993 to September 2020, was conducted using the Pubmed and Google. The search strategy had used the following MeSH words: “Spirometry”, “COVID-19”, “ACE2”, “immunosenescence” AND “Aging”. The studies results’ were presented in the context of all other available evidence. Only studies written in English, were included.
Current state of knowledge
There is a progressive, age-associated decrease in lung function, the forced expiratory volume at the first second (FEV1) declines by ~30 mL per year in men and women, whereas the forced vital capacity (FVC) begins to decline later and at a slower rate (20 mL per year) resulting in a decrease in the FEV1/FVC ratio (6).
The losses in volumes and flow rates due to aging are due to structural and functional changes of the lung:the alteration of the elasticity of thoraco-pulmonary tissues,the kyphosis or curvature of the spine, the decrease in the strength of the respiratory muscles, the changes in the pulmonary circulation, the increase in ventilation-perfusion inequality, the reduction in response to hypoxia and to hypercarbia, the immunosenescence which can cause a low-grade systemic inflammation described as inflamm-aging and the regulation of pulmonary receptors expression (beta2 and Angiotensin converting enzyme-2 (ACE2) (Figure 1)(3, 6, 7). All these changes weaken the respiratory system and make it vulnerable to serious infections such as COVID-19 infection.
The decrease in the strength of the respiratory muscles with age is related to changes in skeletal muscle structure including the diaphragm (8). Physical inactivity and smoking exposure of many elderly subjects worsens skeletal muscle dysfunction by aggravating proteolysis and inhibiting protein synthesis, leading to loss of muscle mass (9).
In the study of Zhonghua Shi et al., they provide unique evidence for ACE2 expression in the human diaphragm and severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) viral infiltration in the diaphragm of a subset of COVID-19 patients. In COVID-19 patients, we report increased expression of genes involved in fibrosis and histological evidence for the development of fibrosis in the diaphragm (10).
Age-related changes in the pulmonary circulation result in an increase in pulmonary artery systolic pressure, increased ventilation-perfusion inequality and a progressive decrease in the diffusing capacity for carbon monoxide (DLCO) in elderly. The reduction in DLCO may be due to declines in the alveolar surface area and, possibly, in the density of lung capillaries (11, 12). These changes in pulmonary circulation and alveolar ventilation could explain desaturation in the event of infection by COVID-19.
A reduction in response to hypoxia and to hypercarbia is noted in elderly subjects. The hypoxic ventilatory response is substantially reduced in smokers. So aging when associated to tobacco use leads to a loss of potentially protective mechanisms making elderly subjects more vulnerable to infections with COVID-19 (13).
The immune system also undergoes an aging process termed immunosenescence which can cause an inflamm-aging. Both innate immunity and adaptive immunity are affected by aging. Declining function of innate immune cells with aging also contributes to the dysregulation of the adaptive immune system via molecular cross-talk (14, 15). Humoral immune function also changes significantly with aging. These changes include decreased antibody responses and diminished production of high-affinity antibodies related to defective surface immunoglobulin/B-cell receptor affinity, decreased signaling, and reduced B-cell proliferation. There is also a loss of naïve B-cells and an increase in memory cells with age,resulting in a reduced ability to respond to new antigens (16-18). The COVID-19 pandemic serves as a potent reminder that older people are at very high risk of adverse outcomes from infectious disease because of comorbidities associated with ageing and decreased immunological competence (immunosenescence). Some authors suggest tackling immunosenescence to improve COVID-19 outcomes and vaccine response in older adults (18).
The pulmonary receptors’ expression changes with age. ACE2 was predominantly expressed in alveolar epithelium (alveolar cells type 2), bronchiolar epithelium, endothelium and smooth muscle cells of pulmonary vessels (19). ACE2 expression is dramatically reduced with aging in both genders (20). Sina Booeshaghi and LiorPachter found that the decrease in ACE2 mRNA expression with age in lungs is likely due to two underlying phenomena: a reduction of ACE2 mRNA in ciliated cells, and a shift in ciliated cell abundance with age (21). SARS CoV-2 can infect human target sites through the cellular angiotensin-converting enzyme II (ACE2) receptor in the respiratory tract. ACE2 was recently identified as a functional receptor for COVID-19 and is therefore a prime target for pathogenesis and pharmacological intervention (19). Certain comorbidities (diabetes, chronic obstructive pulmonary disease (COPD), cardiovascular diseases (CVD), hypertension, malignancies, HIV and obesity) are associated with a strong ACE2 receptor expression and higher release of proprotein convertase that enhances the viral entry into the host cells. The comorbidities lead to the COVID-19 patient into a vicious infectious circle of life and are substantially associated with significant morbidity and mortality (22).
In healthy individuals, endothelial cells help to regulate blood pressure, prevent inflammation, and inhibit clotting, in part through the continual production of nitric oxide (NO); they also serve as gatekeepers for molecules passing in and out of the bloodstream. Some elderly patients who have obesity, diabetes, and cardiovascular conditions have compromised endothelial cells. By attacking those cells, COVID-19 infection causes leaking fluids out of the vessels and blood clotting. Those changes spark inflammation throughout the body and fuel the acute respiratory distress syndrome (ARDS) responsible for most patient deaths (Figure 1)(23).
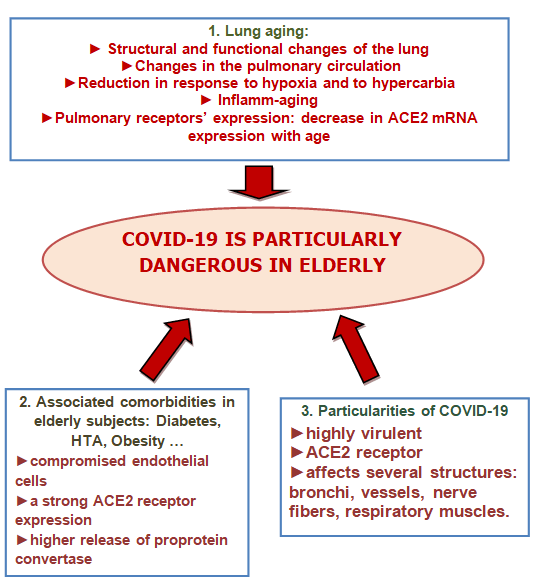
Figure 1: The severity factors of COVID-19 disease in the elderly
Conclusion
These changes related to age may expose elderly subjects to an increased risk of serious infections by COVID-19, decompensation of chronic diseases, addiction and death.
References
- Guan WJ, Ni ZY, Hu Y, et al., for the China Medical Treatment Expert Group for COVID-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382:1708-1720.
- COVID-19 Surveillance Group. Characteristics of COVID-19 patients dying in Italy: report based on available data on March 20th, 2020. Rome, Italy: InstitutoSuperiore Di Sanita; 2020.
- Guénard H, Rouatbi S. Physiological aspects of the decline of pulmonary function with age. Rev Mal Respir 2004;21(5 Pt 3):8S13-24.
- López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. The Hallmarks of Aging Cell 2013;153(6):1194-217.
- Lepeule J, Litonjua AA, Gasparrini A, Koutrakis P, Sparrow D, Vokonas PS, et al. Lung function association with outdoor temperature and relative humidity and its interaction with air pollution in the elderly. Environ Res 2018;165:110-7.
- Culham EG, Jimenez HA, King CE. Thoracic kyphosis, rib mobility, and lung volumes in normal women and women with osteoporosis. Spine 1994;19(11):1250-5.
- Cho WK, Lee CG& Kim LK. COPD as a Disease of Immunosenescence. Yonsei Med J 2019;60(5):407-13.
- Rouatbi S, Ben Moussa S, Guezguez F, Ben Saad H. Muscle dysfunction in case of active tobacco consumption. Science & Sports 2017; 32(4): e119-e126
- Jackman RW, Kandarian SC. The molecular basis of skeletal muscle atrophy. Am J Physiol Cell Physiol 2004;287(4):C834-843.
- Shi Z., De Vries HJ., Vlaar APJ., Van der Hoeven J., Boon RA., Heunks LA., Ottenheijm CAC., for the Dutch COVID-19 Diaphragm Investigators. Diaphragm Pathology in Critically Ill Patients With COVID-19 and Postmortem Findings From 3 Medical Centers. JAMA Intern Med 2021;181(1):122-124.
- Levin DL, Buxton RB, Spiess JP, Arai T, Balouch J, Hopkins SR. Effects of age on pulmonary perfusion heterogeneity measured by magnetic resonance imaging. J Appl Physiol 2007;102(5):2064-70.
- Rouatbi S, Ouahchi YF, Ben Salah C, Ben Saad H, Harrabi I, Tabka Z, et al. Physiological factors influencing pulmonary capillary volume and membrane diffusion. Rev Mal Respir. 2006;23(3 Pt 1):211-8.
- Lalley PM. The aging respiratory system - Pulmonary structure, function and neural control. Respiratory Physiology & Neurobiology. 2013, 187(3): 199-210.
- Castelo-Branco C, Soveral I. The immune system and aging: a review. GynecolEndocrinol. 2014;30:16-22.
- Baylis D, Bartlett DB, Patel HP, Roberts HC. Understanding how we age: insights into inflammaging. LongevHealthspan. 2013;2:8.
- Solana R, Tarazona R, Gayoso I, Lesur O, Dupuis G, Fulop T. Innate immunosenescence: effect of aging on cells and receptors of the innate immune system in humans. SeminImmunol. 2012;24:331-41.
- Whisler RL, Grants IS. Age-related alterations in the activation and expression of phosphotyrosine kinases and protein kinase C (PKC) among human B cells. Mech Ageing Dev. 1993;71:31-46.
- Cox LS., Bellantuono I., Lord JM., Sapey E., Mannick JB., Partridge L., Gordon AL., Steves CJ., Witham MD. Tackling immunosenescence to improve COVID-19 outcomes and vaccine response in older adults. THE LANCET 2020; 1 (2): E55-E57.
- Gheblawi M., Wang K., Viveiros A., Nguyen Q., Zhong JC., Turner Anthony J., et al. Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System. Circ Res. 2020;126(10):1456-74.
- Xudong X, Junzhu C, Xingxiang W, Furong Z, Yanrong L. Age- and gender-related difference of ACE2 expression in rat lung. Life Sci. 2006;78(19):2166–71.
- Sina Booeshaghi A. & Pachter L. Decrease in ACE2 mRNA expression in aged mouse lung.
- Ejaz H., Alsrhani A., Zafar A., Javed H., Junaid K., E Abdalla A., Abosalif KOA, Ahmed Z., Younas S. COVID-19 and comorbidities: Deleterious impact on infected patients. J Infect Public Health 2020;13(12):1833-1839.
- Del Turco S., Vianello AM., Ragusa R., Caselli C., and Bastaa G. COVID-19 and cardiovascular consequences: Is the endothelial dysfunction the hardest challenge? Thromb Res 2020 ; 196: 143-151.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi 