Review Article, J Trauma Rehabil Vol: 1 Issue: 1
The Need for Pre-Hospital Simulation Training Platforms in Battlefield Medicine
Amber S. Linde*
Medical Simulation and Information Technology Research Program (MSISRP), Maryland, USA
*Corresponding Author : Amber S Linde
Medical Simulation and Information Technology Research Program (MSISRP), 1054 Patchel Street Fort Detrick, Maryland, USA
E-mail: amber.s.linde.civ@mail.mil
Received: February 15, 2018 Accepted: April 20, 2018 Published: April 28, 2018
Citation: Linde AS (2018) The Need for Pre-Hospital Simulation Training Platforms in Battlefield Medicine. J Trauma Rehabil 1:1.
Abstract
Medical evacuation strategies and tactics to provide seamless point of injury/care and en route patient care for wounded war-fighters is a challenge. Having highly trained medical personal that can rapidly and correctly triage patients by determining who requires immediate need of stabilizing interventions from those that do not requires systematic training to implement appropriate treatment intervention. A smart, flexible training platform can allow for the incorporation of a student's experience and skill level and apply it to simulation training in the areas of triage, TCCC, PFC and medical evacuation. The development of a standardized, accessible simulation training platform system can alleviate medical errors and stress levels in medical providers and improve patient rehabilitation.
Keywords: Pre-hospital simulation; Battlefield medicine; Trauma; Casualty evacuation; Medical evacuation system
Introduction
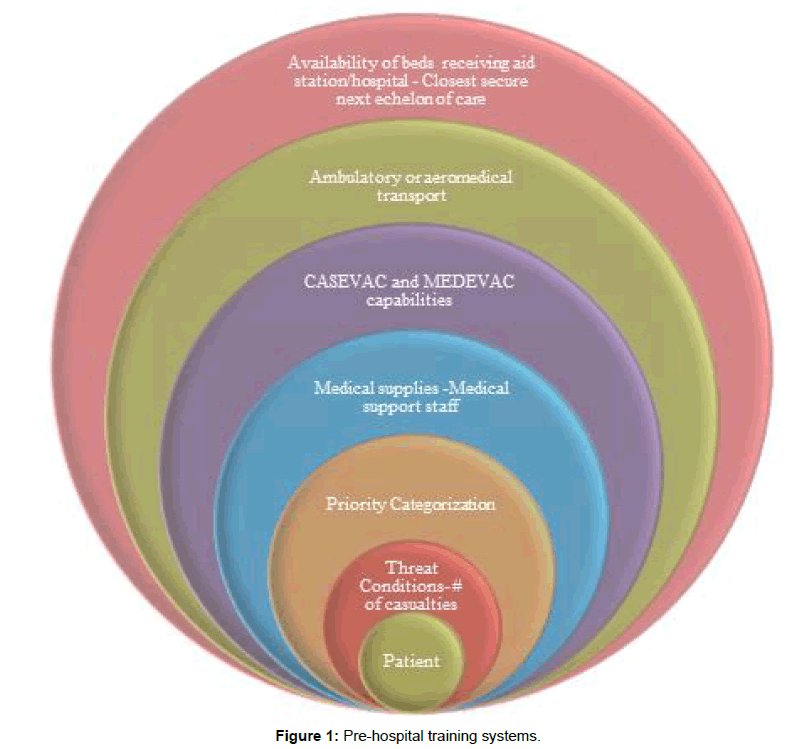
Medical evacuation strategies and tactics to provide seamless point of injury/care and en route patient care for wounded war-fighters is a challenge. Logistical complexities regarding the availability/ quantity of medical supplies and medical personnel (i.e. specialty and experience level of personnel on site); number of patients wounded; and geographical and weather difficulties are just a few examples of barriers to battlefield healthcare that needs to be assessed and executed quickly in order to prevent or reduce the number of warfighters killed in action and died from wounds. The development of a standardized, accessible simulation training platform system can alleviate medical errors and stress levels in medical providers and improve patient outcomes. Having highly trained medical personnel who can rapidly and correctly triage patients by determining who requires immediate need of stabilizing interventions from those that do not is critical. Having those same medical personnel who are able to put into action the appropriate treatment intervention in addition to setting up an evacuation plan is incredibly important to patient survival. The Department of Defense (DoD) faces future wars involving Multi-Domain Battle (MDB) field environments and increases of battlefields that can involve mega-cities increasing the chances of mass casualty events [1]. The MDB describes not so distant future battlefields occurring in the air, land, sea, space, cyberspace, electromagnetic spectrum, military information support operations, physical attack, special technical operations, information assurance, computer network operations and civil-military operations [2]. Providing medical care from pre-hospital through Role 4 is multilayered. It is essential to take a anticipatory measure in considering all known angles of the planned area of deployment of medical personnel to ensure the proper training is available/taken/mastered prior to their arrival. Future conflicts are predicted to have an increase in Prolong Field Care (PFC) situations at the point of injury (POI) and the point of care (POC). Pre-hospital training systems within the platforms must not only be designed to train medical providers by accurately mimicking the situations they will encounter but have the capability of bringing ‘on the job training’ or real-time tele-health mentoring directly to the medical provider that may or may not have medical training beyond providing basic buddy aid. In order to prepare for an increase of PFC medical scenarios, focus will need to be on directed towards providing treatment in a prolonged pre-hospital setting up to 72 h (Figure 1). It is at this first echelon of care, POI and POC, when improvements to training can be made not only to maintain the stabilization of a patient, but to significantly lower the number of preventable deaths while waiting for MEDEVAC (Medical Evacuation System) or CASEVAC (Casualty Evacuation) to arrive [3].
Background
The military MEDEVAC system was established during the Vietnam War when helicopters were used to quickly evacuate patients. The MEDEVAC system remains virtually the same system today [4]. During Desert Shield/Desert Storm it was not uncommon to find inadequate passenger restraints in ground vehicles serving in a CASEVAC capacity. Medical providers also experienced many evacuation attempts hampered by communication deficiencies. This was exacerbated by a lack of a standardized triage system that ultimately limited long range evacuation maneuvers and the ability to transfer multiple casualties to an equipped, medical care facility [5]. Early in the Afghanistan and Iraq War there were already concerns regarding facilities ability to support surgical procedures. Data collected between 2002-2003 described medical operations conducted on patients as ”damage control” operations. In these cases, the patient had to endure multiple operating room procedures because of various limitations of the facility and onsite medical staff. The incidence of hypothermia from blood loss was worsen by conditions in a PFC environment as well prolonged transport in air evacuations in which neither environments had blood products immediately available for patient use [4]. The increase in the number of surgical teams that had a high mobility capability in order to counter longer patient transportation times, regardless if MEDEVAC or CASEVAC was utilized, had been identified and was clearly needed. The research began to focus on MEDEVAC capability gaps to include improving flight medic standards, access to initial and sustainment training, and medical oversight of the air evacuation systems [6,7]. At this stage of the War there was already discussion to improve casualty evacuation, en-route care, and joint operations planning for future evacuation systems [6]. Today, there is still no standardized MEDEVAC system in the US military [4]. At a minimum, military MEDEVACs are provided with one combat medic that has an Emergency Medical Technician (EMT) certification. The civilian MEDEVAC standard procedure includes critical care-trained flight paramedics or trained flight nurses with comparable EMT backgrounds that use standardized patient documentation and validated protocols that include feedback loops for quality improvement processes [6]. The military has an exemplary safety rating for evacuation services as there are typically two pilots and an armory on each flight. The armory adds weight and takes up space which can limit medical equipment that could be used to perform lifesaving procedures during the transport of a critical patient [8].
It is clear that a formal standardized patient care system for the pre-hospital environment is overdue in the US military. The following sections describe pre-hospital outcomes/lessons learned involving studies involving triage, tactical combat casualty care (TCCC), prolong field care and evacuation systems. It also provides recommendations for prehospital point of injury care and evacuation strategies that need to be addressed in the early stage development of the medical simulation training platform.
Triage
On the battlefield there is not a surgeon embedded in the field units. This can be quite a loss of a vital asset given the high occurrences of mass casualties, and compound injuries seen in battle. Another disadvantage of not having a physician on the frontline is that studies have revealed that physicians are better at mass casualty triage compared to other medical providers (nurses and medics) [9]. This is not to suggest that proper triage techniques cannot occur without a physician present; many countries do triage quite well. The advantage to civilian triage compared to military battlefield triage is the civilian triage units have a diverse medical staff and properly equipped medical evacuation vehicles with standardized protocols [10]. Triage of mass casualties is a difficult operation. In 2010, De Jong et al., individuals representing the Joint Services who had knowledge from serving in Afghanistan and Iraq were interviewed. The results of the interviews helped to identify areas of mass casualty systems that needed to be addressed. These needs included mass casualty prioritization; coping with uncertainty; tracking patients in hectic, dangerous environments; optimal usage of available resources; direct and indirect effects of a mass casualty event; and operational procedures of an aid station or hospital under attack [11]. Aside from the Air Force and the Army, the Navy had its own issues when having to develop mass casualty procedures on a ship to include limited resources, personnel, space, and evacuation strategies. As the United States has not recently engaged in a full scale naval battle, there is not current data to suggest how these scenarios will play out. It is essential to use general lessons learned from PFC mass casualty environments in past conflicts in order to plan and execute these scenarios when they occur [12]. Real-world simulations can help in effectively triaging patients for evacuation [13,14].
Tactical Combat Casualty Care
Approximately 20% of all battlefield deaths are hypothetically preventable. Tactical Combat Casualty Care (TCCC) training provided to units has been shown to reduce numbers of preventative deaths [15]. As a result of a US Army Special Operations Command Command-directed casualty response system in the late 1990s requiring all its personnel to have TCCC training as well as to collect data from the pre-hospital trauma registry data to track outcomes, a 2010 study was conducted in which health data from October 1, 2001, through March 31, 2010 was collected from both Afghanistan and Iraq to compare casualties from the 75th Ranger Regiment to casualties from the Services. The results showed a significant decrease in preventable deaths on the battlefield (including numbers of killed in action and died of wounds) to the Command whose members were required to take TCCC [16]. Severe head injury was the most common cause of death in the battlefield and non-battlefield injuries and presently the TCCC does not have a validated treatment plan that addresses traumatic brain injuries [17,18]. Many military medical providers have very little exposure to actual battlefield trauma scenarios and have had far more clinical experience working at sick call and hospital sites. Efforts have been made to provide military medical providers with just in time relevant field trauma refresher training when the individual is given orders to deploy [19]. The access to supplemental combat medical training is not always available nor is it a requirement to take combat medical training programs before being deployed to a potentially hostile location. Although tourniquet use is routine in a combat medical treatment environment, tourniquets are difficult to use and can be applied incorrectly, even for a trained combat medical provider. In the field, it is not uncommon for blast patients to suffer compound injuries and need the application of multiple tourniquets. According to the data collected 2013-2014 Joint Theater Trauma Registry (JTTR), medics tend to perform more circulation hemorrhage control management (43% of the treatments) compared to Medical Officers (24% of the treatments) [18]. Research has yet to develop and commercialize an ideal hemorrhage control dressing even though products are being actively investigated. Needle decompression is a battlefield technique taught in the TCCC curriculum yet even this procedure has had to be reassessed because of the complex nature of blast injuries and the need for at least two skilled medical providers to perform the procedure. Cricothyroidotomy, also taught in the TCCC, is an extremely skilled procedure and, according to the JTTR data, is usually performed by a medical doctor and not in a pre-hospital setting where it may be more advantageous to ensure patient survival [18,20]. TCCC recognizes and provides guidance to medical procedures. Without an accessible training platform that can provide repetitive practice, highly skilled procedures may only be train one time on a procedure. The procedure will not be performed again until the provider is faced with a live scenario under tremendous amounts of stress. Both the terms the “Golden Hour” (transferring a patient in 60 min or less to a medical trauma treatment facility) and the “Platinum Ten Minutes” (ability to assess, initiate treatment and transport the patient within 10 min of a POC) address the urgency of trauma care and the push to eliminate all preventable deaths on the battlefield [21]. In 2006, a protocol known as Damage Control Resuscitation, which changed how blood components were provided to hemorrhaging patients, was implemented [22]. In 2009, air evacuation transport involving trauma injuries occurring on the battlefield was mandated by the Secretary of Defense Robert M. Gates to occur in 60 min or less [23]. Later research revealed that both of the policies showed a decrease in the number of patients killed in action (KIA). However, the Golden Hour requirement did not affect the number of those who died from their wounds [22,23]. It must be noted that the KIA percentage was lower when blood transfusion was provided to the trauma patient during evacuation [23]. Currently, medics are not taught transfusion skills and at a minimum only one medic is required on a MEDVAC. Patient survival numbers could possibly be improved if a standard MEDVAC system was in place and the medic had accesses to the training of using that system. Given the timeline of this data, it is unclear if both mandates working together may have provided an overall decrease in mortality. Further research into efforts including point of injury system of care that can provide transfusion capabilities is compelling. TCCC training does not include a module to train medical providers to take advantage of medical technology or anticipating working with medical technology that use such systems like Unmanned Aerial Vehicles (UAV) that can serve as telehealth mentors or deliver supplies such as blood products. Technology is being developed and as a result, the delivery of blood to a PFC or POC environment for example, will have an element of training complexity [24]. As access to this technology in UAV and robotics mature it will become very important to include technology scenarios in simulated training platforms. Standardizing the process of point of injury, MEDEVAC and CASEVAC scenarios across the Joint Services using TCCC training is an endeavor that will need to be supported by policy implementation in order to provide a dependable method that medical units can ensure a strict adherence to the evidence-based TCCC Guidelines proven to reduce morbidity and mortality on the battlefield [4]. It is difficult to design medical simulation scenarios when an agreed curriculum is not available. Lack of standardization of the foundation of battlefield care affects not only patient outcomes but affects the validity of the health data collected in the field for medical evacuation and POC treatment when medical language and code is not consistent.
Prolong Field Care
PFC is not overlooked in modern warfare. Prior to change in policy mandating medical evacuation be provided in 60 min or less, pre-hospital care was being provided up to 72 h before evacuation vehicles could be provided. After the implementation of this policy, for the majority of units, advanced medical help had become expected and could be set by a timeline [6]. It is the standard consensus that future wars will not have this luxury to advance patient care evacuation services [2]. US Battalion aid stations (mobile facilities integral to combat units) operating during the War in Iraq had high casualty rates. Consequently Battalion aid stations provided high evacuation rates in addition to maintaining a high rate of patient survival. In many of the studies discussing evacuated patient survival, it is unclear if the location of the aid station contributes to the high survival rate. This concept is worth researching as it can provide the groundwork to systematically scope the most advantageous locations for battalion aid stations in situations where PFC conditions will become more common [25]. If the future battlefield will include several dispersed medial aid stations, it is unclear how future battles will track patient data from smaller battalion aid stations to evacuation sites to higher roles of care when faced with a high casualty battlefield. For PFC training scenarios to be successful it is important that data collected from the field can provide the capability to provide accurate guidance to the medical provider of any skill level as to what the next steps will needed to apply the suitable medical care with the supplies that are available. For example, in 2007 MEDEVAC capabilities in southern Afghanistan were audited. Any issues uncovered were expected to be assessed and appropriate measures taken to improve performance. Areas that were reviewed included factors such as distance from a medical site having the proper trauma medical equipment and services, hostile landing sites, information delay, and incorrect patient priority categorization [6]. Advances and incorporation of communication technologies collecting real-time data from PFC locations can determine evacuation availability and the capacity of treatment facilities in the area [26].
Evacuation
Evacuation times of patients are well published in the literature and offer many lessons to be learned. A reoccurring theme from the medical community in order to better the evacuation system is the need for trained staff on the evacuation vehicle. The evacuation vehicle will be outfitted with proper equipment and staff that can interact with well-trained forward medical teams embedded in the military teams that are able to apply relevant POC procedures while waiting for suitable evacuation approaches to be leveraged [27]. As previously discussed, POI, POC and en route medical interventions are multifaceted and involve various skill levels of medical professionals. Treatment of trauma injuries can on many occasions involve numerous medical interventions and patient movement to several Roles of care until a hospital is reached [17,28]. The US military forces are a fighting force and evacuation vehicles are going to be equipped with weapons to conduct the mission; leaving little space available for medical personnel and equipment [29]. This is a fact of military life as well as an unfortunate state of affairs as research shows that the evacuation of a patient that has access to a pre-hospital trauma team will result in better patient health outcomes for the patient [30]. Adding to the complication of the medical evacuation system in war time, the recent conflicts have shown an increase in both military and civilian casualties. Air evacuation system requirements are not prepared for mass casualty events that may include a large number of civilian patients to include geriatric and pediatric casualties. Evacuation strategies will need to be reexamined and revamped before the next conflict [31].
Conclusion
Having highly trained medical personal that can rapidly and correctly triage patients by determining who requires immediate need of stabilizing interventions from those that do not requires systematic training to implement appropriate treatment intervention. In addition, setting up an evacuation plan is incredibly important as the Department of Defense faces future wars involving Multi-Domain Battle (MDB) field environments and increases of battlefields that can involve attacks of mega-cities; increasing the chances of mass casualty events. The MDB describes not so distant future battlefields occurring in the air, land, sea, space, cyberspace, electromagnetic spectrum, military information support operations, physical attack, special technical operations, information assurance, computer network operations and civil-military operations. Future conflicts are predicted to have an increase in Prolong Field Care (PFC) situations at the point of injury and the point of care. Pre-hospital training systems within the platforms must not only be designed to train medical providers by accurately mimicking the situations they will encounter, but have the capability of bringing ‘on the job training’, artificial intelligence technologies, and/or real-time tele-health mentoring directly to the medical provider. In order to prepare for the increase of PFC medical scenarios, focus will need to be on providing treatment in a prolonged pre-hospital setting up to 72 h. It is at this first echelon of care, (POI and POC) where improvements to training can be made in order to not only maintain the stabilization of a patient, but to significantly lower the number of preventable deaths while waiting for MEDEVAC (Medical Evacuation System) or CASEVAC (Casualty Evacuation) to arrive. The development of a smart, flexible training platform can allow for the incorporate a student’s experience and skill level and apply it to simulation training in the areas of triage, PFC and medical evacuation. The future fight will need to include a structured plan of action as to how Military Health System integrates various types of simulation training in order to appropriately and effectively train medical providers. A smart, flexible training platform can allow for the incorporation of a student’s experience and skill level and apply it to simulation training in the areas of triage, TCCC, PFC and medical evacuation. By having real-world training scenarios, it makes simulation exercises far more realistic to reflect encounters. It can also show that what the learner may come to expect will not always go according to plan. This training environment can encourage team work, communication, and foster creative solutions that compliment standardized training to meet mission needs. The mission of simulation training regardless of how it is delivered (VR, AR or task trainers) should not be to “win” but to prepare and provide the student with the knowledge and practical skills that increases the overall success by lowering the occurrences of battlefield mortality and morbidity.
Organization
The Medical Simulation and Information Sciences Research Program (MSISRP) is tasked with planning, coordinating, and overseeing a tri-service science and technology program to improve strategic planning and process development by improving military medical training through medical simulation, educational gaming, and objective training metrics and improving health information sciences through increased interoperability and better health information technology applications [32]. The MSISRP believes that the need for a foundation platform for unlimited access to appropriate point of injury and medical evacuation training is the solution to facilitate the distribution in providing future medical training needs via virtual reality (VR), augmented reality (AR) and manikin technologies that leverage machine learning and artificial intelligence technology.
References
- Grusd E, Kramer-Johansen J, Scand J (2016) Does the Norwegian emergency medical dispatch classification as non-urgent predict no need for pre-hospital medical treatment? An observational study. Trauma Resusc Emerg Med 24: 65.
- United States Army-Marine Corps White Paper (2017) Multi-Domain Battle: Combined Arms for the 21st Century.
- McLeod J, Hodgetts T , Mahoney P (2007) Combat "Category A" calls: evaluating the pre hospital timelines in a military trauma system. J R Army Med Corps 153: 266-268.
- Mabry RL, Apodaca A, Penrod J, Orman JA, Gerhardt RT, et al. (2012) Impact of critical care-trained flight paramedics on casualty survival during helicopter evacuation in the current war in Afghanistan. J Trauma Acute Care Surg 73: S32-S37.
- Beekley AC, Watts DM (2004) Combat trauma experience with the United States Army 102nd Forward Surgical Team in Afghanistan. Am J Surg 187: 652-654.
- Bilski TR, Baker BC, Grove JR, Hinks RP. Harrison MJ, et al. (2003) J Battlefield casualties treated at Camp Rhino, Afghanistan: lessons learned. Trauma 54: 814-821.
- Gerhardt RT, McGhee JS, Cloonan C, Pfaff JA, De Lorenzo RA (2001) U.S. Army MEDEVAC in the new millennium: a medical perspective. Aviat Space Environ Med 72: 659-664.
- De Lorenzo RA (1997) Military and civilian emergency aeromedical services: common goals and different approaches. Aviat Space Environ Med 68: 56-60.
- Janousek, JT, Jackson DE, De Lorenzo RA, Coppola M (1999) Mass casualty triage knowledge of military medical personnel. Mil Med 164: 332-325.
- Raiter Y, Farfel A, Lehavi O, Goren OB, Shamiss A, et al. (2008) Mass casualty incident management, triage, injury distribution of casualties and rate of arrival of casualties at the hospitals: lessons from a suicide bomber attack in downtown Tel Aviv. Emerg Med J 25: 225-229.
- De Jong MJ, Benner R, Benner P, Richard ML, Kenny DJ, et al. (2010 ) Mass casualty care in an expeditionary environment: developing local knowledge and expertise in context. J Trauma Nurs 17: 45-58.
- D Souza E, Wing V, Zouris J, Vickers R, Lawnick M, et al. (2016). Multi-Injury Casualty Stream Simulation in a Shipboard Combat Environment. M. Mil Med 181: 70-75.
- Remick KN, Dickerson JA, Nessen SC, Rush RM, Beilman GJ (2010) Transforming US Army trauma care: an evidence-based review of the trauma literature. US Army Med Dep J 4: 21.
- Pizzola JL (2010) MEDEVAC miscategorization. Mil Med 175: 655-658.
- Deal VT, McDowell D, Benson P, Iddins B, Gluck G, et al. (2010) Direct from the Battlefield: TCCC lessons learned in Iraq and Afghanistan. Spec Oper Med 10: 77-119.
- Kotwal RS, Montgomery HR, Kotwal BM, Champion HR, Butler FK, et al. (2011) Eliminating preventable death on the battlefield. Arch Surg 146: 1350-1358.
- Keene DD, Penn-Barwell JG, Wood PR, Hunt N, Delaney R, et al. (2016) Died of wounds: a mortality review. J R Army Med Corps 162: 355-360.
- Linde AS, Kunkler K, Caridha J (2017) Medical simulation training: targeting medical skills to emulate real-time field injuries. International Conference on Applied Human Factors and Ergonomics, AHFE 2017: Advances in Human Factors in Simulation and Modelling; Book Chapter, Springer 151-161.
- Sohn VY, Miller JP, Koeller CA, Gibson SO, Azarow KS, et al. (2007) From the combat medic to the forward surgical team: the Madigan model for improving trauma readiness of brigade combat teams fighting the Global War on Terror. Jr J Surg Res 138: 25-31.
- Savage E, Forestier C, Withers N, Tien H, Pannell D (2011) Tactical combat casualty care in the Canadian Forces: lessons learned from the Afghan war. Can J Surg 54: S118-S123.
- Committee for Tactical Emergency Casualty Care (2017).
- Olson W (2014) Study: change in transfusion protocol cuts troop death rate. Stars and Stripes.
- Kotwal RS, Howard JT, Orman JA, Tarpey BW, Bailey JA, et al. (2016). The Effect of a Golden Hour Policy on the Morbidity and Mortality of Combat Casualties. JAMA Surg 151: 15-24.
- Wen T, Zhang Z, Wong KK (2016) Multi-Objective Algorithm for Blood Supply via Unmanned Aerial Vehicles to the Wounded in an Emergency Situation. PLoS One 11: e0155176.
- Gerhardt RT, De Lorenzo RA, Oliver J, Holcomb JB, Pfaff JA (2008) Out-of-hospital combat casualty care in the current war in Iraq. Ann Emerg Med 53: 169-174.
- Horne ST, Vassallo J (2015) Triage in the defence medical services. J R Army Med Corps: 161: 90-93.
- Cordell RF, Cooney MS, Beijer D (2008) Audit of the effectiveness of command and control arrangements for medical evacuation of seriously ill or injured casualties in southern Afghanistan 2007. J R Army Med Corps 154: 227-230.
- Maddry JK, Mora AG, Savell S, Reeves LK, Perez CA, et al. (2016) Combat MEDEVAC: A comparison of care by provider type for en route trauma care in theater and 30-day patient outcomes. J Trauma Acute Care Surg 81: S104-S110.
- Bastian ND, Brown D, Fulton LV, Mitchell R, Pollard W, et al. (2013) Analyzing the future of army aeromedical evacuation units and equipment: a mixed methods, requirements-based approach. Mil Med 178: 321-329.
- Clarke JE, Davis PR (2012) Medical evacuation and triage of combat casualties in Helmand Province, Afghanistan. Mil Med 177: 1261-1266.
- Patterson CM, Woodcock T, Mollan IA, Nicol ED, McLoughlin DC (2014) United Kingdom military aeromedical evacuation in the post-9/11 era. Aviat Space Environ Med 85: 1005-1012.
- Medical Simulation and Information Research Sciences Portfolio.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi