Case Report, J Spine Neurosurg Vol: 12 Issue: 2
To Study Role of Temporary Fixation by Pedicular Screw in Spondylodiscitis Secondary to Tuberculosis Origin by Percutaneous Placement of Pedicular Screw with Recent Update on Advancements in Role of Surgical Intervention in Such Scenario
Nishant Nishant*
Department of Spine Services, Rameshwaram Orthopedic and Spine Clinic, Patna, India
*Corresponding Author: Nishant Nishant
Department of Spine Services, Rameshwaram Orthopedic and Spine Clinic, Patna, India
Tel: 919560265449
E-mail: nishantspine@gmail.com
Received date: 17 March, 2022, Manuscript No. JSNS-22-57639; Editor assigned date: 21 March, 2022, PreQC No. JSNS-22-57639 (PQ); Reviewed date: 04 April, 2022, QC No. JSNS-22-57639; Revised date: 16 May, 2022, Manuscript No. JSNS-22-57639 (R); Published date: 23 May, 2022, DOI: 10.4172/2325-9701.1000145
Citation: Nishant N (2022) To Study Role of Temporary Fixation by Pedicular Screw in Spondylodiscitis Secondary to Tuberculosis Origin by Percutaneous Placement of Pedicular Screw with Recent Update on Advancements in Role of Surgical Intervention in Such Scenario. J Spine Neurosurg 11:7
Abstract
Aim: To study role of temporary fixation by pedicular screw in spondylodiscitis secondary to tuberculous origin by percutaneous placement of pedicular screw with recent update on advancements in role of surgical intervention in such scenario.
Methods: We share the details of prospectively 32 cases of spondylodiscitis secondary to tuberculosis treated for time span of one year. Management process included clinical assessment, radiological evaluation and lab studies with over a year follow up after surgery. Visual Analogue Scale (VAS score) and Oswestry Disability Indices (ODI scale, Hindi version) were used for outcome measure.
Results: 32 cases had percutaneous fixation for tuberculous spondylodiscitis by using percutaneous pedicular screw instrumentation. The female to male to ratio was 19:13. The average follow up was 14 months ± 6 days and the duration for fusion was reported around six months. The mean duration of stay in hospital was 4.006 ± 1.17 days. The average loss of blood was 27.18 ml ± 17.71. The mean surgical time was 121.25 ± 14.59 minutes. The medical management in the form of ATT was continued for 12-18 months. Mean 48 days after surgery, and one year at follow up, CRP, ESR, pain scores (VAS Score), and ODI returned to their baseline from their the initial rise. No skips lesions were found on MRI in any case. No failure of instrumentation was reported without any decline in neurovascular condition after operative intervention.
Conclusion: Primary treatment of tuberculosis spine has been chemotherapy with limited indications for surgery and that too in selected cases with proper indications. Severe pain in the presence of spondylodiscitis with neurological deficit or deformity projects as an unclear situation and a temporary surgical fixation gives stability to prevent uneventful neurological injury, promote early healing with faster rehabilitation in contrast to strict bed rest and external bracing.
Keywords: Computed tomography; Magnetic resonance imaging; Immobilization; Hypostatic pneumonia; Osteoporosis
Introduction
Tuberculosis of spine is the commonest cause of musculoskeletal TB accounting for 1% of all TB cases and 50% of osseous involvement [1,2]. Popularly known as Pott’s disease, usually causes spondylodiscitis with or without affecting the adjoining structur es [3]. Routine radiographs are not sufficient to diagnose early involvement [4]. The commonest presentation is affliction of the disc space causing spondylodiscitis or involvement of the posterior structures of the spine. In such scenario, higher modalities of investigations like Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) aid in picking up the lesions sooner than compared to radiographs alone. Presence of inflammation around the spine like the bony or soft tissue involvement is the clue to diagnosis in such advanced investigating modalities. Cornerstone of management is medical management with limited surgical indications. Any advancement of angular deformity like kyphosis or neurological deterioration needs decompression, adequate debridement to halt formation or progression in the deformed spine [5-7]. Debridement has its complications like further trauma to soft tissue with more complications. There is inevitable damage even to healthy tissue despite all precautions which delays the recovery period. Pott’s is well known medical disease with excellent treatment with antituberculous medications. Similar response with medication is witnessed in pyogenic causes inflicting the disc space. Bed rest along with antituberculous chemotherapy is the mainstay and pillar against the tubercle bacilli inflicting the spine with dis-ease process at the spinal elements.
Recently, this practice has been questioned as the prolong immobilization adversely affects lung function leading to hypostatic pneumonia, osteoporosis, and declining limb strength.
Some author’s describe that due unresponsiveness and inadequate treatment in 5-11% of Pott’s spine patients on treatment has further aggravated the already challenging scenario. In such cases; early intervention is a necessity to thwart the damages linked like osseous destruction, worsening deformity and intractable pain during the infective duration.
Recently developed techniques such as small incision percutaneous technique has provided an alternative approach in repair process by functioning as an inside splint or brace by assisting patients in early ambulation and rehabilitation by giving a rigid internal support [8,9]. It has an additional advantage of having soft tissue protection and least impairment of adjacent healthy tissue by less aggressive modality of treatment. Pott’s disease requires a prerequisite of a rigid stabilization for healing tissue. Adequate healing insures that the deformity does not progress. These parameters have gained approval but very few published work supports the early but limited intervention fixation by pedicular screws, hence the need for this study. This novel procedure has gained attention since it aids in providing adequate pain relief, combating angular deformity and has improved the outcome by decreasing the disability-adjusted life year (Daly).
Case Presentation
This was a prospective study, conducted in our orthopedic department at Rohilkh and Medical College and Hospital, with ethical committee acceptance with written and informed written con-sent from each patient. The data collection included clinical and imaging data of 62 cohorts with diagnosed Pott’s spine along with complications. Out of 62 patients, 32 cases were evaluated after meeting criteria of exclusion and percutaneous pedicular screw were placed with existing spondylodiscitis of tubercular origin. Our inclusion criteria were: 1) Progressive bone destruction tending toward deformity, 2) Unstable spinal elements, and 3) Persistent pain. Exclusion basis where: 1) Neurological deficit, 2) Large abscess. Same surgeon performed the PPS fixation in every case.
Perioperative management: Diagnosis as established using a blood picture test, tissue diagnosis (biopsy) and other investigating modalities likes (X-ray, CT, and MRI) with minimum of 2 weeks of antituberculous treatment before proceeding with surgery. The chemotherapy drugs were prescribed for minimum duration of one year, till healed lesion documented on repeat MRI.
Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP) decreased, and serum albumin was obtained and recovery conditions were measured. Patient was mobilized on first postoperative day following surgery. Post-surgical bracing was recommended and was discontinued following treatment for 2-3 weeks as tolerated by the patient.
Duration chemotherapy was around 36 weeks of following RHZE regimen for 9 months, and another 3 months of HRE (Isoniazid, Rifampicin and Ethambutol) chemotherapy was administered [10].
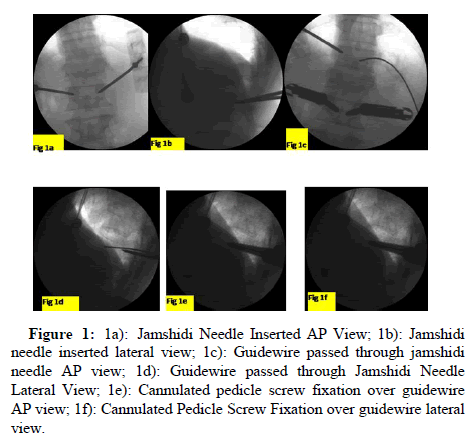
Operative techniques: All cohorts were positioned in prone under the influence of general anesthesia, on radiolucent spine frame (Allen spine frame) with free abdomen. Adequate lordosis was maintained and the bony prominences were well padded, with arms in abduction and legs in extension on adequately padded board. Antibiotic prophylaxis was given in form of first generation cephalosporin, Cefazolin 1 gm intravenous before skin incision. Under C arm guidance, Anteroposterior (AP) and lateral views were taken and the vertebral levels were identified and lateral pedicular, inter-pedicular and midline lines were marked with marker pen. A slight lateral entry point lateral to the lateral border of pedicle is chosen for trasnpedicular placement of screw especially in lumbar levels. Through paraspinal approach, the skin incision is made be large enough to accommodate the extenders of the instrumentation. The entry is made with a Jamshidi needle in both views usually in the upper outer quadrant. A mallet is used to advance in the trasnpedicular channel approximately 30 mm and not to cross the medial border (Figure 1a-1f).
Figure 1: 1a): Jamshidi Needle Inserted AP View; 1b): Jamshidi needle inserted lateral view; 1c): Guidewire passed through jamshidi needle AP view; 1d): Guidewire passed through Jamshidi Needle Lateral View; 1e): Cannulated pedicle screw fixation over guidewire AP view; 1f): Cannulated Pedicle Screw Fixation over guidewire lateral view.
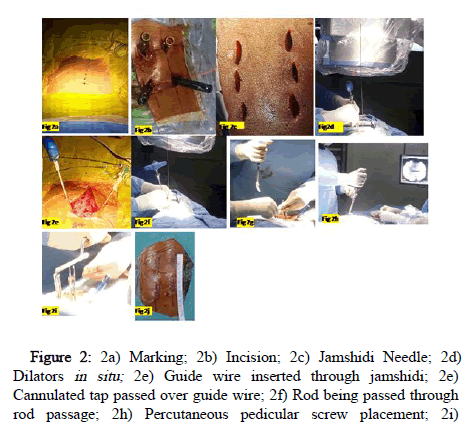
The guide wire is inserted through the needles under C-Arm guidance followed by placement of serial dilators and screw extenders over the guide wire. Three dilators are used and later two are removed, leaving behind the final dilator to be used as screw extender, is kept in situ, as protection sleeve during tapping. Cannulated screws are placed through these extenders and later removed after screw placement. This entire step is performed under lateral view. A rod measuring device is used to measure appropriate rod length with the extenders assembled. Rod bender is used to contour the rods prior to insertion or pre-bent titanium rods were placed using, a rod passer passage across the screws using medtronic longitude screws system. The rod inserter is fitted over screw extenders the rod are placed percuteously from the proximal incision site, followed by compression and tightening and later caps broken off from the screw head (Figure 2a-2j).
Figure 2: 2a) Marking; 2b) Incision; 2c) Jamshidi Needle; 2d) Dilators in situ; 2e) Guide wire inserted through jamshidi; 2e) Cannulated tap passed over guide wire; 2f) Rod being passed through rod passage; 2h) Percutaneous pedicular screw placement; 2i) Pedicular screw tightening with extenders; 2j) Incision closure with staples.
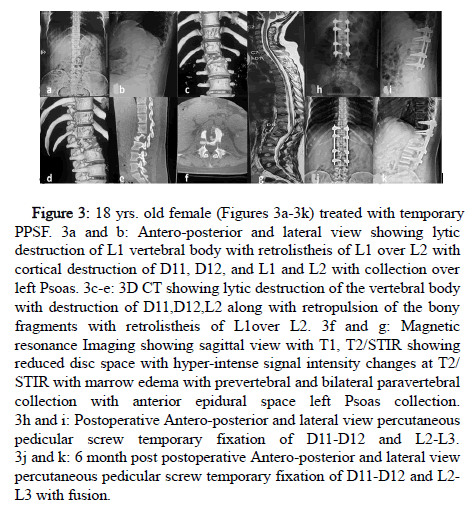
Early ambulation was encouraged first post-operative day as tolerated by patient. (Figures 3-5 illustration with Intraoperative pictures from Figures 1 and 2).
Figure 3: 18 yrs. old female (Figures 3a-3k) treated with temporary PPSF. 3a and b: Antero-posterior and lateral view showing lytic destruction of L1 vertebral body with retrolistheis of L1 over L2 with cortical destruction of D11, D12, and L1 and L2 with collection over left Psoas. 3c-e: 3D CT showing lytic destruction of the vertebral body with destruction of D11,D12,L2 along with retropulsion of the bony fragments with retrolistheis of L1over L2. 3f and g: Magnetic resonance Imaging showing sagittal view with T1, T2/STIR showing reduced disc space with hyper-intense signal intensity changes at T2/ STIR with marrow edema with prevertebral and bilateral paravertebral collection with anterior epidural space left Psoas collection. 3h and i: Postoperative Antero-posterior and lateral view percutaneous pedicular screw temporary fixation of D11-D12 and L2-L3. 3j and k: 6 month post postoperative Antero-posterior and lateral view percutaneous pedicular screw temporary fixation of D11-D12 and L2- L3 with fusion.
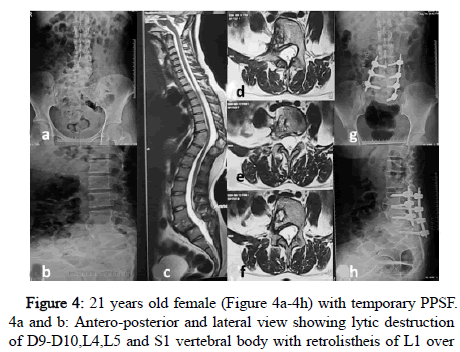
Figure 4: 21 years old female (Figure 4a-4h) with temporary PPSF. 4a and b: Antero-posterior and lateral view showing lytic destruction of D9-D10,L4,L5 and S1 vertebral body with retrolistheis of L1 over L2 with cortical destruction of D11, D12, and L1 and L2 with collection over left Psoas. 4c-f: Magnetic resonance Imaging showing sagittal view with T1, T2/STIR showing reduced disc L5-S1 space with hyper-intense signal intensity changes at T2/STIR with marrow edema with bilateral paravertebral collection with anterior epidural space bilateral Psoas collection. 4g-h: 8 months Postoperative Anteroposterior and lateral view percutaneous pedicular screw temporary fixation of bilateral L4, L5 Right S1 with healed and fused of L5-S1 spondylodiscitis.
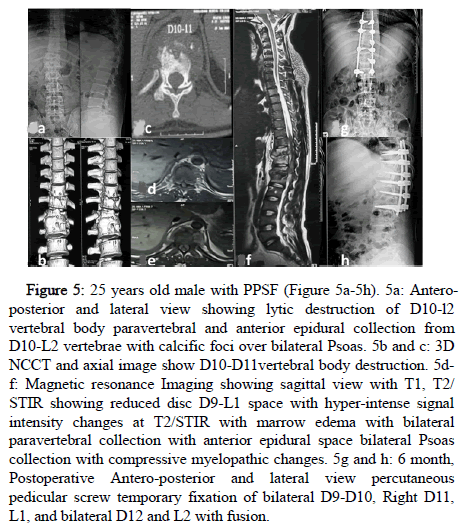
Figure 5: 25 years old male with PPSF (Figure 5a-5h). 5a: Anteroposterior and lateral view showing lytic destruction of D10-l2 vertebral body paravertebral and anterior epidural collection from D10-L2 vertebrae with calcific foci over bilateral Psoas. 5b and c: 3D NCCT and axial image show D10-D11vertebral body destruction. 5df: Magnetic resonance Imaging showing sagittal view with T1, T2/ STIR showing reduced disc D9-L1 space with hyper-intense signal intensity changes at T2/STIR with marrow edema with bilateral paravertebral collection with anterior epidural space bilateral Psoas collection with compressive myelopathic changes. 5g and h: 6 month, Postoperative Antero-posterior and lateral view percutaneous pedicular screw temporary fixation of bilateral D9-D10, Right D11, L1, and bilateral D12 and L2 with fusion.
Postoperative assessments: The blood loss with total surgical time was recorded. Conventional radiographs and CT scans done 4 weeks, 6 weeks and 24 weeks following spinal fixation to assess stability with spinal instrumentation.
Results
Only 32 out of 62 patients with Pott’s spine were reviewed and met our inclusion criteria. 9 had thoracic level disease and 23 had lumbar involvement. The age of presentation was 38.81 ± 8.19. The male to female ratio was 19:13. The age group ranged from 26 to 55 years old. Data included duration of surgery, intraoperative loss of blood and time of stay in hospital (Table 1).
| In our study (n=32) | Historical cohort (Song, et al.) | |
|---|---|---|
| Gender: Male/Female | 19:13 | 13/9 |
| Age | 38.81 ± 8.32 | 44.86 ± 11.01 |
| Levels | ||
| Thoracic | 9 | 8 |
| Lumbar | 23 | 14 |
| Operative time (minutes) 121.25 ± 14.59 121.86 ± 24.94 | ||
| Blood loss (mL) | 27.18 ± 17.71 | 73.05 ± 36.78 |
| Hospital stay (day) | 4.006 ± 1.17 | 8.05 ± 1.70 |
Table 1: Demographic and operation data of patients.
The de-tailed follow up data has been recorded (Table 2).
| Age | sex | Level of PIVD | Pre-operatively | ODI Preop | 3 M | 12 M | Preop | WBC 3M | Intraoperative | Serum baseline | Length of hospital stay | Mean Surgical Time | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| VAS | VAS | ODI Preop | ODI | ODI | 4-10.8 × 103 | 4-10.8 × 103 | Blood Loss | CRP | ESR | stay | Minutes | |||
| 28 | M | L5 S1 | 7 | 4 | 72 | 46 | 22 | 12.1 | 4.5 | 30 | 20 | 40 | 5 | 140 |
| 36 | M | L4 S1 | 8 | 5 | 84 | 42 | 12 | 13.4 | 4.1 | 20 | 18 | 55 | 3 | 120 |
| 44 | F | D12-L1 | 8 | 3 | 76 | 40 | 10 | 14.5 | 5.2 | 20 | 5 | 42 | 3 | 110 |
| 52 | F | D6-D7 | 8 | 4 | 86 | 34 | 12 | 13.8 | 6.3 | 20 | 12 | 66 | 2 | 130 |
| 42 | F | D9-D10 | 8 | 3 | 74 | 44 | 14 | 16.4 | 7.8 | 40 | 8 | 78 | 5 | 140 |
| 36 | F | L4-L5 | 8 | 4 | 88 | 46 | 10 | 15.4 | 6.9 | 20 | 8 | 68 | 7 | 160 |
| 46 | M | D12-L1 | 7 | 4 | 70 | 48 | 12 | 13.4 | 5.8 | 80 | 6 | 78 | 7 | 150 |
| 40 | F | L4 S1 | 7 | 3 | 68 | 34 | 10 | 13.9 | 4.7 | 90 | 8 | 67 | 5 | 140 |
| 33 | M | L5 S1 | 7 | 4 | 74 | 32 | 14 | 16 | 8.8 | 20 | 12 | 63 | 4 | 130 |
| 35 | M | L3-L4 | 7 | 4 | 88 | 44 | 16 | 17.5 | 9.9 | 20 | 10 | 58 | 3 | 140 |
| 32 | F | D10-D11 | 7 | 5 | 70 | 38 | 18 | 18.8 | 9.7 | 70 | 6 | 32 | 3 | 130 |
| 34 | F | L5 S1 | 7 | 5 | 72 | 40 | 20 | 14.4 | 8.7 | 20 | 5 | 44 | 4 | 140 |
| 36 | F | L3-L4 | 8 | 3 | 74 | 32 | 22 | 15.7 | 7.3 | 30 | 12 | 12 | 4.25 | 120 |
| 47 | F | L4-L5 | 8 | 3 | 68 | 32 | 22 | 11.2 | 8.4 | 20 | 12 | 22 | 3 | 110 |
| 55 | M | L5 S1 | 8 | 3 | 64 | 32 | 22 | 13.7 | 7.3 | 30 | 12 | 10 | 3 | 110 |
| 33 | M | L4-L5 | 7 | 3 | 66 | 32 | 22 | 11.9 | 8.8 | 20 | 12 | 32 | 3 | 110 |
| 28 | M | L4-L5 | 7 | 3 | 76 | 32 | 14 | 12.4 | 9.8 | 20 | 12 | 32 | 3 | 110 |
| 44 | M | L3-L4 | 7 | 3 | 70 | 32 | 14 | 11.6 | 7.6 | 20 | 12 | 32 | 4 | 110 |
| 37 | M | L5 S1 | 8 | 3 | 70 | 32 | 14 | 13.5 | 7.7 | 20 | 12 | 12 | 4 | 110 |
| 43 | F | L5 S1 | 8 | 3 | 66 | 32 | 14 | 12.7 | 7.4 | 20 | 10 | 12 | 4 | 110 |
| 42 | F | D12-L1 | 8 | 3 | 64 | 32 | 14 | 15.6 | 7.5 | 20 | 10 | 12 | 4 | 110 |
| 33 | M | L5 S1 | 7 | 3 | 68 | 34 | 14 | 17.6 | 7.8 | 20 | 10 | 22 | 5 | 110 |
| 29 | M | L4-L5 | 7 | 3 | 80 | 34 | 10 | 19.6 | 8.5 | 20 | 10 | 10 | 5 | 110 |
| 53 | F | L4-L5 | 7 | 3 | 72 | 34 | 10 | 18.6 | 8.1 | 20 | 10 | 10 | 5 | 110 |
| 26 | M | L5 S1 | 7 | 3 | 66 | 34 | 10 | 24.2 | 7.3 | 20 | 10 | 10 | 5 | 110 |
| 28 | M | D12-L1 | 7 | 3 | 58 | 24 | 10 | 11.7 | 6.9 | 20 | 10 | 10 | 5 | 110 |
| 30 | F | D12-L1 | 7 | 3 | 54 | 22 | 10 | 12.6 | 6.7 | 20 | 6 | 10 | 3 | 110 |
| 44 | M | L4-L5 | 7 | 3 | 56 | 22 | 10 | 12.8 | 8 | 20 | 6 | 22 | 3 | 130 |
| 55 | M | L5 S1 | 7 | 3 | 64 | 26 | 14 | 13.4 | 9.3 | 20 | 6 | 12 | 3 | 110 |
| 39 | M | D11-D | 7 | 3 | 70 | 28 | 14 | 13.1 | 6.7 | 20 | 6 | 12 | 3 | 130 |
| 48 | M | L3-L | 7 | 3 | 66 | 30 | 14 | 13.5 | 8.2 | 20 | 6 | 12 | 3 | 110 |
| 34 | M | L5 S1 | 8 | 3 | 60 | 32 | 14 | 13.8 | 5.5 | 20 | 6 | 12 | 3 | 110 |
Table 2: Pathogens detected (n=32 patients).
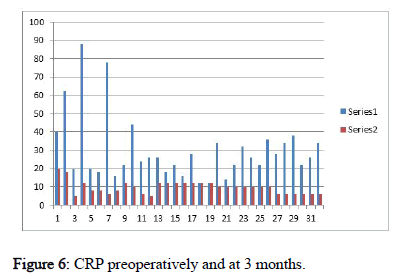
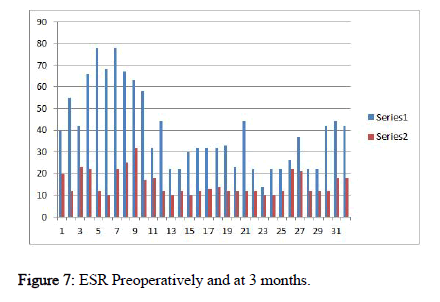
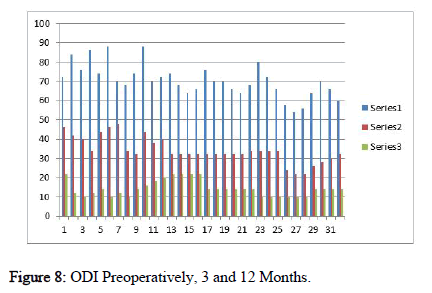
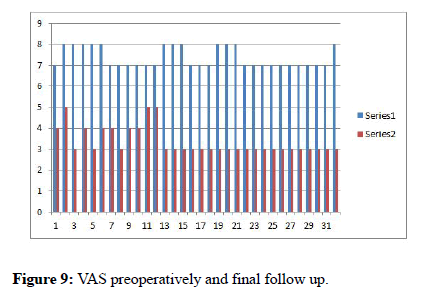
14 months ± 6 days over 24 weeks was fusion time for the cohorts. The VAS score improved post-operatively from 7.37 ± 0.48 and 3.37 ± 0.64, respectively. The ODI (%; Hindi version) was 70.43 ± 8.30, at 6 weeks post-surgical ODI of 34 % improvement with 34.25 ± 6.57 at 12 weeks was 14.31 ± 14.06 with 59 % improvement at final follow up. The average blood loss was 27.18 ml ± 17.71 and the surgical time span of 121.25 ± 14.59 minutes. Presence of co-morbidity or immunecompromised status was not reported in any patient. CRP, ESR pain scores (visual analog scale) and ODI were lower at 3months and at final review (Figures 6-9).
No skip lesions, instrumentation loosening or failure or resurgence of the tubercle bacilli resurfaced at final review. Following surgery, patients were neurologically sound. The pain at the back region improved in couple of weeks’ time frame including radiculopathy. 2 cases had superficial infection involving the lumbar level have underwent culture sensitively guided appropriate antibiotics treatment. All patient achieved baselines CRP in 12 weeks, with equal number of the cases had mild increase in ESR. Fusion was gained by end of 24 weeks to 48 weeks in every cohort.
Discussion
In developing countries, TB is still wide spread with changing disease spectrum despite medically curable entity and progress in diagnosis and treatment. Anti-tuberculous medications have been the pivotal role in curing the ailment and reduce disease burden amongst those exposed. The adequacy of treatment was reflected by return of baseline ESR and CRP as a marker of successful chemotherapy treatment [11-13]. It is established that even where debridement was performed, anti-Tb drugs were unable to halt the spread. Controversy has been in current literature whether early surgery is required or has any change in treatment outcome. A study summarized that no extra successful outcome was witnessed when cases underwent surgery with concurrent chemo-therapy versus anti-tuberculous drugs alone for treating Potts spine with conclusion that chemo-therapy alone was sufficient with immobilization in bed.
Recent authors have acknowledged the presence of two primary inherent defects in Pott’s spine. The Firstly, the neurology concomitant osteoporosis, pulmonary embolism, hypostatic pneumonia and even DVT can be aggravated due to absence of inherent strong stabilization or prolonged immobilization in form of bed rest. Secondly, even with strict immobilization with bracing the lack of adequate internal stability essential for the segment which leads to intractable pain at the back, aggravation of deformity can occur. Another study 4 pointed out certain specific indication like deterioration in neurology, not responding to antituberculous medications for 4 to 6 weeks, or existing instability (antero-posterior or lateral translation; kyphosis), for intervening by early surgery in those patients without loss of neurological status. Classical strategies were to perform focal debridement, achieve proper stability by spinal instrumentation and performing adequate decompression to prevent progressive deformity [14]. The aggressive approach during surgery for Pott’s spine has disastrous effects on degree of loss of blood or impairment to the neurovascular structures. Additionally, procedures warrant spinal fixation with healing after debridement. This raises the concern and objection to the controversial intervention of radical procedure in Pott’s spine. To address such concerns, we suggest temporary percutaneous stabilization as assistive device like an internal splint or brace by placing pedicular screws which gives rigid support for such pathological conditions. Magerl introduced this concept by using external fixator in thoracic and lumbar spine [15]. A Magerl modification technique was incorporated for perfect entry point for precise placement of PPS [16]. Foley and Gupta et al further designed percutaneous pedicle screw treating spinal tumors, spinal trauma and even spondylolistheis [17-20].
Minimal disruption of soft tissue or Para spinal muscles by mini stab incision procedures have this advantage which prevents worsening of deformity [21]. Amongst our 32 patients, outcome (imaging and functional) was reflected by achieving pain relief, improving the disability, attaining good spinal curvature and prevention deformity progression especially kyphosis. The laboratory parameters like ESR has established as a sensitive and specific parameters for Tb than for pyogenic infections because it's an inflammatory marker for chronic infection. But if increase in ESR accompanied by normal or moderate leukocytosis, we can suspect secondary infection, as reflected in two of our cases of superficial infection. A highly sensitive marker is for inflammation is CRP which is increased in Tb. Furthermore, it is compulsory to monitor CRP and ESR to monitor disease spread and to check proper treatment with anti-tub treatment. However, these markers are nonspecific and are raised other conditions with inflammation or autoimmune conditions [22]. However, the quantitative rises to certain levels are more reflection than mere raised parameter. These have been quoted as “early phase reactants”, and currently are the cheapest with good reliability for monitoring benefit of medications. We observed that preoperatively, all these makers were raised and finally fall and achieve their baseline on continued treatment which further establishes our findings. One of the major causes for the existence of pain over the back is due to the underlying destruction of osseous elements further leading to instability [23]. Our study outcome involved assessment of disability by calculating the Indian scale of the ODI 10 included measuring of pain severity by VAS scale which improvement clinical test.
Every case reported successful bone healing further substantiates our findings. This supports our hypothesis that a minimally invasive technique like percutaneous spinal instrumentation, does not disturb the fusion process as the tuberculosis foci heals by regenerating bony tissue. Additionally, it decrease operative time, bloodless, time of stay as in patient and avoids complications pertaining to prolong immobilization in bed with distinct benefits of quicker rehabilitation.
Conclusion
We ascertain that PPF is safe, small incision procedure to provide internal rigid stabilization spinal conditions. PPF provides pain relief, improves disability, attains fusion which prevents progression of angular curve in treating Pott’s spinal involvement with spondylodiscitis avoids the requirement of radical debridement advocated earlier literature.
References
- Rasouli MR, Mirkoohi M, Vaccaro AR, Yarandi KK, Rahimi Movaghar V (2012) Spinal tuberculosis: Diagnosis and management. Asian Spine J 6:294–308. [Googlescholar][Indexed]
- Jain AK (2010) Tuberculosis of the spine: A fresh look at an old disease. J Bone Joint Surg Br 92: 905–913. [Googlescholar] [Crossref] [Indexed]
- Gouliouris T, Aliyu SH, Brown NM (2010) Spondylodiscitis: update on diagnosis and management. J Antimicrob Chemother 65:11-24. [Googlescholar] [Crossref][Indexed]
- Govender S (2005) Spinal infections. J Bone Joint Surg 87-B:1454-1458. [Googlescholar] [Crossref]
- Garg RK, Somvanshi DS (2011) Spinal tuberculosis: A review. J Spinal Cord Med 34:440–454. [Googlescholar][Crossref][Indexed]
- Tuli SM (2013) Historical aspects of Pott’s disease (spinal tuberculosis) management. Eur Spine J 4:529–538. [Googlescholar][Crossref][Indexed]
- Dunn RN, Ben Husien M (2018) Spinal tuberculosis. Bone Joint J 100-B:425-431. [Googlescholar] [Crossref] [Indexed]
- Guo S, Zhu K, Zhang S, Ma B, Yang M, et al. (2019) Percutaneous pedicle screw fixation alone versus debridement and fusion surgery for the treatment of early spinal tuberculosis: a retrospective cohort study. Med Sci Monit 25:1549-1557. [Googlescholar][Crossref][Indexed]
- Kulkarni AG, Mewara NG (2018) The scope of minimally invasive techniques in spinal infections. Indian Spine J 1:17-23. [Googlescholar]
- Nishant HS, Kapoor KS (2014) New modified English and Hindi oswestry disability index in low back pain patients treated conservatively in Indian population. Asian spine J 8:632-638. [Googlescholar][Indexed]
- Liu P, Zhu Q, Jiang J (2011) Distribution of three anti-tuberculous drugs and their metabolites in different parts of pathological vertebrae with spinal tuberculosis. Spine 36:E1290–1295. [Googlescholar][Crossref][Indexed]
- Ge Z, Wang Z, Wei M (2008) Measurement of the concentration of three anti-tuberculosis drugs in the focus of spinal tuberculosis. Eur Spine J 17:1482–1487. [Googlescholar] [Crossref][Indexed]
- Dai LY, Jiang LS, Wang YR, Jiang SD (2010) Chemotherapy in anterior instrumentation for spinal tuberculosis: highlighting a 9-month three-drug regimen. World Neurosurg 73:560–564. [Googlescholar] [Crossref][Indexed]
- Jutte PC, van Loenhout-Rooyackers JH (2006) Routine surgery in addition to chemotherapy for treating spinal tuberculosis. Cochrane Database Syst Rev 25:CD004532. [Googlescholar][Crossref][Indexed]
- Magerl FP (1984) Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin Orthop Relat Res 189:125–141. [Googlescholar][Indexed]
- Wiesner L, Kothe R, Rüther W (1999) Anatomic evaluation of two different techniques for the per-cutaneous insertion of pedicle screws in the lumbar spine. Spine 24:1599–1603. [Googlescholar][Crossref][Indexed]
- Foley KT, Gupta SK (2002) Percutaneous pedicle screw fixation of the lumbar spine: Preliminary clinical results. J Neurosurg 97:7–12. [Googlescholar][Crossref][Indexed]
- Kim JS, Choi WG, Lee SH (2010) Minimally invasive anterior lumbar interbody fusion followed by percutaneous pedicle screw fixation for isthmic spondylolisthesis: Minimum 5 years follow-up. Spine J 10:404–409. [Googlescholar][Crossref][Indexed]
- Wang H, Zhou Y, Li C, Liu J, Xiang L (2017) Comparison of open versus percutaneous pedicle screw fixation using the sextant system in the treatment of traumatic thoracolumbar fractures. Clin Spine Surg 30:E239–246. [Googlescholar][Crossref][Indexed]
- Mobbs RJ, Park A, Maharaj M, Phan K (2016) Outcomes of percutaneous pedicle screw fixation for spinal trauma and tumors. J Clin Neurosci 23: 88–94. [Googlescholar][Crossref][Indexed]
- Alander DH, Cui S (2018) Percutaneous pedicle screw stabilization: Surgical technique, fracture reduction, and review of current spine trauma applications. J Am Acad Orthop Surg 26:231–240. [Googlescholar][Crossref][Indexed]
- Huang YS, Ge CY, Feng H et al (2018) Bone cement-augmented short-segment pedicle screw fixa-tion for Kümmell disease with spinal canal stenosis. Med Sci Monit 24:928–35. [Googlescholar] [Crossref][Indexed]
- Mizuno T, Sakakibara T, Yoshikawa T, Inaba T, Kato T et al. (2018) Biomechanical stability of a cross-rod connection with a pedicle screw system. Med Sci Monit Basic Res 24:26–30. [Googlescholar] [Crossref][Indexed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi