Research Article, Int J Ophthalmic Pathol Vol: 7 Issue: 1
The Clinical Characteristics, Treatment, and Outcomes of Giant Cell Arteritis are Dependent on Histological Subtype
Salter M, Chacko J, Stanley J, Henry W* and Brown H
Department of Ophthalmology, UAMS, Jones Eye Institute, USA
*Corresponding Author : William Henry BS
Department of Ophthalmology, UAMS, Jones Eye Institute, 4301 West Markham, #523 Little Rock, AR 72205, USA
Tel: 8708344454
E-mail: wahenry@uams.edu
Received: November 06, 2017 Accepted: January 06, 2018 Published: January 13, 2018
Citation: Salter M, Chacko J, Stanley J, Henry W, Brown H (2018) The Clinical Characteristics, Treatment, and Outcomes of Giant Cell Arteritis are Dependent on Histological Subtype. Int J Ophthalmic Pathol 7:1.doi: 10.4172/2324-8599.1000214
Abstract
Objective: To determine the clinical outcomes of the two histopathological patterns considered positive for giant cell arteritis (GCA): active arteritis and healed arteritis. Methods: A retrospective chart review was performed of 22 patients with biopsy-proven GCA. Eleven patients had active arteritis and eleven patients had post-inflammatory alterations consistent with healed arteritis. We sought to compare presenting symptoms, ischemic ocular events, inflammatory markers (erythrocyte sedimentation rate [ESR], C-reactive protein [CRP], and platelet count), relapses, and dosage requirements of long-term steroids between the two groups. Results: 7 of 11 patients with active arteritis had an initial ocular ischemic event while 3 of the 11 patients with healed arteritis had an initial ischemic event to the eye. There was no statistical difference in initial ESR between the two groups, but CRP and platelet counts on initial presentation were statistically higher in the active group (p = 0.0002 and p <0.0001 respectively). Patients with active arteritis on biopsy required higher doses of steroids over a 2-year follow-up compared to the healed group: on average 11 mg/day to 1 mg/day at 1 year (p = 0.0008), and 7 mg/day to 0.5 mg/day at 2 years (p = 0.0208), respectively. During the follow-up period, 2 of the 11 patients in the active group demonstrated a recurrent ischemic event to the eye same or fellow eye while in the healed group there were no recurrent ischemic events. Conclusions: Patients with healed arteritis on pathological examination of temporal artery biopsy appear to have better prognoses and may require less aggressive treatment than those with active inflammation.
Keywords: Giant cell arteritis; Healed arteritis; Temporal arteritis
Introduction
Giant cell arteritis (GCA) can cause sudden and potentially bilateral sequential visual loss in the elderly. Therefore, it is considered a medical emergency in ophthalmology and a significant cause of morbidity in an increasingly aging population. Permanent visual loss has been reported to occur in as high as 15-20% of these patients [1], making early and correct diagnosis critical [2]. Several attempts, such as the American College of Rheumatology (ACR) criteria, have been made to diagnosis GCA without temporal artery biopsy. However, Murchison et al. found that the use of ACR criteria alone could miss up to 25% of GCA diagnoses [3]. Thus, temporal artery biopsy remains the diagnostic gold standard for GCA.
Histopathologically, two patterns are considered diagnostic of giant cell arteritis: those with inflammation of the vessel wall (active arteritis) and those with post-inflammatory alterations (healed arteritis). Positive biopsies, whether active or healed, are treated the same initially with high dose steroids. Few investigators have examined the differences between these two groups and their outcomes with treatment. Borg et al. found patients with healed arteritis had lower erythrocyte sedimentation rates (ESR) and higher hemoglobin levels, theorizing that those with healed arteritis represented a relatively benign subgroup with milder clinical presentation and a good prognosis [4]. Borg et al. suggested that a lower initial dose of prednisone (15 mg/day) may be used for this subgroup compared to the active arteritis subgroup which should begin treatment with an initial dose of prednisone of 40-60 mg/day or higher. Another rheumatology group, Lee et al, found similar results [5]. These studies were reported in the rheumatology literature and were focused on the rheumatologic signs and symptoms of GCA. We were unable to find any studies in the neurologic or ophthalmic literature that looked at visual outcomes between these two subgroups to validate these results.
Long-term, high-dose glucocorticoid treatment is not benign and can result in the development of serious adverse effects including glaucoma, gastritis, osteoporosis, bone avascular necrosis, myopathy, and heightened risk for infection. Adjusting steroid dosage based on histologic subgroup for GCA is a paradigm shift away from the historic approach of treating both groups the same and may result in reduced long-term morbidity from therapy without compromising visual outcomes.
Materials and Methods
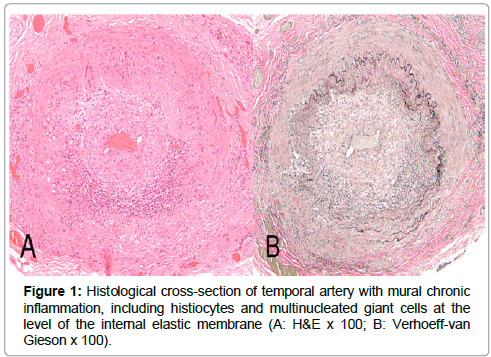
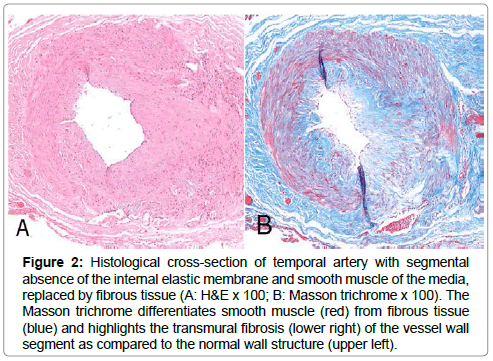
An IRB-approved retrospective review was conducted of all patients with a positive temporal artery biopsy who had visited the Jones Eye Institute of the University of Arkansas for Medical Sciences between February 2004 and February 2013. All patients had presented with clinical signs and symptoms consistent with a diagnosis of GCA. All biopsy specimens were examined and interpreted by a single ocular pathologist (HB). Biopsies were considered positive when either inflammatory components (lymphocytes +/- plasma cells and histiocytes/multinucleated giant cells [active arteritis]) were present within the vessel wall (Figure 1) or there was mural fibrosis +/- neovascularization, with loss of internal elastic membrane and smooth muscle but without an inflammatory cell component present [healed arteritis] (Figure 2).
Figure 2: Histological cross-section of temporal artery with segmental absence of the internal elastic membrane and smooth muscle of the media, replaced by fibrous tissue (A: H&E x 100; B: Masson trichrome x 100). The Masson trichrome differentiates smooth muscle (red) from fibrous tissue (blue) and highlights the transmural fibrosis (lower right) of the vessel wall segment as compared to the normal wall structure (upper left).
These two subgroups were then compared with respect to their clinical characteristics upon presentation to an ophthalmologist. Ischemic events to the eye (ischemic optic neuropathy or retinal artery occlusion) were recorded. Initial laboratory values including ESR, C-reactive protein (CRP), hemoglobin (Hgb), and platelet counts were reviewed in all patients. All patients were treated with steroids and the initial dose (mg/kg), dose at 1 year, and dose at 2 years of follow-up were recorded. Clinical relapses were identified over follow-up visits.
Differences between the subgroups were analyzed with a two sample t-test. P values less than or equal to 0.05 were considered statistically significant.
Results
Twenty-two positive temporal artery biopsies with histopathological characteristics of giant cell arteritis were found: 11 biopsies were found to have active arteritis and 11 biopsies were found to have healed arteritis (Table 1). Of these 22 patients, 20 were women and 2 were men. Mean age was 75 (range 60-91).
| Histological subtype | |||
|---|---|---|---|
| Characteristics | Active | Healed | Total |
| Cases | 11 | 11 | 22 |
| Age | 77 +/- 9 | 72 +/- 8 | 75 +/- 9 |
| Female/Male | 11/0 | 9/2 | 20/2 |
Table 1: Demographics.
Presenting symptoms are shown in Table 2. Five of the 22 patients had a pre-existing diagnosis of polymyalgia rheumatica. The active arteritis group was found to be more symptomatic on initial presentation. Jaw claudication and scalp tenderness were the most prevalent symptoms in the active arteritis group. The most prevalent symptom in the healed arteritis group was headache (Table 2).
| Characteristics | Active | Healed | Total |
|---|---|---|---|
| Temporal Artery/Scalp Tenderness | 8 (73) | 2 (18) | 11 (50) |
| Jaw Claudication | 9 (82) | 2 (18) | 11 (50) |
| Polymyalgia Rheumatica | 3 (27) | 2 (18) | 5 (23) |
| Headache | 8 (73) | 7 (64) | 15 (68) |
| Unintentional Weight Loss (>10 lbs) | 5 (45) | 3 (27) | 8 (36) |
Table 2: Clinical signs/symptoms.
Seven of the 11 patients in the active arteritis group presented with anterior ischemic optic neuropathy (Table 3). Only 3 of the 11 patients with healed arteritis presented with ocular ischemia: 1 with anterior ischemic optic neuropathy, 1 with posterior ischemic optic neuropathy, and 1 with a central retinal artery occlusion.
| Characteristics | Active | Healed | Total |
|---|---|---|---|
| Cases | 11 | 11 | 22 |
| Visual Loss | 7 (64) | 3 (27) | 10 (45) |
| AION | 7 (64) | 1 (09) | 8 (36) |
| PION | 0 (0) | 1 (09) | 1 (09) |
| CRAO | 0 (0) | 1 (09) | 1 (09) |
Table 3: Ocular findings.
There was no statistically significant difference between the average initial ESR values of the two groups (p-value 0.97); however, there was a statistically significant difference between the average initial CRP values of the two groups (p-value 0.0002). The average CRP was 50 mg/dL in the active group and 12 mg/dL in the healed group (Table 4). The average platelet count was also significantly higher in the active group, 401,000 platelets/mcL, compared to the healed group, 249,000 platelets/mcL, (p-value<0.0001).
| Characteristics | Active | Healed | Total |
|---|---|---|---|
| ESR (mm/hr) | 48 +/- 24 | 41 +/- 23 | 45 +/- 23 |
| CRP (mg/dL) | 50 +/- 28 | 12 +/- 9 | 31 +/- 28 |
| Hemoglobin (g/dL) | 12.7 +/- 2.7 | 12.3 +/- 2.0 | 12.5 +/- 2.3 |
| Platelets (1000/mcL) | 401 +/- 76 | 249 +/- 94 | 325 +/- 114 |
Table 4: Laboratory values.
Treatment at presentation, 1 year, and 2 year follow-up are shown in Table 5. The active group required higher doses of steroids at 1 and 2 years of follow-up: average 11 mg/day vs. 1 mg/day at 1 year (p-value 0.0008) and 7 mg/day vs. 0.5 mg/day at 2 years (p-value 0.0208), respectively. Two of the 11 patients in the active group also demonstrated a clinical relapse defined by a subsequent ischemic event to the same or fellow eye during follow-up. In the healed group there were no subsequent ischemic events during the 2 years of follow-up (Table 5).
| Prednisone dosage (mg/day) | |||
|---|---|---|---|
| Characteristics | Active | Healed | Total |
| On presentation | 64 +/- 18 | 54 +/- 15 | 60 +/- 17 |
| At 1 year | 11 +/- 3 | 1 +/- 2 | 7 +/- 6 |
| At 2 years | 7 +/- 3 | 0.5 +/- 1 | 3 +/- 4 |
| Clinical Relapse | 2 (18) | 0 (0) | 2 (9) |
Table 5: Treatment.
Discussion
To our knowledge we are the first ophthalmology investigators to report the differences in clinical outcomes of patients with healed vs. active giant cell arteritis on temporal artery biopsy. Our results are consistent with those in the rheumatology literature [4,5], concluding that the histopathological diagnosis of healed arteritis is a relatively benign subgroup of giant cell arteritis. Borg et al found 4 out of 37 patients (11%) with active arteritis had a recurrence during their 3 year follow-up which is similar to our series, 2 out of 11 patients (18%). There were no healed arteritis patients in the Borg et al group that had a recurrence during follow-up, similar to our study.
In our study, there was no statistical difference in ESR between the healed and active group, but the active group did have statistically higher CRP and platelet count values on presentation. This is consistent with prior reports that both elevated platelet counts and CRP are more sensitive inflammatory markers than ESR [6].
We found over a 2 year follow-up that patients in the healed arteritis group were able to be tapered off of steroids more rapidly than the active arteritis group. The primary indication for tapering steroids was by trending sequential lab values of inflammatory markers (ESR and CRP) while monitoring patients for recurrent GCA symptoms. Currently, the standard of care is to initially treat all patients with positive temporal artery biopsies, whether active or healed, with high dose prednisone (1 mg/kg). Our results suggest that the healed group may be able to be started on lower doses of steroids or tapered more quickly. Our study results may be limited by the retrospective design and the relatively low number of patients. A large prospective clinical trial is needed to validate this hypothesis.
Unlike most other giant cell arteritis studies, our patient population included only subjects with a positive temporal artery biopsy, creating a homogenous study group. A single ocular pathologist (HB) examined and interpreted all biopsies, eliminating inter-observer variability in diagnosis. Also, all biopsies were performed within 2 weeks of starting high dose steroids. There was no significant difference between the active and healed groups with regard to history of PMR which would require chronic low dose prednisone use (Table 2). There were three patients with history of PMR in the active group and two patients in the healed group.
While it is presumed that patients with the healed arteritis pattern had prior episode(s) of active inflammation that had resolved by the time of biopsy, it may be that this histopathological pattern represents a more chronic and indolent underlying pathophysiology. Regardless of the natural history that is occurring on a cellular level, a positive temporal artery biopsy that demonstrates a healed pattern seems to portend a more benign patient clinical course and may not require the same degree of treatment or follow-up as those with active arteritis.
Acknowledgements
This work was supported in part by Research to Prevent Blindness and the Pat & Willard Walker Eye Research Center.
References
- Evans JM, Hunder GG (2000) Polymyalgia rheumatica and giant cell arteritis. Rheum Dis Clin North Am 26: 493-515.
- Aiello PD, Trautmann JC, McPhee TJ, Kunselman AR, Hunder GG (1993) Visual prognosis in giant cell arteritis. Ophthalmology 100: 550-555.
- Murchison AP, Gilbert ME, Bilyk JR, Eagle RC Jr, Pueyo V, et al. (2012) Validity of the American College of Rheumatology Criteria for the Diagnosis of Giant Cell Arteritis. Am J Ophthalmol 154: 617-619.
- Borg EJ, Haanen HC, Seldenrijk CA (2007) Relationship between histological subtypes and clinical characteristics at presentation and outcome in biopsy-proven temporal arteritis. Clin Rheumatol 26: 559-532.
- Lee YC, Padera RF, Noss EH, Fossel AH, Bienfang D, et al. (2012) Clinical Course and Management of a Consecutive Series of Patients with “Healed Temporal Arteritis”. J Rheumatol 39: 295-302.
- Foroozan R, Danesh-Meyer H, Savino PJ, Gamble G, Mekari-Sabbagh ON, et al. (2007) Thrombocytosis in patients with biopsy-proven giant cell arteritis. Ophthalmology 109: 1267-1271.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi