Case Report, J Clin Exp Oncol Vol: 7 Issue: 5
Tibial Metastasis from Primary Carcinoma Tongue in a Young Male: A Case Report
Sanjay Kumar M* and Praveen Kumar M
Department of Radiation Oncology, HCG Cancer Center Hubli, Karnataka, India
*Corresponding Author : Sanjay Kumar M
Department of Radiation Oncology, HCG Cancer Center Hubli, Karnataka, India
Tel: +919019960007
E-mail: drsanjayamishra@gmail.com
Received: July 18, 2018 Accepted: August 30, 2018 Published: September 07, 2018
Citation: Kumar SM, Kumar PM (2018) Tibial Metastasis from Primary Carcinoma Tongue in a Young Male- A Case Report. J Clin Exp Oncol 7:5. doi: 10.4172/2324-9110.1000226
Abstract
We report a case of a young male with Carcinoma right lateral border of tongue, cT3N1Mx, post-surgery post adjuvant chemo-radiation. Following a Disease-free interval of 15 months, he developed pain in the left knee region for which he was evaluated with MRI and then biopsy which was conclusive of a Metastatic squamous cell carcinoma from the tongue primary. Workup for the Chest, Abdomen and Pelvis did not show any other metastatic disease. He further underwent palliative radiotherapy for pain at the local site and is being further planned for palliative chemotherapy. In this case report, we discuss the rarity of such presentations, possible high-risk factors, present and future implications in the follow-up of such high-risk cases of Head and Neck Squamous Cell Carcinomas, especially in the younger population.
Keywords: Tibia; Metastasis; Tongue; Radiotherapy; Carcinoma
Case History
We report a case of a 35 year old male from poor socioeconomic background, chronic gutka chewer, who is a known case of Carcinoma of the right lateral border of tongue. He was initially diagnosed in April 2016 with biopsy from non-healing ulcer over the right lateral border of tongue. He was clinically staged as cT3N1Mx. He underwent Partial Glossectomy + Marginal Mandibulectomy + Left Coronoidectomy + Bilateral Supraomohyoid Neck Dissection in April 2016. Post-op Histo-pathological Examination showed moderately differentiated Squamous cell carcinoma, margins free, 1/20 nodes positive for metastasis with extracapsular extension, pT3N1. He received Adjuvant concurrent Chemo-radiation with weekly Cisplatin 50 mg IV and External Beam Radiation therapy using 3dimensional conformal RT technique to a dose of 60 Gy/30 fractions over 6 weeks, which he completed in June 2016. He was on regular 3 monthly follow-up till September 2017 during when he was disease-free.
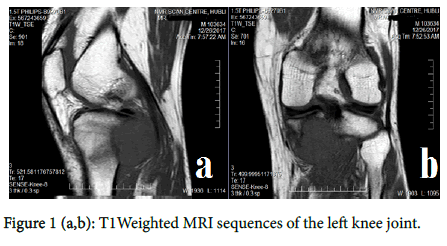
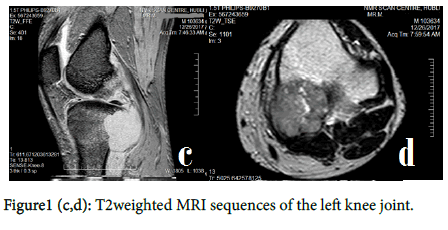
In December 2017, he presented with the complaints of pain in left leg since 2 months. After clinical examination, he was sent for MRI of the left knee joint which showed 4x3.8x3.3cm well defined focal expansile lesion involving the posterior cortex/subcortical aspects of the proximal tibia with associated marrow edema/juxtacortical soft tissue, suggestive of primary/secondary malignant bone neoplasm [Figure 1((a,b,c,d)].
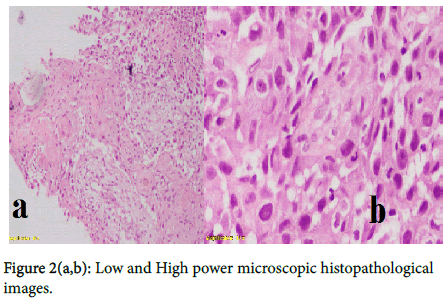
Biopsy was done which showed features of Metastatic Squamous cell carcinoma [Figure 2(a,b)].
Metastatic workup was done with Chest X-Ray and Ultrasound of Abdomen and Pelvis which were normal. Considering oligometastasis, treatment options of surgery, palliative RT, palliative chemotherapy were offered to the patient.
He underwent palliative RT 39Gy/13 fractions in view of pain at the local site, delivered by 3DCRT technique which he completed in January 2018. Post palliative RT, he had good pain relief. He was further planned for 3 weekly platinum + taxol based palliative chemotherapy for 6 cycles and monthly Zoledronic acid injections. He received 1st cycle of chemotherapy on 9th February 2018.
Discussion
The most common pattern of spread of Head and neck squamous cell carcinoma (HNSCC) is local extensions followed by lymphatic spread. The incidence of distant metastasis at presentation is approximately 10% and is usually found in the Lungs, Brain, Bones, and Skin. Several factors contribute for the propensity of HNSCC for distant metastasis. They are:- higher stage of the tumor at the initial presentation, size of the primary lesion (T4), the grade of the tumor and the site of the lesion - with the incidence being highest in the hypopharynx 60%, followed by the base of the tongue 53% and the anterior tongue 50% [1,2].
One of the main reasons for treatment failure in HNSCC patients who achieved loco-regional control is the development of distant metastasis. The most common sites of distant metastases (5 year incidence) documented in literature are Lungs (66%) and Bones (22%) [3].
In one of the largest study done by Kapoor et al. of 8326 HNSCC patients in India, the prevalence of bone metastasis was found to be 0.3%. The most common primaries causing bone metastasis in HNSCC were tonsil and tongue. They also reported that the incidence of bone metastases were more common in the younger age group (< 40 y) when compared to > 40 y. The common sites of bone metastases were spine and pelvis accounting for nearly 90% of overall. Metastasis to appendicular skeleton is comparatively less common, owing to less vascularity of the yellow marrow in the appendicular skeleton compared to red marrow in the axial skeleton [4]. One can argue that bone metastases to the appendicular skeleton is likely to be symptomatic (pain exacerbated during movement, pathological fracture, swelling) in the earlier stage of the disease when compared to those that arise from the axial skeleton.
Comparing our case with the Kapoor, et al. [4] series, the site of primary and the aggressive nature of HNSCC in the younger age group are common adverse prognostic features. Also the initial locally advanced presentation could also be considered as a high risk feature. Kapoor et al. study had shown that bone metastasis was more common in axial skeleton; our patient had developed distant metastasis in the left sided tibia which was by itself, an uncommon site of metastasis in the appendicular skeleton [4].
The early diagnosis of distant metastasis from HNSCC to any site presents a clinical challenge as these patients are usually asymptomatic and there are no useful screening tests for their early diagnosis and treatment. This is justified by the prevalence of metastases at autopsy (37-57%) being much higher than the clinical studies (4-26%) [5].
Serum Alkaline Phosphatase, Plain X-rays, CT and Bone Scans are the most frequently used investigations for detection of bone metastases. Bone scans have better sensitivity when compared to conventional radiographs but they have low specificity in identification of metastases [6].
Positron emission tomography-computed tomography with fluorodeoxyglucose F18 (18 F-FDG-PET/CT) has emerged as a useful investigation for the identification of early bone metastases from HNSCC. It also allows for detection of occult lung and liver metastases and this early detection frequently influences therapeutic decision making [7].
Interpretation
Whole body FDG PET-CT is an invaluable tool for locally advanced HNSCC for initial staging and Radiation treatment planning. During follow-up, it can be considered when there is clinical/radiological/ endoscopic suspicion of persistent/progressive disease or for treatment response assessment following systemic therapy. In this case report, we hypothesize that PET-CT can be considered for early detection of metastatic disease in treated patients of HNSCC less than 40 years of age, who had high risk features at initial presentation, as there is a relatively higher risk of disease progression in this group compared to the rest of the cohort of HNSCC.
Limitations
This is a single case study, which in itself has several drawbacks. Hypothesis testing based on single case studies are rarely formulated even in the case of an uncommon clinical scenario. Standard guidelines recommend that PET-CT be performed during follow up when there is suspicion of progressive disease or for assessment of treatment response following systemic therapy and not as a routine follow-up investigation in HNSCC.
Conclusion
Bone metastasis although very uncommon in treated HNSCC patients, presents an important concern mainly because of its tendency to occur more frequently in younger individuals and adversely impacting the survival of the patient, reducing the time from distant metastasis to death . Recent advances like the use of 18 F-FDGPET/ CT scans for follow-up of high risk HNSCC patients may allow for early detection and treatment, although recommendations for routine usage remains to be studied with larger samples.
References
- Bhandari V, Jain RK (2013) A retrospective study of incidence of bone metastasis in head and neck cancer. J Can Res Ther 9: 90-93
- Kotwall C, Sako K, Razack MS, Rao U, Bakamjian V, et al. (1987) Metastatic patterns in squamous cell cancer of the head and neck. Am J Surg 154: 439-442.
- Holsinger FC, Myers JN, Roberts DB, Byers RM. (2000) Clinicopathologic predictors of distant metastases from head and neck squamous cell carcinoma. In the proceedings of 5th International Conference on Head and Neck Cancer, San Francisco, USA.
- Kapoor A, Kalwar A, Narayan S, Kumar N, Singhal MK, et al. (2015) Analysis of bone metastasis in head and neck squamous cell carcinoma: Experience of a regional cancer center. Clin Cancer Investig J 4: 206-210
- León X, Quer M, Orús C, Venegas MDP, López M (2000) Distant metastases in head and neck cancer patients who achieved loco-regional control. Head Neck 22: 680-686
- Fujimoto R, Higashi T, Nakamoto Y, Hara T, Lyshchik A, et al. (2006) Diagnostic accuracy of bone metastases detection in cancer patients: Comparison between bone scintigraphy and whole-body FDG-PET. Ann Nucl Med 20: 399-408.
- Basu D, Siegel BA, McDonald DJ, Nussenbaum B (2007) Detection of occult bone metastases from head and neck squamous cell carcinoma: Impact of positron emission tomography computed tomography with fluorodeoxyglucose F 18. Arch Otolaryngol Head Neck Surg 133: 801-805
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi