Case Report, J Clin Image Case Rep Vol: 1 Issue: 1
Tropical Diabetic Hand Syndrome: A Case Report with an Overview of Literature
Derrick Tembi Efie1, Eugene Vernyuy Yeika1,2,3*, Cedrick Mbassi2 and Siméon Pierre Choukem1,4
1Health and Human Development Research Network, Douala, Cameroon
2Saint Elizabeth Catholic General Hospital and Cardiac Centre Shisong, Kumbo, Cameroon
3Clinical Research Education Networking and Consultancy, Douala, Cameroon
4Department of Internal Medicine and Pediatrics, Faculty of Health Sciences, University of Buea, Cameroon
*Corresponding Author : Eugene Vernyuy Yeika
Saint Elizabeth Catholic General Hospital and Cardiac Centre Shisong, Cameroon, PO Box-08, Kumbo, Cameroon
Tel: +237679934736
E-mail: eugenembinglo@gmail.com, yeika_eugene@shisonghospital.org
Received: August 14, 2017 Accepted: August 24, 2017 Published: August 31, 2017
Citation: Efie DT, Yeika EV, Mbassi C, Choukem SP (2017) Tropical Diabetic Hand Syndrome: A Case Report with an Overview of Literature. J Clin Image Case Rep 1:1.
Abstract
Background: Hand infections amongst patients living with diabetes are common in the tropical region and remain a major cause of morbidity and mortality. Tropical diabetic hand syndrome is the term that has been coined for diabetic hand infections that commonly occur in the tropics. This syndrome is not known to many physicians especially in sub-Saharan Africa and consequently it is overlooked and underreported. This indexed case is reported to create more awareness on the existence of tropical diabetic hand syndrome.
Case presentation: We report the case of 57 year-old black African driver, newly diagnosed with type 2 diabetes mellitus after he presented with a life threatening infection of the right hand for which a diagnosis of Lawal Group 3 right diabetic hand syndrome was made which eventually led to amputation of the right thumb.
Conclusion: Although tropical diabetic hand syndrome is associated with a high morbidity and mortality, its occurrence has been underreported by many medical practitioners in sub-Saharan Africa. Education of diabetic patients on hand care and appropriate glycaemic control is a cost-effective and easier way to prevent the occurrence of tropical diabetic hand syndrome.
Keywords: Tropical diabetic hand syndrome; Underreported; Sub-Saharan Africa
Abbreviations
TDHS: Tropical Diabetic Hand Syndrome
Background
Hand infections have been reported in patients living with diabetes, causing significant morbidity from amputation and functional disability or mortality from sepsis [1-3] Tropical diabetic hand syndrome (TDHS) is the term that has been coined for these diabetic hand infections because it occurs commonly in the tropics [1,3,4]. This syndrome comprises a complex pattern of hand infection that ranges from cellulitis to swelling and ulceration of the hand, which can progress to more fulminant infections such as gangrene or necrotizing fasciitis [1,2]. Factors that lead to hand infections amongst patients living with diabetes include systemic sclerosis, trauma, connective tissue disorders, vasculitic disorders and myeloproliferative disorders [5]. Unrecognized trivial trauma remains the most common predisposing factor in the tropics [1]. Early surgical intervention, proper glycaemic control, elevation of the affected hand and early initiation of broad spectrum antibiotics are essential for the rapid healing of diabetic hand infections [1,6]. Although TDHS is a major cause of morbidity and mortality amongst diabetic patients in the tropics, many physicians are less aware of the frequent occurrence [2,3,7]. This case report emphasizes on the frequent occurrence of this fatal hand sepsis amongst diabetic patients in the tropical region.
Case Presentation
A 57 year-old male black African driver presented at our centre with a gradual onset painful and progressive swelling of the right thumb of 2 weeks duration which later became ulcerated and gangrenous, all in a febrile context. This started following a trivial trauma which was initially managed as whitlow with cloxacillin and diclofenac and daily dressing as an outpatient following the first consultation in our service. This infection progressed from the tip of the thumb to involve the entire digit and later became gangrenous despite initial management. The patient had no prior history of diabetes or hypertension and did not smoke or drink alcoholic beverages.
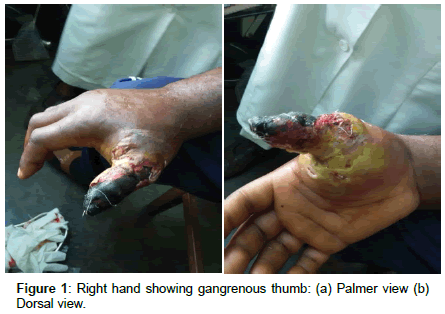
Physical examination upon presentation revealed a temperature of 38.4ºC, a pulse of 124 beats/minute, blood pressure of 150/80mm/ Hg, and a respiratory rate of 24 breaths/minute. The entire right finger was gangrenous with suppurating ulcers right to the base (Figure 1). The rest of physical examination was unremarkable.
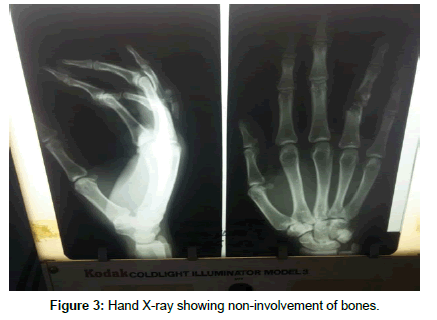
The following investigations were conducted: a complete blood count which revealed a white blood cell count of 19.3 × 109/l with neutrophil predominance and a haemoglobin level of 14.2 g/dl, an erythrocyte sedimentation rate of 67, random blood glucose of 369 mg/dl and fasting blood glucose of 330 mg/dl repeated 12 hours later. Urine analysis was unrevealing; serum creatinine was 1.2 mg/ dl and blood urea nitrogen of 47 mg/dl. Wound swab sent for culture revealed no pathologic organism after 72 hours of incubation. Hand X-ray was done and showed non-involvement of bones (Figure 2). We concluded on Lawal Group 3 Tropical Diabetic Hand Syndrome in a newly diagnosed type 2 diabetic mellitus patient.
After obtaining informed consent, the right thumb was amputated under general anaesthesia. Penrose drains were inserted on the stump (Figure 3). The patient was placed on the following intravenous antibiotics; ceftriaxone 1g 12 hourly, metronidazole 500mg 8 hourly, and pain was controlled using intravenous tramadol 100mg 12 hourly and intravenous paracetamol 1g 6 hourly and fluids (normal saline 500ml 8 hourly). Blood glucose level normalised postoperatively and the stump healed uneventfully. The patient was discharged following 3 weeks of hospitalisation with oral anti-diabetic medication metformin at 500g 12 hourly and was advised to modify his lifestyle.
Discussion
The diabetic hand is a less commonly recognized entity when compared to the diabetic foot related infections [1]. Diabetic hand infections are easily ignored and underestimated resulting in increased morbidity and mortality [1,2]. Recent studies indicate that diabetic hand infections are not as rare as they are diagnosed and reported in the tropical region especially in sub-Saharan Africa [6,7]. The frequent occurrence of TDHS warrants the need to increase its awareness amongst physicians, as early diagnosis and prompt intervention will result in better outcome [1,2]. Despite the early presentation of our patient, TDHS was not promptly diagnosed partly because he had no previous history of diabetes and probably due to lack of awareness on TDHS by the attending physician.
Management of TDHS remains challenging mainly due to late diagnosis, coupled with the lack of existing guidelines and protocols for the management of this disease entity. Nthumba et al. in a study set out to establish a protocol for the holistic management of TDHS to improve digit/hand salvage and function in their centre concluded that TDHS appears to be more aggressive in some patients than in others and a multidisciplinary approach, with early involvement of the surgical team, and a radical surgical debridement are essential to improve outcomes [8]. Although the goal of medical treatment (i.e. glycaemic control) is simple and easily achieved, surgical goals (salvage of limb or life, preservation of hand function) are more complex, costly, and difficult to achieve [8]. Educating health care workers, diabetic patients, and their relatives on hand care is an important preventive measure. Diligence in taking anti-diabetic medications, early presentation, and appropriate care of TDHS are required for meaningful improvement in outcomes of patients with diabetes who develop hand sepsis in the tropics [8].
Diabetic hand sepsis seen today in tropical countries is a reflection of a problem which previously also occurred among people with diabetes in the developed countries [4]. The reduction in its occurrence in the Western regions is probably due to increase awareness of diabetes and its complications, improved glycaemic control amongst diabetic patients and access to expert care [4]. Good health facilities that carry out educative programs on the prevention and control of diabetes and its complication are largely absent in sub-Saharan Africa in particular and the tropical region at large. Consequently, most patients remain unaware of their glycaemic status and diabetic patients are ignorant of complications. Government policies are needed to create more day care diabetic clinics that focus more on the prevention than management of diabetic complications.
Education of diabetic patients and health staff regarding proper hand care, nutrition and the importance of immediate medical consultation following hand trauma or even after unexplained redness and swelling of hand in diabetic patients will go a long way to reduce the incidence of TDHS [3,7]. Prevention of permanent disability and death due to TDHS will require early recognition by patients and medical practitioners, improved management of glycaemic levels in resource-limited countries, and surgical intervention during less severe stages of the condition [7].
Conclusion
Although tropical diabetic hand syndrome is associated with a high morbidity and mortality, its occurrence has been overlooked and consequently underreported by many physicians in sub-Saharan Africa. Education of diabetic patients on hand care and appropriate glycaemic control is a cost-effective and easier way to prevent TDHS.
Consent for Publication
Written informed consent was obtained from the patient for publication of this case report. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing Interests
The authors declare that they have no competing interests.
Authors Contributions
Eugene Vernyuy Yeika and Cedrick Mbassi managed the patient. Eugene Vernyuy Yeika wrote the original manuscript. Derrick Tembi Efie and Siméon Pierre Choukem reviewed and corrected the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors wish to acknowledge the entire surgical team for the great work they did in managing this patient.
References
- Raveendran S, Naik D, Raj Pallapati SC, Prakash JJ, Thomas BP, et al. (2016) The clinical and microbiological profile of the diabetic hand: A retrospective study from South India. Indian J Endocr Metab 20: 619-624.
- Yeika EV, Tchoumi Tantchou JC, Foryoung JB, Tolefac PN, Efie DT, et al. (2017) Tropical diabetic hand syndrome: a case Report. BMC Res Notes 10: 94.
- Naqash MM, Ahmad F, Bhat AN, Jalalie U, Najar RR (2016) Tropical diabetic hand syndrome- a case report with a short review. Int J Res Med Sci 4: 5494-5496.
- Gill G, Archibald L, Abbas ZG (2003) Diabetic hand infections in the tropics. Diabet voice 48: 17- 9.
- Singh S, Chand G, Charan S, Arora S, Singh P (2013) Peripheral Arterial Disease and Digital Gangrene: A Rare Presentation of Diabetic Hand Syndrome. J Clin Diag Res 7: 2286-2287.
- Jalil A, Barlaan PI, Keung Fung BK, Ip JW (2011) Hand infection in diabetic patients. Hand Surg 16: 307-312.
- Ngim EN, Amah P, Abang I (2012) Tropical Diabetic Hand Syndrome: report of 2 cases. Pan Afr Med J 12: 24.
- Nthumba P, Cavadas P, Landin L (2013) The Tropical Diabetic Hand Syndrome: A Surgical Perspective. Annals Plast Surg 70: 42-46.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi