Research Article, J Physiother Rehab Vol: 6 Issue: 5
The Effects of Therapeutic Exercise on Lumbopelvic Pain among Pregnant Women Who Attend Primary Health Centers in Slemani Governorate
Begard Muhammad*
Department of Medical Sciences, American University of Iraq, Sulaymaniyah, Iraq
*Corresponding Author: Begard Muhammad, Department of Medical Sciences, American University of Iraq, Sulaymaniyah, Iraq, Tel: 09647701993036;E-mail: begard.othman@uor.edu.krd
Received date: 16 March, 2022, JPTR-22-57331;
Editor assigned date: 18 March, 2022, PreQC No. JPTR-22-57331 (PQ);
Reviewed date: 01 April, 2022, QC No. JPTR-22-57331;
Revised date: 16 May, 2022, Manuscript No. JPTR-22-57331 (R);
Published date: 23 May, 2022, DOI: 10.4172/Jptr.1000108
Citation: Muhammad B (2022) The Effects of Therapeutic Exercise on Lumbopelvic Pain among Pregnant Women Who Attend Primary Health Centers in Slemani Governorate. J Physiother Rehab 6:5.
Abstract
Background: Pregnancy is one of the enjoyable periods of a woman’s life that turns into an unpleasant experience of common undesirable complications, such as Lumbopelvic Pain (LPP). LPP is one of the common musculoskeletal dysfunctions that occur during pregnancy. The pain tends to increase with advancing pregnancy and negatively affects the quality of life.
Objective: The aim of this study was to investigate the effect of therapeutic exercise on pregnancy-related lumbopelvic pain and daily mobilities.
Methodology: A quasi-experimental research design was conducted on a purposive sample size of 110 pregnant women who had at least minimal pain located on one or more areas around their lumbar or pelvic region and attended primary health care centers. All participants had filled out an informed consent. 50 subjects were admitted into the control group and 60 subjects were admitted into the intervention group. The intervention group has attended a therapeutic exercise course which lasted 12 weeks, including four supervised and individualized sessions per month in a specialized clinic, with continued follow-up at home through phone call for the remaining two months. As instrument, Numeric Rating Scale (NRS) to assess pain intensity, third tool was Modified Pregnancy Mobility Index (MPMI) to assess daily mobility of the pregnant women was used before and after therapeutic exercise course intervention. Statistically, Chi-square test was used for analysed normal distributed data, and Mann-Whitney U test and Wilcoxon Signed Ranks Test were used for those non-normally distributed variables.
Result: The findings illustrated that there were statistically highly significant (P value=<0.001) differences between control to exercise group, after performing therapeutic exercise as intervention, in terms of pain intensity and daily mobility among pregnant women who complain from LPP.
Conclusion: practicing individualized therapeutic exercise that consist of stretching and stability exercise by pregnant women who complain from lumbopelvic pain had a positive effect on reducing pain intensity, as well as promoting physical daily mobility.
Keywords: Therapeutic exercise; Lumbopelvic pain; Pregnancy; Pain intensity; Physical mobility
Introduction
Lumbopelvic Pain (LPP) is one of the most commonly reported complaints among pregnant women which is described as either Low Back Pain (LBP) or Pelvic Girdle Pain (PGP) or a combination of both, that might be happened at the same time [1-7].
Pregnancy-related Lumbopelvic Pain (LPP) is defined as pain in the region of the lower back between the 12th rib and the gluteal fold and/or anterior symphysis pubis and/or posterior region near to sacroiliac joints of the pelvis with or without radiation pain down to the legs [8-10]. Pain and functional disability are main clinical features of LPP during pregnancy [11-14].
Recently, LPP has gained importance because of the negative impact it has on the different aspects of pregnant woman’s regarding health quality and daily functioning [15,16]. In addition, of high prevalence that estimated from 26.5-91%, based on previous studies [17-20].
The exact underlying aetiology of LPP is unknown [21-25]. Several hypotheses have been proposed including hormonal changes cause a laxity within the joints and ligaments in the back and pelvis [26,27], biomechanical and postural alterations in balance occur from an increase in uterine volume, poor joint stability at pelvic region, psychosocial [28-32].
Risk factors are included history of previous LBP maternal weight gain during pregnancy [33-34]. In addition to the level of pre-pregnancy physical fitness.
Different interventions have been used to reduce LPP in general including exercise acupuncture, drugs, and therapies using heat/cold, traction, laser, ultrasound, short wave, massage and corsets [35]. Amongst these cost-effective, non-pharmacological treatments and therapeutic interventions, therapeutic exercise programs combining global strengthening and local pelvic stabilization exercises exhibited positive results [36-38]. Exercise is easily accessible as part of a self-management strategy, can require minimal equipment and can be performed at home [39].
Most of the studies reported that the prevalence average of pregnant women who complain from LPP is nearly 50% [40].
Pregnant women who suffer from LPP experience problems in everyday activities, such as walking, dressing, lifting, carrying, turning in bed, climbing stairs, and sitting [41]. Despite its high prevalence and high affectivity on functional ability, LPP during pregnancy is often considered as a normal unavoidable part of pregnancy, not enough emphasis is placed on its management [42]. Health care professionals typically lack the knowledge on how to successfully treat musculoskeletal pain in pregnant women.
In Kurdistan region/Iraq, according to the researcher experiences, low back and pelvic girdle pain during pregnancy have not been investigated, while there is a noticeable number of complaints, according to what the researcher observed during her visit to antenatal care units. Although, locally there is a lack of information on the prevalence, risk factor, diagnosis, prevention and even management of this condition.
Pregnancy is a sensitive condition and the use of excessive medication should be avoided, thus locally, pregnancy-related LPP needs more studies and more investigation in order to find out what could possibly be done to avoid pain, suffering, and physical disability during pregnancy. In addition, the musculoskeletal treatment based on basic physiotherapy for women’s health problems during pregnancy is one of the major interests of the researcher. There is also a concerning vast gap regarding musculoskeletal dysfunction during pregnancy in local health sectors that requires desperately to be filled.
Aim of the present study aimed to assess the effect of therapeutic exercise on lumbopelvic pain among pregnant women who suffer from lower back pain or pelvic girdle pain or both.
The research hypothesis is practicing therapeutic exercise can cause in decreasing pain intensity and promote daily physical mobility of pregnant women who are complaining from lower back pain or pelvic pain or both in combination lumbopelvic pain.
Materials and Methods
A quasi-experimental research pre/post-test design. The study protocol has been approved by the scientific board of the Nursing College/University of Raparin in April 2020. Although, it was accepted officially from the scientific research unit belonging to the Director of Health (DoH) in the Slimani governorate in September 2020. The present study setting was consisted of two set, “one for collecting samples and others for application of the course”. Official permission was obtained from the Director of Health (DoH) of Slemani governorate, to facilitate accessibility to the Antenatal Care Units (ANC)s within Primary Health Centres (PHC)s.
Antenatal care units are the best resource for obtaining samples. Usually, these units are founded to provide health care services for women during pregnancy and postpartum periods. As application setting for the study, the researcher preferred a private physiotherapy clinic which is belonged to a polyclinic privet hospital at Slemani governorate.
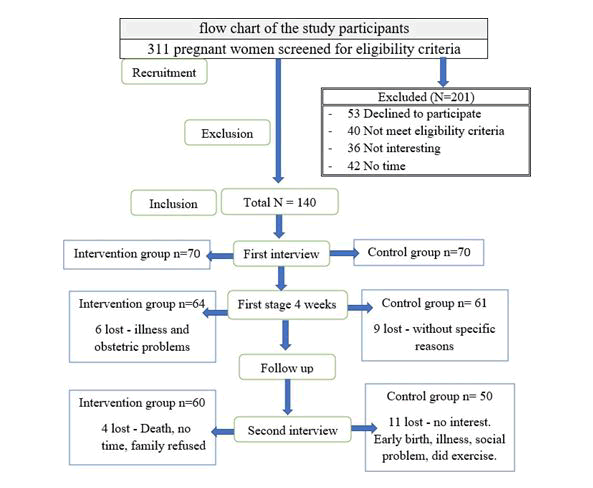
Non-probability purposive sampling was used for recruiting study subjects, the enrolment process started from the end of November 2020 to the end of October 2021. Totally, 311 pregnant women were interviewed through one year, 201 of these women have been excluded and 110 pregnant women with LPP remained with the study. They were randomly split into two groups of intervention (n=60) and control (n=50) randomly. Figure 1 Show the flow chart of sampling.
The study sample was fulfilled the following inclusion criteria; age over 18 years old, singleton pregnancy, gestation age been between 14 and 30 weeks, had lumbopelvic pain means pain at the lower back or pelvic region and with no co-morbidity, finally, not using other methods to treat low back and pelvic pain. Although, those who are contraindicated for exercises according to the ACOG guidelines has been excluded [43]. Particularly, any indications for high-risk pregnancy e.g., placenta previa, pre-eclampsia, previous intrauterine death, previous miscarriage, Thrombophlebitis, decreased fetal movement, amniotic fluid leakage, severe anaemia, history of disc prolapses, spine or pelvic trauma or operation and body mass index greater than 40 or unexplained weight loss.
Ethically, a written formal consent was assigned by each of the participants after explaining the nature and purpose of the study. Study participations are volunteer they were allowed to withdraw from the study without any compensation. Anonymity, privacy, safety, and confidentiality were absolutely assured throughout the study.
The study instruments were designed by the researcher after reviewing the questionnaire from previous study and were validated by expert reviews in a pilot study [44,45]. All participants were required to complete a questionnaire, which was consisted of three parts.
First tool was a demographic characteristic which was consisting in three sections that comprised of; sociodemographic factors include age, residency, education status, employment status, Body Mass Index (BMI). The second section was obstetric history with current pregnancy which included: gravidity, parity, number of abortions and died child, gestational age, history of caesarean section delivery and normal vaginal delivery, intervals between previous pregnancies, and spinal anesthesia; past exercise participation, enrolment in antenatal exercise and admission to antenatal care unit. Last section was history of lumbopelvic pain that included; history of LBP, history of pregnancy-related LBP or pelvic pain and location of the pain on the diagram that adopted from Consulting for LBP or pelvic pain and history of family related to LBP.
The second tools were covered the “Assessment baseline characteristics of Lumbopelvic pain”, that was started with Numeric Rating Scale (NRS), it was adopted from to assess the intensity of LPP [46]. It is the most frequently assessment tool used in the clinical setting with constant scale paces, a straight line with symbols spaced 1 cm distant. It is a subjective assessment tool; the pregnant women had the option to verbally rate their pain intensity as a number or put a circle on the no. Likewise, it is an 11 points scale ranging from 0 (no pain), 1 up to 3 indicated mild pain, 4 up to 6 indicated moderate pain, 7 up to 9 indicated severe pain and 10 indicated the worst pain (unbearable).
In terms of the localization with characters of lumbopelvic pain, the diagram of human body (anterior and posterior) was used to self-report lumbopelvic pain. The LBP was determined if the pregnant women marked a pain area of the 5th lumbar vertebra or above that level. While, the pelvic girdle pain was determined if the pain areas were marked below the level of L5 and the iliac crests (anterior, posterior, and/or lateral view) and those marked both above and below were classified as combined LBP and PGP. In addition, pain onset by gestational age, pain quality, radiation, frequency per day or week, duration, the most severe time of pain, aggravating factors and alleviating factors.
The researcher mainly used two techniques for assessing the presentation and localization of the LPP, to been confirmed and work according to the study’s criteria. The first one was completely depended on the participants’ answer, in finding out their pain location on diagram human body (anterior and posterior) was used to self-report lumbopelvic pain. The second was involved performing “clinical pain provocation tests”. FABER’s test, posterior pelvic pain provocation test (P4 test) and Active Straight Leg Raise (ASLR) test were used for patients with more pain around the sacroiliac joint, and for those with more complaints in symphysis pubis, modifying Trendelenburg test and direct palpation of symphysis pubis test were performed. The pregnant women could include in the study if at least two of the performed tests were positive. In addition, lumbar spine mobility was assessed through active end range movements were performed in flexion, extension, rotation and lateral flexion. A straight leg raising test was applied to exclude nerve-root pain. The hip was excluded as the cause of pain with end range tests of the hip joints in abduction, flexion, internal and external rotation [47]. In general, the evaluation of LPP is typically based on self-administered questionnaires or interviews, and occasionally assessed by clinical evaluation.
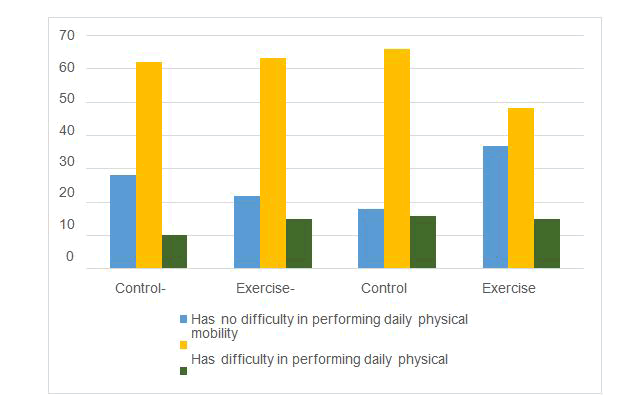
The third tools were named “Modified Pregnancy Mobility Index” (MPMI). It has been created and used in the present study for the first time. Indeed, this instrument has been integrated from three other validated and reliable tools which are pregnancy mobility index, pelvic girdle questionnaire, and oswestry disability index [48,49]. The aim of these instruments is to assess daily physical mobility. These instruments’ variables were not validated to be used as it is consisted in our society. In proportion to the differentiation between both societies (eastern to western) regarding daily mobility behaviour, the researcher adds some other items that are related to daily activities; such as; sweeping floor manually, washing clothes manually, cross-leg sit on the ground at mealtime, and kneeling for prying are the main parts of our daily activities, and omits those which are not applicable such as (travelling by train, travelling by bicycle, walking 500 meters) from PMI-Qs, and (Run and Carry out sporting activities) from PGQs in Figure 2.
Figure 2 this bar chart represents, that there were no significant differences between both groups in terms of the variables in the “Modified Pregnancy Mobility Index” (MPMI) before initiation of the therapeutic exercise course. Obviously, two-thirds of the control and exercise groups had similar difficulty in performing daily physical mobility (62 to 63%) reciprocally. While there were clearly significant differences between both groups after intervention in terms of (no difficulty in performing daily physical mobility), the range of (pre to post) was increased in the exercise group from one-fifths to two-fifths (21 to 36%) but in the control group were decreased from (28 to 18%). In continues, the range of those who (had difficulty in performing daily physical mobility) in the exercise group (pre to post) was declined from (63 to 48%), while reversed elevation were could found (62 to 66%) at the control group, under the column of difficulty in practicing daily activities.
The total number of variables are 39, they were arranged in 10 dimensions of day-to-day activities that include (standing, sitting, walking, carrying, sleeping, self-care, housework, sex life, social life, travelling), each dimension was consist of 1 to 7 variables and their answers scored start from 0 that points to (no problems performing this task), 1 indicates to 25% (some effort performing this task), 2 indicates to 50% (much effort to perform this task), 3 shows 75% (performing this task is possible with aid of others), and 4 that means 100% (impossible to perform this task). It was self-reported, the participants were asked to select one answer for each variable according to the effectiveness of pain, on their daily activity performance. Not applicable (N/A) can put for those activities that never/ever done, such as lifting (10 kg).
The questionnaires were investigated and evaluated for it is consistency and integration by five expertise from different specialty such as (Academic Nurses, Orthopaedic, Obstetrician and gynaecologist, Rheumatologist). Based on their recommendation, modifications were done. Statistically “Cronbach's alpha test” was used in Statistical Package for Social Science (SPSS) version 20, for checking reliability before data collection and the result of “Modified Pregnancy Mobility Index Questionnaire” was 0.845. It indicated highly acceptable. Numeric Rating Scale are usually reliable and valid tools to be used for measuring pain intensity [50,51]. Finally, the validated and reliable questionnaires were used for data collection.
The final confirmation was done through the Pilot study, which was conducted on 10 of the pregnant women who met the incorporation criteria to assess the clarity and appropriateness of these instruments. Based on the discoveries of the pilot study, necessary modifications were done again for adding and rewording a few questions. Pregnant women who enrolled within the pilot study avoided from study to avoid error and bias.
Intervention
The researcher could achieve practical information by reviewing the internationally relevant literature, textbooks, and theoretical knowledge about the various aspects of the musculoskeletal dysfunction during pregnancy, particularly LPP, and the ways of management. Although, the way of delegating instruction to the participants [52,53].
Recruitment process was started from November 2020 to the end October 2021. Nearly 311 pregnant women had been questioned, from those who already complained from LBP. At the first interview, the purpose of the study has been explained, and the informed consent has been received after the eligibility criteria of the pregnant women were assessed. The participants were subsequently randomized, from the first of registration, odd numbers were assigned as exercise group and even numbers as control group. At the commencement 140 participants had been recruited (70) for each of the control and exercise group from the total number (311).
Fifty-three had declined to take part without any reason, forty were not eligible, thirty-six had no interest, forty-two had no time, thirty were lost their follow-up from both groups (20 from control and 10 from exercise) after participating in the study, and involvement in one to two sessions. Therefore, they were dismissed and the reasons were reported that (no time, transportation, had other small child, husband refused, obstetric problem, got COVID-19, death, moved, gave birth before the scheduled follow-up, mobile closed). Lastly, 110 pregnant women were continued to the end, (n=60) at the exercise group and (n=50) at the control group the Figure 1 represents the flow chart of the study participants.
Initial data collection was completed for the control group at the setting of the recruitment which was usually the units of ANC, but for the exercise group was done at the privet physiotherapy clinic. The control participants were normally remained with their basic antenatal care services, without any follow-up or intervention. Simultaneously, they were not discouraged from exercising on their own. While the exercise group were started with intervention program 1 to 7 days after first met, in addition to their basic antenatal care services.
Two hard copy information have been prepared by the researcher; one contains information on the aim of the study, pregnancy-related lumbopelvic pain, cause, risk factors, management that going to be performed in the study course. It was written in the Kurdish language (local language) and offered to the exercise group from the beginning of the course. In order, to gain more confidentiality from the participants and her family, too.
The second one was a coloured booklet prepared by the researcher for the structured, therapeutic exercise course, based on the other literature and textbooks. It was kept underhand as a guideline at the clinic, to avoid distributing information to the control group. The equipment that used during performing the course of therapeutic exercise was consisted of wall mirror, Swiss ball, exercise mat and pillows.
The study course intervention was started from the first week of December 2020 to the end of February 2022. A privet clinical physiotherapy was used as a setting for performing sessions. The course duration was planned for 12 weeks and arranged in two times; First stage; the participants have to be present physically in the clinic for the following four weeks, four sessions enough for adapting exercise correctly. Second stage; the participants have to adhere the program at home as it was performed in the clinic for the next (8 weeks) rest period.
The session was performed by the researcher individually with 1 to 2 pregnant women. The participants were trained well enough in the clinic, through providing instruction, encouragement on performing exercise correctly and repeatedly. They were finished in a complete supervised session. They were asked to repeat them at home, 2 times per day, and to perform each exercise with 10 repetitions. Furthermore, they were followed and encouraged for adherence with the course of the exercise through weekly one phone call for the subsequent 8 weeks.
The session was started with 5-minutes worming up by walking or repeated sit to stand on the chair with who can tolerate her pain. If not, directly, the pregnant woman could start with the positioning that help in stretching and decreasing pain intensity. Then exercise started for 20 to 40 minutes with gentle motion, specifically with who had high pain intensity. The session was ended with 5 minutes relaxation with deep breathings in a resting position. Mostly, the sessions were completed in a positive education atmosphere with considering the principles of adult education [54]. Normally, at each coming session, the participants were evaluated for detecting encountered problems and difficulties.
The therapeutic exercises given to the intervention group were considered the guidelines “Physical Activity and Exercise during Pregnancy and the Post-partum Period” by the Royal College of Obstetricians and Gynecologists (RCOG) [55]. Supine position flat on the bed or floor, body rotations, crossing legs, bending and sudden movement were avoided during performing exercises.
The present study course was consisted of 24 exercises. Totally, can be classified as stability and stretching exercise. Stability exercise for lumbopelvic region through strengthen exercise for (pelvic floor muscle, abdominal muscles, hip abductor, adductor, extensor, external rotation muscles and Quadriceps), in combination with stretching exercise for lower limb flexors (Hamstring, Calf muscle, hip adductors, flexors, and extensors with lower back extensors m.).
All stability and stretching exercises were shown in different positions that reflect various degrees of difficulty. Therefore, the pregnant women selected according to their own endurance and preferences during the course. The researcher specified the exercise plan with each of the participants, making an individual exercise program according to their personal characteristics. At the end of the first stage (4 weeks), each participant was chosen 8 to 10 types of the exercise, this was mean, they fixed their schedule of the program until the end of the course. Performing the exercise program was strongly emphasized and recorded weekly in the women’s personnel file by the researcher, and the participants were asked to record the type and the repetition of the exercise by their personal mobile.
The final assessment of the pregnant women was done at the final week of the course. The duration of the course was depended on the time of their engagement to the study, which was extended from 8 to 12 weeks. Finally, the participants did not have any negative feed-back in regard to the exercise program. In contrast, they mentioned they felt improvement in their others' health complaint, such as (anterior knee pain, incontinence, perineal pain during intercourse, upper back pain).
The pregnant women in the control group were re-assessed through phone call to complete the data collection form, at the same duration as it was performed with the exercise group. Nearly, none of the pregnant women in the control group used medication as painkiller because they were afraid of the harm to their baby.
The data has been collected and analyzed by using the SPSS program (Statistical Package for the social sciences) version 23. Descriptive statistics were performed for all variables of interest. It included mean, standard deviation and minimal and maximal value where appropriate normality of data was checked with Shapiro-Wilk test. Chi-square test was used for analyzed normal distributed data, and Mann-Whitney U test and Wilcoxon Signed Ranks Test were used for those non-normally distributed variables. The p-value is the degree of significance. A significant level value was considered when p-value ≤ 0.05 and a while p-value>0.05 shows non-significant.
Results
The collected data that related to the participants’ characteristics were analyzed by using the chi-square test to get the significant p-value at the Table 1 and Table 2. The groups showed similar baseline characteristics. Clearly, there were no significant differences between the means of the two groups (control to exercise) reciprocally. In terms of age means nearly was (28), gestational age was (23 weeks), BMI before being pregnant mean was (25). As occupation, two-thirds (74%) and (68%) of both groups were housewives, while the majority had a university degree (58%) to (70%). Overall participants’ body weight means in Kg was nearly (70 kg).
| General characteristics | Control (n=50) | Exercise (n=60) | P Value Chi-square | |
|---|---|---|---|---|
| Frequency (%) | Frequency (%) | |||
| Maternal age | 20 to 30 years | 34 (68.0) | 44 (73.3) | 0.419 |
| 31 to 41 years | 16 (32.0) | 16 (26.7 | ||
| Mean (SD) | 27.76 (4.73) | 28.13 (4.76) | ||
| Min to Max | 19 to 38 | 20 to 40 | ||
| Education Level | Primary | 7 (14.0) | 8 (13.3) | 0.366 |
| Secondary | 14 (24.0) | 10 (16.7) | ||
| University | 29 (58.0) | 42 (70.0) | ||
| Maternal Occupation | House Wife | 37 (74.0) | 41 (68.3) | 0.14 |
| Working | 13 (26.0) | 19 (31.7) | ||
| Maternal weight in Kg | 50 to 74 Kg | 28 (56.0) | 34 (56.7) | 0.076 |
| 75 to 100 Kg | 32 (64.0) | 26 (43.3) | ||
| Mean ( ± SD) | 73.6 (11.5) | 71.9 (9.8) | ||
| Min to Max | 51 to 100 | 50 to 91 | ||
| BMI before been pregnant | ˃18.5 | 0 (0.0) | 2 (3.3) | 0.076 |
| 18.5 24.5 | 20 (40.0) | 31 (51.7) | ||
| 25-30 | 27 (54.0) | 23 (38.3) | ||
| 31≤ | 3(6.0) | 4 (6.7) | ||
| Mean (± SD) | 25.4 (3.40) | 24.6 (3.40) | ||
| Min to Max | 18 to 33 | 17 to 33 | ||
| Gestation age | 14-20 Weeks | 16 (32.0) | 20 (33.3) | 0.428 |
| 21-25 Weeks | 16 (32.0) | 17 (28.4) | ||
| 23-30 Weeks | 18 (36.0) | 23 (38.3) | ||
| Mean (± SD) | 23.28 (4.036) | 23.33 (4.61) | ||
| Min to Max | 14 to 30 | 14 to 30 | ||
| Have you done any exercise before being pregnant | Yes | 7 (14.0) | 22 (36.7) | 0 |
| No | 43 (86.0) | 38 (63.3) | ||
| Have you done any exercise before engagement to the present study? | Yes | 2 (4.0) | 2 (3.3) | 0 |
| No | 48 (96.0) | 58 (96.7) | ||
| Other family member who has LBP | None | 15 (30.0) | 18 (30.0) | 0.681 |
| Parent | 7 (14.0) | 9 (15.0) | ||
| Mother | 24 (48.0) | 29 (48.3) | ||
| Father | 4 (8.0) | 4 (6.7) | ||
Table 1: Represent general characteristics of both groups.
| Obstetric history | Control (N=50) | Exercise (N=60) | P Value | |
|---|---|---|---|---|
| Frequency (%) | Frequency (%) | |||
| Gravidity | Primipara | 18 (36.0) | 24 (40.0) | 0.908 |
| Multi and Grand multi | 32 (64.0) | 36 (60.0) | ||
| Mean (± SD) | 2.10 (1.015) | 2.12 (1.290) | ||
| Min to Max | 1 to 4 | 1 to 6 | ||
| Parity | Primipara | 24 (48.0) | 30 (50.0) | 0.292 |
| Multipara | 36 (52.0) | 30 (50.0) | ||
| Mean (± SD) | 0.82 (.919) | 0.75 (.914) | ||
| Min to Max | 0 to 3 | 0 to 4 | ||
| Abortion | None | 37 (74.0) | 45 (75.0) | 0.443 |
| Have abortion | 13 (26.0) | 15 (25.0) | ||
| Mean (± SD) | 0.28 (497) | 0.37 (.712) | ||
| Min to Max | 0 to 2 | 0 to 3 | ||
| No of NVD | None | 32 (64.0) | 43 (71.3) | 0.267 |
| NVD | 18 (34.0) | 17 (28.7) | ||
| No of CS | 0 | 32 (64.0) | 43 (71.7) | 0.302 |
| 1≤ | 18 (36.0) | 17 (28.3) | ||
| Interpregnancy intervals | None | 22 (44.0) | 29 (48.3) | 0.185 |
| 2≥ | 4 (8.0) | 9 (15.0) | ||
| 3≤ | 24(48.0) | 22 (38.7) | ||
| Mean (± SD) | 2.53 (2.875) | 2.19 (2.749) | ||
Table 2: Obstetric history of the participants in both groups.
Table 2 shows obstetric history of the study’s participants, two-thirds (60%) of both groups were multipara and grand multipara. One-third (64 to 71%) of each group at least had one previous cesarean section, as pregnancy intervention more than one-thirds (48 to 38%) had 3 years and more interval with previous pregnancy.
Discussion
The aim of the present study was to investigate the effects of structured, therapeutic exercise, which comprised stretching and stability exercises, on pregnancy-related Lumbopelvic Pain (LPP). The study covers two main aspects of the pregnancy-related LPP. First, it investigated pain intensity with characteristics of the lumbopelvic pain. Second, it measured the performance of daily physical mobility that pain might affect.
To our knowledge, locally, this study is the first effort on pregnancy-related lumbopelvic pain. Therefore, there is a lack of information about prevalence, risk factors, and management of LPP among Kurdish pregnant women. According to the researcher experience during recruiting samples, no pregnant women necessarily consulted physician for her lower back pain. This point can observe clearly when the researcher asked about LPP, then the second questions was “did you consult any health professionals for your LBP?” Two-thirds’ (71.8%) were answered “No” even they did not mention.
The main outcome of the present study was data recorded in term of the characteristics all over participants (110) pregnant women. Two-thirds (61.8%) of both groups were multipara and grand multipara, while multiparity was identified as a risk factor for LPP [56]. As characteristics of lumbopelvic pain More than four-fifths of the pregnant women in both groups were complained from pain around sacroiliac joint, control (96%) and exercise (83%). PGP is the most common diagnosis among pregnant women with lumbopelvic pain, compared to lumbopelvic along or combined LBP and pelvic pain. In addition, pelvic pain commonly has been described as a stabbing or shooting pain the same description had been reported by half of both groups, control (54%) and exercise (51%) (Table 3a) [57].
| Characteristics of pain | Control (n=50) | Exercise (n=60) | P Value* |
|---|---|---|---|
| Quality of the pain | No. (%) | No. (%) | |
| Burning | 4 (8.0) | 2 (3.3) | 0.724 |
| Tightness | 17 (34.0) | 27 (45.0) | |
| Stabbing | 27 (54.0) | 31 (51.7) | |
| numbness | 2 (4.0) | 2 (3.3) | |
| Duration of the pain | |||
| Continue | 6 (12.0) | 13 (21.7) | 0.568 |
| Intermittent | 44 (88.0) | 47 (78.3) | |
| Frequency of the pain | |||
| Not related | 2 (4.0) | 1 (1.7) | 0.699 |
| Weekly | 2 (4.0) | 9 (15.0) | |
| Daily | 46 (92.0) | 50 (83.3) | |
| Most sever time | |||
| No relation | 7 (14.0) | 8 (13.3) | 0.404 |
| Day | 23 (46.0) | 32 (53.3) | |
| Night | 20 (40.0) | 20 (33.3) | |
| Aggravated factors | |||
| Physical activity with weight-bearing | 26 (52.0) | 28 (46.7) | 0.716 |
| Physical activity without weight-bearing | 3 (6.0) | 1 (1.7) | |
| Both in wt. bearing and non-wt. bearing | 21 (42.0) | 31 (51.7) | |
| Alleviating factors | |||
| Rest | 17 (34.0) | 26 (43.3) | 0.527 |
| Special position | 3 (6.0) | 2 (3.3) | |
| Combination (rest and massage) | 30 (60.0) | 32 (53.3) | |
| Source of pain | |||
| Lumbar pain | 1 (2.0) | 4 (6.7) | 0.173 |
| Pelvic girdle pain | 35 (70.0) | 32 (53.3) | |
| Lumbopelvic pain | 14 (28.0) | 24 (40.0) | |
Table 3a: Characteristics of lower back and pelvic pain at both groups before intervention.
Table 3a demonstrates the lumbopelvic pain characteristics in both groups, consequently control to exercise group. There were no significant differences in LPP features among both groups. In percentage, the majority (70 to 53%) of the pregnant women had pain in the pelvic area, nearly more than half of each group (54 to 51%) define their pain quality as stabbing, as duration, their pain was intermittent in four-fifths (88 to 78%). The pain episodes were daily (92 to 83%), as well as, pain severity was increased during the day in both groups (46 to 53%). Weight-bearing activities were considered as the main factor in exaggerating LPP (52 to 43%). While removing factors that were used by most of the participants (60 to 53%) were comprised (bed rest, massage and special position) that helped in decreasing their pain.
Nearly more than half (control 60%) and (exercise 51%) had pain radiation to their thigh, it is one of the LPP symptom, particularly at PGP cases at Table 3b.
| Characteristics of pain | Control (n=50) | Exercise (n=60) | P Value* |
|---|---|---|---|
| Quality of the pain | No. (%) | No. (%) | |
| Burning | 4 (8.0) | 2 (3.3) | 0.724 |
| Tightness | 17 (34.0) | 27 (45.0) | |
| Stabbing | 27 (54.0) | 31 (51.7) | |
| numbness | 2 (4.0) | 2 (3.3) | |
| Duration of the pain | |||
| Continue | 6 (12.0) | 13 (21.7) | 0.568 |
| Intermittent | 44 (88.0) | 47 (78.3) | |
| Frequency of the pain | |||
| Not related | 2 (4.0) | 1 (1.7) | 0.699 |
| Weekly | 2 (4.0) | 9 (15.0) | |
| Daily | 46 (92.0) | 50 (83.3) | |
| Most sever time | |||
| No relation | 7 (14.0) | 8 (13.3) | 0.404 |
| Day | 23 (46.0) | 32 (53.3) | |
| Night | 20 (40.0) | 20 (33.3) | |
| Aggravated factors | |||
| Physical activity with weight-bearing | 26 (52.0) | 28 (46.7) | 0.716 |
| Physical activity without weight-bearing | 3 (6.0) | 1 (1.7) | |
| Both in wt. bearing and non-wt. bearing | 21 (42.0) | 31 (51.7) | |
| Alleviating factors | |||
| Rest | 17 (34.0) | 26 (43.3) | 0.527 |
| Special position | 3 (6.0) | 2 (3.3) | |
| Combination (rest and massage) | 30 (60.0) | 32 (53.3) | |
| Source of pain | |||
| Lumbar pain | 1 (2.0) | 4 (6.7) | 0.173 |
| Pelvic girdle pain | 35 (70.0) | 32 (53.3) | |
| Lumbopelvic pain | 14 (28.0) | 24 (40.0) | |
Table 3b: Pain location and pain radiation assessment for both groups.
Table 3b statistically, Wilcoxon signed rank test used for (P-value). Shows the result of pain assessment according to pain location and pain radiation, which was done by the participants in both groups (control to exercise) reciprocally. It shows four-fifths (96 to 83%) complained from pain around SIJ and two-thirds (60 to 73%) lumbar pain. In addition, of increased radiation nearly more than half (60 to 51%) to the thigh.
The intensity of LPP has been shown to increase with time, both during the day and during the pregnancy course [58]. The present study finding showed that the severity of pain at half (46%) of the control and (53%) of the exercise group was increased at the day, in opposition to what had been discovered by Ozdemir and Mohamed they stated LPP was usually increased at night at. This is might be related to that three-fourths of the control (74%) and exercise (68%) group were housewives and their lifestyle was physically inactive (86% and 67%) reciprocally, before enrolling to the study. In addition, their pain intensity was mainly increased with weight-bearing activities, this was another symptom of LPP or pain from other parts of the pelvic girdle, such as standing, rising and walking, because, frequently regular house holding chores need weight-bearing activities in the Table 4.
| Variables | Control (N=50) | Exercise (N=60) | ||||
|---|---|---|---|---|---|---|
| pre No. (%) | post No. (%) | *p-value | pre No. (%) | post No. (%) | *p-value | |
| No pain 0 | 0 (0.0) | 0 (0.0) | 0.059 | 0 (0.0) | 8 (13.3) | 0 |
| Mild pain 1-4 | 0 (0.0) | 1 (2.0) | 0 (0.0) | 42 (70.0) | ||
| Moderate pain 5-6 | 0 (0.0) | 3 (6.0) | 2 (3.3) | 9 (15.0) | ||
| Severe pain 7-10 | 50 (100.0) | 46 (92.0) | 58 (96.7) | 1 (1.7) | ||
| Total | 50 (100) | 50 (100) | 60 (100) | 60 (100) | ||
Table 4: Represent the result of NRS of both groups in pre/post intervention.
Table 4 indicates the scale and scores of NRS tool which was reported by the participants, before and after intervention. Undoubtedly, shows significantly no differences between pre to post in control group, their pain intensity remained as it was high (severe pain 7 to 10 in 10) at (92%) at the 2nd assessment. In compare with exercise group, at pretest the majority (96%) stated that had (severe pain), while at the termination of the exercise course, two-thirds (70%) were reported (mild pain 1 to 4 in 10). Although, the P-value shows highly significant when the data analyzed by Wilcoxon Signed Ranks Test.
The findings of the present study achieved that an individualized therapeutic exercise program, over 12 weeks, significantly relieved the severity of lumbopelvic pain. Statistically, there were significant differences between the exercise group after the intervention, compared to control, and the (P-value=0.000). As well as significantly the ability of daily mobility at intervention group was promoted and the result was (P-value=0.000), analysed with chi-square test, compared to the control group which was remained with basic antenatal care with no instruction or intervention. This result was confirmed by our study hypothesis in Table 5.
| Variables | Control (N=50) | Exercise (N=60) | *P-value | ||||
|---|---|---|---|---|---|---|---|
| Mean ( ± SD) | Min | Max | Mean ( ± SD) | Min | Max | ||
| The onset of LPP at the present pregnancy in gestational age | 14.02 (2.80) | 6 | 25 | 12.87(6.67) | 6 | 28 | 0.216 |
| Gestational Age at thebeginning of the therapeutic course | 23.28 (4.04) | 14 | 30 | 23.3 (4.62) | 14 | 30 | 0.876 |
| Pre-test of NRS (0-10) of PR-LPP | 8.54 (1.07) | 7 | 10 | 8.78 (1.18) | 6 | 10 | 0.189 |
| Post-test of NRS (0-10) of PR-LPP | 8.34 (1.35) | 4 | 10 | 2.67 (1.80) | 0 | 7 | 0.065 |
| Gestational Age at the end of the therapeutic course | 34.46 (3.11) | 28 | 38 | 34.65(3.21) | 28 | 38 | 0.040 |
Table 5: Represent the differentiation of pain intensity between both groups after intervention
*Wilcoxon signed ranks test
Table 5 illustrates the onset of beginning LPP in both groups were mainly started at the end of the first trimester, mean (SD) control to exercise (14 (2.8) to (13 (6.6)), continue to the end of the second trimester (25 to 28 weeks) in gestation age. The gestational age of both groups at the commencement of the study were (23 (4.0)). Both groups' pain intensity score was analyzed by mean (SD) and minimum to maximum. There was similarity in the pain score before the intervention, in control were (7 to 10) as well as in exercise were (6 to 10). There were fully significant differences between groups after intervention in term NRS (0-10), means (SD) of control to exercise were (8 (1.3)) to (2 (1.8)).
The European guidelines for PGP recommended individual exercise in pregnancy, because supervision with an individualized exercise performance leads to a better quality and positive result in promoting pregnancy-related LPP. Obviously, at the end of the intervention course, pain severity was increased dramatically at the majority (92%) of the control group with advancing their pregnancy, while nearly half (46%) of the exercise group had not stated any pain after intervention in Table 6.
| Variables | Range | No difficulty in performing daily mobility 0-25% | Difficulty in performing daily mobility 25-75% | Impossible to perform daily mobility75-100% | |
|---|---|---|---|---|---|
| Groups | No. % | No. % | No. % | P-value | |
| Standing | Control | 10 (20.0) | 38 (76.0) | 2 (4.0) | 0.000 |
| Exercise | 23 (38.3) | 34 (57.0) | 3 (5.0) | ||
| Sitting | Control | 14 (28.0) | 32 (64.0) | 4 (8.0) | 0.003 |
| Exercise | 27 (45.0) | 27 (45.3) | 6 (10) | ||
| Walking | Control | 7 (24.0) | 39 (68.0) | 4 (8.0) | 0.000 |
| Exercise | 17 (28.4) | 38 (64.0) | 5 (8.3) | ||
| Carrying | Control | 4 (8.0) | 34 (68.0) | 12 (24.0) | 0.000 |
| Exercise | 14 (23.3) | 30 (51.0) | 16 (26.7) | ||
| Sleeping | Control | 4 (8.0) | 39 (78.0) | 7 (14.0) | 0.000 |
| Exercise | 18 (30.0) | 32 (54.7) | 10 (16.7) | ||
| Self-Care | Control | 16 (32.0) | 27 (54.0) | 7 (14.0) | 0.000 |
| Exercise | 31 (51.7) | 22 (38.0) | 7 (11.7) | ||
| House holding Working | Control | 9 (18.0) | 25 (50.0) | 16 (32.0) | 0.000 |
| Exercise | 21 (35.0) | 20 (34.3) | 19 (31.7) | ||
| Sex Life | Control | 8 (16.0) | 41 (82.0) | 1 (2.0) | 0.000 |
| Exercise | 20 (33.0) | 35 (59.0) | 5 (8.0) | ||
| Social life | Control | 7 (14.0) | 41 (82.0) | 2 (4.0) | 0.021 |
| Exercise | 25 (41.7) | 35 (59.7) | 0 (0.0) | ||
| Traveling | Control | 10 (20.0) | 21 (42.0) | 19 (38.0) | 0.000 |
| Exercise | 19 (31.7) | 18 (31.0) | 23 (38.4) |
Table 6: Shows the differentiation of both groups (exercise n=60 and control n=50) after intervention in term of Modified Pregnancy Mobility Index.
Table 6 demonstrates the level of difficulty in performing daily mobility depending on the tool “modified pregnancy mobility index” that had been used in both groups after intervention. Statistically most of the result show significance as (p-value ≤ 0.005) was analyzed by chi-square test. Observed, there are slightly significant differences after intervention in the exercise group compared to the control. In the exercise group, one-thirds had got difficulty in performing (self-care 38%, House-holding work 34%, and traveling 31%), while half of the control group (54%, 50%, 42%) were faced difficulty. On the other hand, the highest 82% struggling in performing (sex life and social life) were found in the control group. Although the highest percentage in performing physical mobility without any problems was observed in (self-care 51%, Sitting 45%, social-life 41%) of the exercise group after intervention.
There were works of literature that confirmed the positive effects of exercises on pain intensity and physical mobility for LPP pregnant women, similar to the present study. While there were others on the conflicted side.
The result of the present study is in agreement with the result that conducted by Garshasbi and Faghih Zadeh. They investigated the effect of exercise during pregnancy on the intensity of low back pain and spine mobility [59]. They included 212 Iranian women during their second trimester until the 37th of the pregnancy. The exercise program was performed three times per week for 12 weeks of intervention. The program was included 15 exercises for abdominal and hamstring muscles and for increasing flexibility of iliopsoas and paravertebral muscles. The control group received only standard antenatal care. In conclusion, they reported a significant reduction in low back pain among the exercise group, while there was increased LBP in the control group (p˂0.0001).
In South Africa, a Randomized Controlled Trial (RCT) conducted by Kluge et al. Investigated the effect of strengthening and stretching exercises on the pain intensity of women with pregnancy-related low back pain [60]. The 10-week intervention was divided into 3 stages to enable the difficulty of the exercises to increase progressively. There were significant differences in pain intensity and functional ability scores between the groups at the end of the study (p˂0.01 and p=0.03, respectively). Although, our study program was included 24 exercises that were arranged from more easily perform to some advance. In order to prepare the participant’s body flexibility and capability in performing an exercise, to keep their adherence with the program and being motivated when they found their quality in performance. We concluded this from their answer to the question “have you done any exercise while you are pregnant? Most of the participants (control 94% and exercise 96%) were answered “No”. It proved that physically they were not active before being pregnant and before their recruitment to the study.
Conventionally, exercise during pregnancy is not a preferable recommendation, not by pregnant women and neither by her family. Therefore, the program was scheduled to be 4 weeks in the clinic with supervision and 8 weeks follow up at home.
Contrary to findings of the present study, Stafne, et al. a randomized control trial to investigate the effect of aerobic and strengthening exercises on lumbopelvic pain. Data collection was done at inclusion (18–22 weeks of pregnancy) and at follow-up (32–36 weeks of pregnancy) [61]. Women in the intervention group received a standardized exercise program. Intervention (n=396) and control (365) pregnant women. Training sessions of 60 minutes in groups of 8–15 women instructed by a physiotherapist were offered once a week over 12 weeks. They concluded that regular exercise during pregnancy had no effect on the prevalence of lumbopelvic pain. No differences between groups regarding disability, pain intensity, or fear-avoidance beliefs were found unadjusted or adjusted for the baseline value of the outcome measure. In an investigation comprising 105 pregnant females aged on average 30.7 ± 4.0 years, Haakstad et al. Concluded that a 60-minute fitness program performed twice a week achieves a non-significant reduction of back pain and pelvic girdle pain.
In relation to the management of lumbopelvic pain during pregnancy, these findings were in accordance with a Turkish study conducted by Ozdemir, which investigated 96 pregnant women who had Low Back and Pelvic Pain (LBPP). It was (RCT), their program consisted of education sessions on how could prevent pregnant women from LBPP and exercise (stretching and tightening) for the large muscles from the neck to the spine, and walking, for the intervention group. The program was scheduled as (30 minutes) 3 sessions per week in 4 weeks duration; they used practical demonstrations and illustrated booklets. The result statistically was significant (P=0.001), pain intensity was decreased, and functional status was promoted for the intervention group. The current study was a likeness in an association of providing information to the participants about their physiological changes during pregnancy, risk factors, and prevention techniques from recurrent LPP through given instruction on performing correct body posture and body mechanics in their daily activities, through demonstration at the clinic under supervision by the researcher.
Another RCT from Croatia conducted by Kokic, et al. investigated the effects of a structured, individualized, supervised therapeutic exercise programme which combines aerobic, resistance, and stretching exercises with daily vigorous walks on pregnancy-related lumbopelvic pain. A total number was 42 pregnant women, 20 for experimental and 22 for control. The upper limit for inclusion was set at 30 weeks of gestation to allow the minimum exercise period of 6 weeks. The duration of the exercise session was 50-55 minutes, twice a week. All exercise sessions were performed in the private physiotherapy practice. The results clearly confirm the positive effects of the exercise programmes on pain intensity (P=0.017), less disability, and symptoms (P=0.005) in the experimental group. Participants in the control group received only standard antenatal care.
In Egyptian Quasi-experimental research that was conducted on 70 pregnant women with lumbopelvic pain practicing sitting pelvic tilt exercise, it was start with educational session to learn how to do the exercise through educational video and Arabic brochure. Participants were instructed to do it at home 2-3 times per day, with 10 repetitions for two consecutives. They reported a positive effect on decreasing the intensity of lumbopelvic pain during pregnancy. There were highly statistically significant differences between the intensity of lumbopelvic pain at the end of the intervention (P<0.001).
As pregnancy-related LPP is a preventable consequence of pregnancy, pregnant women should not have to accept living with this pain [62]. According to the present study result, tailored an individualized physical therapy (stretching and stabilizing) exercise could lead to diminish lumbopelvic pain intensity with moderately to fully promoted physical daily mobility during pregnancy.
Physiologically and anatomically, the pelvic function is sustained by a combination of specific bone features (form closure) and the compression generated by muscles and ligaments (force closure). The biomechanics and postural changes that naturally happen during pregnancy, when the center of gravity is moved anteriorly. In addition, there is a hormonal induced relaxation of the pelvic joints to prepare for delivery. The increased mobility may lead to higher demands on stabilizing ligaments and muscles. When the demand is not met, pain may follow. Therefore, stability exercises were chosen with the aim of strengthening muscle groups and reestablishing stability for the lumbopelvic region. This can help women to handle these changes better, sustain good physical condition, and develop endurance in performing daily activities with less suffering.
At the time of conducting the present study, two-thirds (60%) of the participants were gestational age between 14th to 25th week. This is to means that the study intervention was mainly started in the middle of the pregnancy duration. Almost, changes have been started as weight gain and body posture. Therefore, for preventing musculoskeletal dysfunction, such as LPP, pregnant women better start earlier with stability, strength, and flexibility exercises. At the first interview, when the presence of LPP have been confirmed. Slightly more than half (60 to 53%) of the participants in both groups were used bed rest and massage to control their pain intensity. While being inactive leads to deconditioning and weakening of muscles, which predisposes to loss of function and experience more pain. There is evidence for an association between reduced muscle function and development of LPP in pregnant women. A cross-cultural myth still exists that pregnant women should be inactive and rest in order to protect the safety of the fetus. Despite the agreement among health professionals that healthy pregnant woman should be encouraged to exercise and have an active lifestyle. Pregnant women are often met with confusing and contradictory recommendations from their healthcare providers [63].
Our study recommended that early intervention, including a consultation with a specialist physiotherapist focusing on ergonomics and exercise instructions, can prevent or manage pregnancy-related LPP, as a short-term goal, and avoid chronicity as a long-term goal. Because who knows why two-thirds (60%) of the participants’ mothers had a history of LBP! The possibility of chronicity is more suspected since one in 10 can have pain up to 12 years postpartum, especially those with a history of pregnancy-related LPP [64-69].
Conclusion
In conclusion, the first symptom that makes pregnant women searching for treatment is pain among who are suffering from LPP. Pregnancy-related LPP has moderate to severe effect on daily mobility. Earlier intervention, individualized therapeutic exercise could help in decreasing pain intensity and physical capability.
Limitation of the study
Working with pregnant women is challenging because it is a sensitive stage as a health issue. This challenge will become greater if this work will be invasion to the pregnant women’s lifestyle. Exercise is not a part of our culture and is not recommended by obstetricians. Since the participants of the exercise group in this study, they might have been more interested in an active and healthy lifestyle.
The main limitation was participants’ adherence to home exercise that was not under researcher control. However, home-based exercise can save time and money. The other problem was their absenteeism to the sessions. To make sure and provide encouragement of doing the exercises regularly and completely, women were followed by weekly phone calls. Another limitation was the researcher could not provide participants with a booklet that contain all exercises, because there wasn’t guarantee of not spreading out to the control group, and this is usually might be happened while strong relationship is our cultural feature. Therefore, some subjects were stayed more in the clinic for practicing the exercise correctly. There was difficulty in the client's transportation to the clinic. Finally, the pandemic of COVID-19 which was produced a great barrier in the process of sampling and continuity of the practical sessions. Therefore, these kinds of research require a specific fund.
Future research should investigate the prevalence and risk factors among Kurdish pregnant women who complain from lumbopelvic pain. In order to combine local information with international and work on establishing specific protocol of management.
References
- Wu WH, Meijer OG, Uegaki K, Mens JM, van Dieen JH, et al. (2004) Pregnancy-related pelvic girdle pain (PPP), I: terminology, clinical presentation, and prevalence. Eur Spine J 1:575-589.
[Google Scholar] [Crossref] [Indexed]
- Vleeming A, Albert HB, Östgaard HC, Sturesson B, Stuge B (2008) European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J 17:794-819.
- Mens JMA, Huis in’t Veld YH, Pool-Goudzwaard A (2012) Severity of signs and symptoms in lumbopelvic pain during pregnancy. Man Ther 17:175–179.
- Stomp-van den Berg SG, Hendriksen IJ, Bruinvels DJ, Twisk JW, van Mechelen W, et al. (2012) Predictors for postpartum pelvic girdle pain in working women: the Mom Work cohort study. Pain 153:2370-2379.
[Google Scholar] [Crossref] [Indexed]
- Starzec M, Truszczyńska A (2017) Pregnancy-related lumbopelvic pain-treatment modalities. Postepy Rehabilitacji 31:69-78.
- Tavares P, Barrett J, Hogg-Johnson S, Ho S, Corso M, et al. (2020) Prevalence of low back pain, pelvic girdle pain, and combination pain in a postpartum Ontario population. J Obstet Gynaecol Can 42:473-480.
- Daneau C, Abboud J, Marchand AA, Houle M, Pasquier M, (2021) Mechanisms Underlying Lumbopelvic Pain During Pregnancy: A Proposed Model. Front Pain Res, 2:773988.
- Olsson CB, Nilsson-Wikmar L, Grooten WJ (2012) Determinants for lumbopelvic pain 6 months postpartum. Disabil Rehabil 34:416-422.
[Google Scholar] [Crossref] [Indexed]
- Starzec M, Truszczyńska-Baszak A, Tarnowski A, Rongies, W (2019). Pregnancy-related pelvic girdle pain in polish and Norwegian women. J Manipulative Physiol Ther 42:117-124.
- Van de Pol G, de Leeuw JR, van Brummen HJ, Bruinse HW, Heintz AP, et al. (2006) The Pregnancy Mobility Index: a mobility scale during and after pregnancy. Acta Obstet Gynecol Scand 85:786-791.
- Mogren IM (2006) BMI, pain and hyper-mobility are determinants of long-term outcome for women with low back pain and pelvic pain during pregnancy. Eur spine J 15:1093-1102.
[Google Scholar] [Crossref] [Indexed]
- Pennick V, Liddle SD (2013) Interventions for preventing and treating pelvic and back pain in pregnancy. Cochrane Database Syst Rev 8:CD001139.
- Gutke A, Boissonnault J, Brook G, Stuge B (2018) The severity and impact of pelvic girdle pain and low-back pain in pregnancy: a multinational study. J Womens Health 27:510-517.
[Google Scholar] [Crossref] [Indexed]
- Aragão FFD (2019) Pregnancy-related lumbosacral pain. Braz J Pain 2:176-181.
- Gallo-Padilla D, Gallo-Padilla C, Gallo-Vallejo FJ, Gallo-Vallejo JL (2015) Low back pain during pregnancy. Multidisciplinary approach. Semergen, 42:e59-64.
- Rabiee M, Sarchamie N (2018) Low back pain severity and related disability in different trimesters of pregnancy and risk factors. Int J Women's Health Reprod Sci 6:438-443.
- Kumle M, Weiderpass E, Alsaker E, Lund E (2004) Use of hormonal contraceptives and occurrence of pregnancy-related pelvic pain: a prospective cohort study in Norway. BMC pregnancy and childbirth 4:1-7.
[Google Scholar] [Crossref] [Indexed]
- Gjestland K, Owe KM, Eberhard-Gran M (2012) Do pregnant women follow exercise guidelines? Prevalence data among 3482 women, and prediction of low-back pain, pelvic girdle pain and depression. Br J Sports Med 47:515–520.
- Robinson HS, Vøllestad NK, Veierd MB (2014) Clinical course of pelvic girdle pain postpartum–impact of clinical findings in late pregnancy. Man Ther 19:190-196.
- Tseng P (2018) The effectiveness of a multimedia exercise programme among postpartum women with lumbopelvic pain in Taiwan. PhD thesis. University of Bedfordshire.
- Gutke A, Ostgaard HC, Oberg B (2008) Association between muscle function and low back pain in relation to pregnancy. J Rehabil Med 40:304–311.
[Google Scholar] [Crossref] [Indexed]
- Vermani E, Mittal R, Weeks A (2010) Pelvic girdle pain and low back pain in pregnancy: a review. Pain Pract 10:60-71.
- Katonis P, Kampouroglou A, Aggelopoulos A, Kakavelakis K, Lykoudis S, et al. (2011) Pregnancy-related low back pain. Hippokratia 15:205-210.
- Wuytack F, Begley C, Daly D (2020) Risk factors for pregnancy-related pelvic girdle pain: a scoping review. BMC pregnancy and childbirth 20:1-14.
- Forrester M (2003) Low back pain in pregnancy. Acupunct Med 21:36–41.
- Bjelland EK, Eberhard-Gran M, Nielsen CS, Eskild A (2011) Age at menarche and pelvic girdle syndrome in pregnancy: a population study of 74 973 women. BJOG 118:1646– 1652.
- Wang SM, Dezinno P, Maranets I, Berman MR, Caldwell Andrews AA, et al. (2004) Low back pain during pregnancy: prevalence, risk factors, and outcomes. Obstet Gynecol 104:65–70.
- Ho SS, Yu WW, Lao TT, Chow DH, Chung JW, et al. (2009) Effectiveness of maternity support belts in reducing low back pain during pregnancy: a review. J Clin Nurs 18:1523-1532.
- Vleeming A, Vries HJD, Mens JM, Van Wingerden JP (2002) Possible role of the long dorsal sacroiliac ligament in women with peripartum pelvic pain. Acta Obstet Gynecol Scan 81:430-436.
- Chang HY, Lai YH, Jensen MP, Shun SC, Hsiao FH, et al. (2014) Factors associated with low back pain changes during the third trimester of pregnancy. J Adv Nurs 70:1054-1064.
[Google Scholar] [Crossref] [Indexed]
- Fitzgerald CM, Segal N (2015) An Evidence-Based Guide for Clinicians Musculoskeletal health in pregnancy and postpartum. Colleen M, Fitzgerald, Neil A. Segal (eds) Springer Cham. Switzerland p284.
- Sencan S, Ozcan-Eksi EE, Cuce I, Guzel S, Erdem B, et al. (2018) Pregnancy-related low back pain in women in Turkey: prevalence and risk factors. Ann Phys Rehabil Med 61:33-37.
[Google Scholar] [Crossref] [Indexed]
- Shijagurumayum Acharya R, Tveter AT, Grotle M, Khadgi B, Koju R (2019) Cross-cultural adaptation and validation of the Nepali version of the pelvic girdle questionnaire. J Manipulative Physiol Ther 43:257-265.
- Perry M (2013) Low back pain: tackling a common problem. Pract Nurs 24:356–358.
- Kokic IS, Ivanisevic M, Uremovic M, Kokic T, Pisot R, et al. (2017) Effect of therapeutic exercises on pregnancy-related low back pain and pelvic girdle pain: Secondary analysis of a randomized controlled trial. J Rehabil Med 49:251-257.
- Mirmolaei ST, Ansari NN, Mahmoudi M, Ranjbar F (2018) Efficacy of a physical training program on pregnancy related lumbopelvic pain. Int. J Women's Health Reprod 6:161-166. [Googlescholar][Crossref][Indexed]
- Mohamed ASA, Khedr NFH, Elsherbiny EAF (2020) Effect of Practicing Sitting Pelvic Tilt Exercise on the Intensity of Pregnancy-related Lumbopelvic Pain. Int J Nurs Sci 7:121-128.
- Lin CW, Haas M, Maher CG, Machado LA, Van Tulder MW (2011) Cost-effectiveness of guideline-endorsed treatments for low back pain: a systematic review. Eur Spine J 20:1024–1038.
- Haakstad LA, Bø K (2015) Effect of a regular exercise programme on pelvic girdle and low back pain in previously inactive pregnant women: a randomized controlled trial. J Rehabil Med 47: 229–234.
- Belogolovsky I, Katzman W, Christopherson N, Rivera M, Allen DD (2015) The Effectiveness of Exercise in Treatment of Pregnancy-Related Lumbar and Pelvic Girdle Pain. J Womens Health Phys Therap 39:53–64.
- Mota PGF da, Pascoal AGBA, Carita AIAD (2015) Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Man Ther 20:200-205.
[Google Scholar] [Crossref] [Indexed]
- Artal R, O'Toole M (2003) Guidelines of the American College of Obstetricians and Gynecologists for exercise during pregnancy and the postpartum period. Br J Sports Med 37:6-12.
- Ozdemir S, Bebis H, Ortabag T, Acikel C (2015) Evaluation of the efficacy of an exercise program for pregnant women with low back and pelvic pain: a prospective randomized controlled trial. J Adv Nurs 71:1926-1939.
- Marzouk T, Fadel EA (2020) Effect of a Lumbopelvic Belt versus Pelvic Strengthening Exercise on the Level of Pregnancy-Related Low Back Pain. IOSR Nurs Health Sci 9:1–12.
- Jensen MP, McFarland CA (1993) Increasing the reliability and validity of pain intensity measurement in chronic pain patients. Pain 55:195-203.
- Elden H, Ostgaard HC, Fagevik-Olsen M, Ladfors L, Hagberg H (2008) Treatments of pelvic girdle pain in pregnant women: adverse effects of standard treatment, acupuncture and stabilizing exercises on the pregnancy, mother, delivery and the fetus/neonate. BMC Complement Altern Med 8:1–13.
[Google Scholar] [Crossref] [Indexed]
- Fairbank JCT and Pynsent PB (2000) The Oswestry Disability Index. Spine 25:2940-2953.
- Stuge B, Jenssen HK, Grotle M (2017) The pelvic girdle questionnaire: responsiveness and minimal important change in women with pregnancy-related pelvic girdle pain, low back pain, or both. Phys Ther 97:1103-1113.
- Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, et al. (1978) Studies with pain rating scales. Ann Rheum Dis 37:378-381.
[Google Scholar] [Crossref] [Indexed]
- Ferraz MB, Quaresma MR, Aquino LR, Atra E, Tugwell P, et al. (1990) Reliability of pain scales in the assessment of literate and illiterate patients with rheumatoid arthritis. J Rheumatol 17:1022-1024.
- Vleeming A, Mooney V, Stoeckart R (2007) Movemnt, Stability and lumbopelvic pain-Integration of Research and Therapy, 2nd edition, ELSEVIER, London, UK.
- Santos-Rocha R, Santos-Rocha R (2019) Exercise and Sporting Activity during Pregnancy. Evidence-Based Guidelines Rita Santos-Rocha(eds) Springer Cham, Switzerland AG; 2019; p.345.
- Palis AG, Quiros PA (2014) Adult learning principles and presentation pearls. Middle East Afr J Ophthalmol 21:114-122.
[Google Scholar] [Crossref] [Indexed]
- Syed H, Slayman T, Thoma KD (2021) ACOG Committee Opinion No. 804: Physical Activity and Exercise during Pregnancy and the Postpartum Period. Obstet Gynecol 137:375-376.
[Google Scholar] [Crossref] [Indexed]
- Mogren IM, Pohjanen AI (2005) Low back pain and pelvic pain during pregnancy: Prevalence and risk factors. Spine 30:983-991.
[Google Scholar] [Crossref][Indexed]
- Östgaard HC (1996) Assessment and treatment of low back pain in working pregnant women. Semin Perinatol 20:61-69.
- Liddle SD, Pennick V (2015) Interventions for preventing and treating low‐back and pelvic pain during pregnancy. Cochrane Database Syst Rev 9:CD001139.
- Garshasbi A, Zadeh SF (2005) The effect of exercise on the intensity of low back pain in pregnant women. Int J Gynaecol Obstet 88:271-275.
[Google Scholar] [Crossref] [Indexed]
- Kluge J, Hall D, Louw Q, Theron G, Grové D (2011) Specific exercises to treat pregnancy-related low back pain in a South African population. Int J Gynaecol Obstet 113:187-191.
[Google Scholar] [Crossref] [Indexed]
- Stafne SN, Salvesen KA, Romundstad PR, Stuge B, Morkved S(2012) Does regular exercise during pregnancy influence lumbopelvic pain? A randomized controlled trial. Acta Obstet Gynecol Scand 91:552–559.
- Greenwood CJ, Stainton MC (2001) Back pain/discomfort in pregnancy: invisible and forgotten. J Perinat Educ 10:1–12.
[Google Scholar] [Crossref] [Indexed]
- Clarke PE, Gross H (2004) Women’s behaviour, beliefs and information sources about physical exercise in pregnancy. Midwifery 20:133–41.
[Google Scholar] [Crossref] [Indexed]
- Bergstrom C, Persson M, Nergard KA, Mogren I (2017) Prevalence and predictors of persistent pelvic girdle pain 12 years postpartum. BMC Muscoloscelatal Disorders. 2017; 18: 399
- Elden H, Gutke A, Kjellby-Wendt G, Fagevik-Olsen M, Ostgaard HC (2016) Predictors and consequences of long-term pregnancy-related pelvic girdle pain, al longitudinal follow up study. BMC Musculoskelet Disord 17:276.
- Pennick VE, Young G (2017) Interventions for preventing and treating pelvic and back pain in pregnancy. Cochrane Database Syst Rev CD001139.
- Berber MA, Satilmis IG (2020) Characteristics of Low Back Pain in Pregnancy, Risk Factors, and its Effects on Quality of Life. Pain Manag Nurs 21:579-586.
- Clark CJ, Carr EC, Way S (2013) Pregnancy related lumbopelvic pain: Prevalence, persistence, risk factors and management implications. Br J Midwifery 21:323-330.
- Elden H, Ladfors L, Olsen MF, Ostgaard HC, Hagberg H (2005) Effects of acupuncture and stabilizing exercises as adjunct to standard treatment in pregnant women with pelvic girdle pain: randomised single blind controlled trial. BMJ 330(7494):761
- Lee DG (2011) The pelvic girdle: an integration of clinical expertise and research.4th edition, Churchill Livingstone, 448.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi