Case Report, J Clin Image Case Rep Vol: 1 Issue: 1
Unusual Acute Myocardial Infarction in Young Male with Hereditary Protein C and S Deficiency
Ibrahim Osman*, Bankim Patel, George Koromia and Assad Movahed
Department of Cardiovascular Sciences, The Brody School of Medicine, East Carolina Heart Institute, East Carolina University, USA
*Corresponding Author : Ibrahim Osman
Department of Cardiovascular Sciences, The Brody School of Medicine, East Carolina Heart Institute, East Carolina University, Greenville, NC, USA 27834
E-mail: osmani@ecu.edu
Received: May 23, 2017 Accepted: July 05, 2017 Published: July 12, 2017
Citation: Osman I, Patel B, Koromia G, Movahed A (2017) Unusual Acute Myocardial Infarction in Young Male with Hereditary Protein C and S Deficiency. J Clin Image Case Rep 1:1.
Abstract
We report on a 33 year old man who presented with an acute anterolateral myocardial infarction (MI) caused by thrombotic occlusion of the left anterior coronary artery [LAD] as the initial cardiac manifestation of hereditary protein C and S deficiencies. This case report shows that acute coronary syndrome in the young population could have other causes than atherosclerotic plaque rupture. This is essential knowledge for the clinicians to consider other etiologies in the differential diagnosis such as hypercoagulable state in young patients with myocardial infarctions. Once the diagnosis is established then more appropriate management and prevention of recurrent events is possible. Furthermore, family screening could lead to a prophylactic approach in carriers of this mutation.
Keywords: Hypercoagulability; Myocardial infarction; Non-atherosclerotic coronary artery disease; Premature atherosclerosis; Young adults
Introduction
The appearance of MI under the age of 40 is rare but the lack of thermodynamically significant coronary artery disease in this age group is not so uncommon since 15-20% of these patients has normal or near normal coronary arteries (N/NNCAs). It is associated with devastating consequences because of the extensive damage that accompanies its abrupt occurrence and absence of collateral coronary circulation. The diagnosis and appropriate management of the underlying cause are essential in preventing recurrence. Other than the traditional risk factors for atherosclerosis, a variety of potential contributing factors have been identified in young patients with myocardial infarction. These include the use of oral contraceptives in young women, cocaine use, marijuana use, a factor V Leiden mutation and protein C deficiency [1-5].
Case Presentation
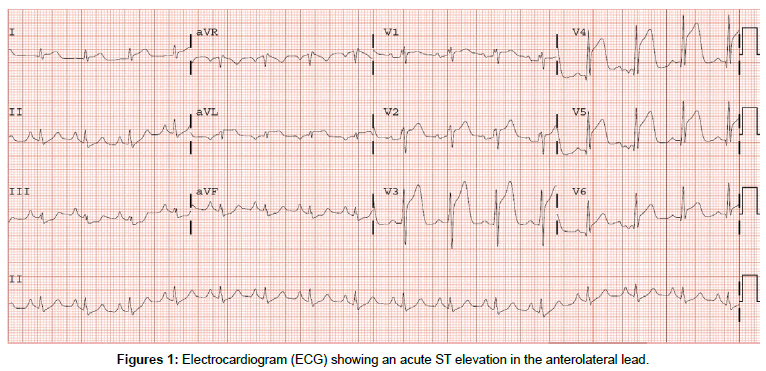
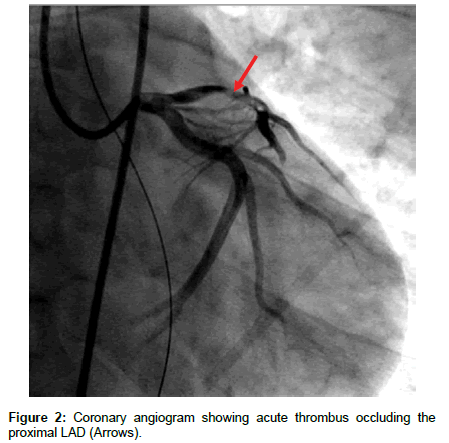
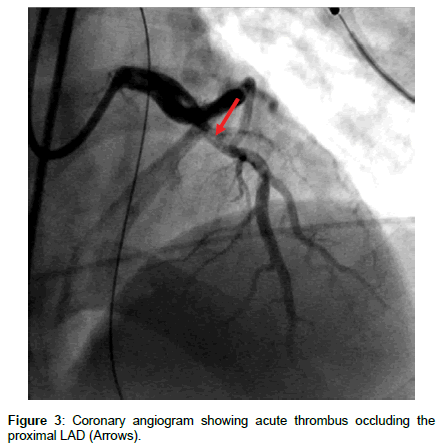
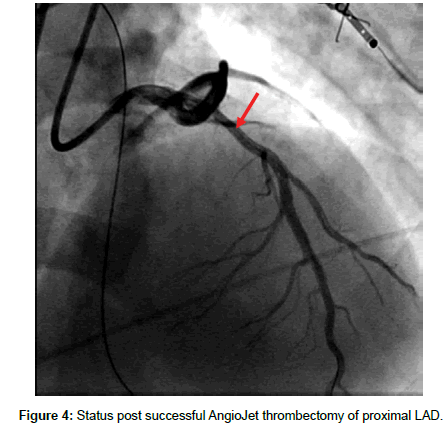
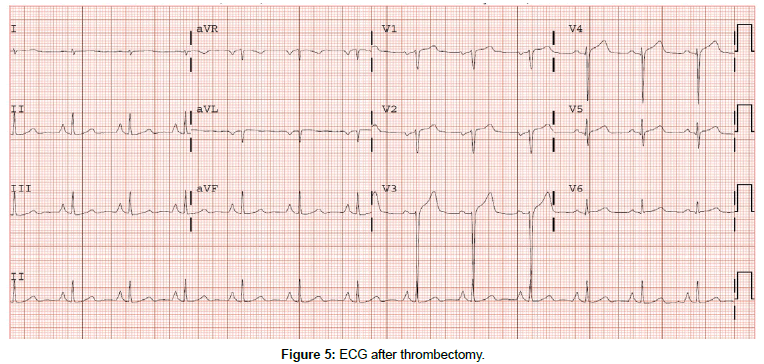
A 33 year old male with a past medical history of protein C and S deficiency, pulmonary embolism and tobacco use who presented to the emergency department for witnessed sudden cardiac arrest proceeded by chest pain while ambulating at home then developed a seizure like activity. He has a family history of clotting disorder in his mother who was diagnosed with a deep venous thrombosis and brother who experienced a myocardial infraction in his 30s. He consumes approximately half-pack/day of cigarettes with occasional alcohol and marijuana use. He was diagnosed with pulmonary embolism and protein C and S deficiencies in 2007 treated with Warfarin for 6 months then declined to continue indefinite systemic anticoagulation for the past eight years. Upon arrival of EMS, he found to have agonal breathing and posturing with cardiac monitor demonstrating a disorganized rhythm consistent with ventricular fibrillation in which advanced cardiovascular life support (ACLS) protocol was immediately initiated, received one round of defibrillation of 200 joules and was subsequently transferred to the emergency department. En route, had two more episodes of ventricular fibrillation with two rounds of successful defibrillation at 200 J. He was intubated for airway protection. Physical examination showed an unresponsive intubated male with heart rate of 74 beats per minute, blood pressure of 123/67 mm Hg, saturating at 100% with supplemental oxygen on 50% and S 3 was heard on auscultation without evidence of volume overload. Initial laboratory work up showed troponin levels of 0.03 ng/ ml then peaked at 15.61 ng/ml and leukocytosis of 21,100 k/μl. Urine drug scree was negative. An electrocardiogram (ECG) showed an acute anterolateral ST segment elevation (Figure 1). He immediately underwent a coronary angiography showing a significant thrombus burden in proximal LAD, had successful angiojet thrombectomy (Figures 2-4) with ST segment elevation resolution (Figure 5). He was admitted to the cardiac intensive care unit on therapeutic intravenous Heparin and Tirofiban infusion. Initial transthoracic echocardiogram (TTE) showed a depressed left ventricular ejection fraction (LVEF) of 30% with left ventricular regional systolic dysfunction in the LAD territories. TTE was repeated in 24 h after thrombectomy and exhibited an improved LVEF to 55%. He remains stable and was discharged with continuation of systemic anticoagulation with warfarin with INR goal 2-3, beta blocker, Aspirin, Ticagrelor and Statin.
Discussion
Acute coronary syndrome in young adults is an uncommon condition; only 2-8% of acute myocardial infarction subjects are under 40 years’ old [6,7]. Males are typically more affected, females account for only 6% in this age group [8].The mean cause of acute coronary syndrome in the young is atherosclerosis; numerous factors can lead to premature and accelerating process such as insulin resistance, diabetes, familial lipid disorder, hypertension, tobacco use, and human immunodeficiency virus infection [9]. Acute coronary syndromes may have non-atherosclerotic etiologies: Congenital coronary artery anomalies, spontaneous coronary artery dissection, vasospasm, illicit drug use and hypercoagulable states like our case. In the absence of coronary disease, the clinicians should expand the differential towards an inherited thrombophilia especially in young individuals presenting with acute coronary syndrome. The inherited thrombophilia syndromes involve several disorders including protein C deficiency, protein S deficiency, hyperhomocysteinemia, with factor V Leiden deficiency having the highest prevalence. Individual case reports on protein C and S deficiencies have been published about the consequences of arterial thrombosis resulting in myocardial infarction which is known to be a rare manifestation of these conditions. A recent work with 255 consecutive patients who had survived a STEMI ≤ 35 years of age reported that only one had deficiency of protein C (0.4%) (10) The role of protein C and S inactivates clothing factors Va and VIIa towards the formation of thrombin. In their absence, individuals have a severely higher risk for developing venous thrombosis and pulmonary embolism.
Because patients with previous venous thrombosis, also have had arterial thrombosis, there have been studies to establish whether patients with thrombophilia and antecedents of venous thromboembolisms have a higher risk of arterial thrombosis [11,12]. One study included 1081 consecutive patients (649 Female/432 Males, age range 16-93) registered with venous thromboembolism in MAISTHRO database (Main-Isar-Thrombosis). Thrombophilia screening tested the presence of factor Ⅴ Leiden, G20210A prothrombin gene mutation, antiphospholipid antibodies, factor VII, protein C, protein S and antithrombin activities. From all of the patients, 40 (3.7%) had a prior myocardial infarction (MI) and 41 (3.8%) had a stroke. Only the presence of lupus anticoagulant was found statistically significant. The conclusion was that the cumulative incidence of arterial thrombotic events is low for those with antecedents of venous thrombosis and inherited thrombophilia doesn’t seem to substantially increase the risk of arterial thrombosis [13]. Another study that included members of protein C, S and antithrombin deficient families also proved that subjects with previous venous thrombosis had a similar risk for arterial thrombosis as those without antecedents of venous thrombosis, so there seems to be no association between venous thrombosis and the subsequent arterial thrombosis [14].
Only some studies and case reports have discussed the implication of trombophilic defects in arterial thrombosis. The results are controversial. In one cohort family study, the arterial events were diagnosed in 8% of the 144 subjects with protein C or S deficiencies and 1% from the 94 subjects with antithrombin deficiency [15]. In another ample study on carriers of familial thrombophilia (the European Prospective Cohort on Thrombophilia [EPCOT] study), overall annual incidences of myocardial infarction and/or ischemic stroke after 20 years of age were 0.15%, 0.18Z% and 0.15% in subjects with protein S (n=111), protein C, (n=150), and antithrombin deficiency (n=92), respectively [16]. A more recent study reported annual incidences of myocardial infarction and/or ischemic stroke of 0.32% (protein S), 0.32% (protein C) and 0.21% (antithrombin) in deficient subjects and 0.19% in non–deficient subjects >20 years of age [17]. In a case-control study, arterial thrombosis was recorded more frequently in 88 cases with protein S, protein C, or antithrombin deficiency (19% arterial thrombosis) compared with control subjects with venous thromboembolism without these deficiencies (1% arterial thrombosis) [17].
Lifelong systemic anticoagulation is the recommended treatment with emphasis of initiation towards symptomatic patients. The potential long term morbidity in young individuals must be recognized when discussing the long term risk and benefits of systemic anticoagulation.
This case report highlights that the diagnosis of protein C and S deficiency in young patients with myocardial infarction is essential for more appropriate management and prevention of recurrent events. Furthermore, family screening could lead to a prophylactic approach in carriers of this mutation. Patients and affected family members need to be informed of the risks, signs, and symptoms of thrombosis and the importance of prophylactic strategies. Education and counseling of the patient’s carrier status may also impact decisions about the indication of antithrombotic prophylaxis.
Conclusion
Hypercoagulable state caused by protein C and S deficiency without appropriate anticoagulant therapy can cause acute myocardial infarction in young adults with normal coronaries and without any underlying major risk factors for coronary artery disease. Raising patient awareness is paramount. Family screening could prevent catastrophic cardiovascular events.
References
- Bux-Gewehr I, Nacke A, FeurleGE (1999) Recurringmyocardial infarction in a 35 year old woman. Heart 81: 316-317.
- Sadiq A, Ahmed S, Karim A, Spivak J, Mattana J (2001) Acute myocardial infarction: A rare complication of protein C deficiency. Am J Med 110: 414.
- Tiong IY, Alkotob ML, Ghaffari S (2003) Protein C deficiency manifesting as an acute myocardial infarction and ischaemic stroke. Heart 89: E7.
- Peterman MA, Roberts WC (2003) Syndrome of protein C deficiency and anterior wall acute myocardial infarction at a young age from a single coronary occlusion with otherwise normal coronary arteries. Am J Cardiol 92: 768-770.
- Fournier JA, Cabezon S, Cayuela A, Ballesteros AM, Cortacero JAP, et al (2004) Long-term prognosis of patients having acute myocardial infarction when <40 years of age. Am J Cardiol 94: 989-992.
- Füllhaas JU, Rickenbacher P, Pfisterer M, Ritz R (1997) Long-term prognosis of young patients after myocardial infarction in the thrombolytic era. Clin Cardiol 20: 993-998
- Imazio M, Bobbio M, Bergerone S, Barlera S, Maggioni AP (1998) Clinical and epidemiological characteristics of juvenile myocardial infarction in Italy: the GISSI experience. G Ital Cardiol 28: 505-512
- Teixeira M, Sá I, Mendes JS, Martins L (2010) Martins Acute coronary syndrome in young adults. Rev Port Cardiol 29: 947-955
- Aguiar C (2010) Acute coronary syndrome in younger patients: an avoidable atherothrombotic complication. Rev Port Cardiol 29: 957-960
- Rallidis LS, Gialeraki A, Tsirebolos G, Tsalavoutas S, Rallidi M, et al. (2017) Prothrombotic genetic risk factors in patients with very early ST-segment elevation myocardial infarction. J Thromb Thrombolysis.
- Prandoni P, Bilora F, Marchiori A (2003) An association between atherosclerosis and venous thrombosis. N Engl J Med 348: 1435-1441.
- Sorensen HT, Horvath-Puho E, Pedersen L (2007) Venous thromboembolism and subsequent hospitalisation due to acute arterial cardiovascular events: A 20 year cohort study. Lancet 370: 1773-1779.
- Linnemann B, Schindewolf M, Zgouras D (2008) Are patients with thrombophilia and previous venous thromboembolism at higher risk to arterial thrombosis? Tromb Res 121: 743-750.
- Mahmoodi BK, Brouwer JL, Veeger NJ, van der Meer J (2008) Hereditary deficiency of protein C or protein S confers increased risk of arterial thromboembolic events at a young age: Results from a large family cohort study. Circulation 118: 1659-1667.
- Boekholdt SM, Kramer MH (2007) Arterial thrombosis and the role of thrombophilia. Semin Thromb Hemost 33: 588-596.
- Vossen CY, Rosendaal FR (2006) Risk of arterial thrombosis in carriers of familial thrombophilia. J Thromb Haemost 4: 916-918.
- Simioni P, Zanardi S, Saracino A (1992) Occurrence of arterial thrombosis in a cohort of patients with hereditary deficiency of clotting inhibitors. J Med 23: 61-74.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi