Research Article, J Pharm Drug Deliv Res Vol: 10 Issue: 3
A Comparison among Three Skin Preparations for the Transdermal Delivery of Vitamin B12 by Iontophoresis: A Novel Approach to Determine Systemic Absorption
Anton Sabiev1,2*, Mark A Korsten1,2,3 and William A Bauman1,2,3,4
1Veterans Affairs Rehabilitation Research & Development Service’s National Center for the Medical Consequences of Spinal Cord Injury, James J Peters VA Medical Center, Bronx, NY, United States
2Departments of Medicine, Medical Service James J. Peters VA Medical Center, Bronx NY, United States
3Departments of Medicine Medical Service James J. Peters VA Medical Center, Bronx NY, United States
4Rehabilitation and Human Performance, The Icahn School of Medicine at Mount Sinai, New York, United States
*Corresponding Author: Anton Sabiev National Center for the Medical Consequences of Spinal Cord Injury, James J. Peters VA Medical Center 130 West Kingsbridge Road Rm 7A-13, Bronx, NY 10468, United States, Telephone: +718584-9000, Ext. 1731, Fax: +718741-4675; E-mail: anton.sabiev@va.gov
Received: March 05, 2021; Accepted: March 19, 2021; Published: March 26, 2021
Citation: Sabiev A, Korsten MA, Bauman WA (2021) A Comparison among Three Skin Preparations for the Transdermal Delivery of Vitamin B12 by Iontophoresis: A Novel Approach to Determine Systemic Absorption. J Pharm Drug Deliv Res 10:3.
Abstract
Background: Poor skin permeability precludes the use of the transdermal route for the administration of most medications that require entry into the systemic circulation. However, charged compounds may be delivered systemically by Iontophoresis (ION). The relative safety and efficacy of the transdermal delivery of vitamin B12 (Methylcobalamin) by ION was determined by testing three different skin preparations. Subjects and Methods: Vitamin B12 15 mg was transdermally administered to 8 healthy subjects after the skin was prepared for ION delivery by three methods that were performed on each subject in a random order 1. Cleaning the skin with isopropyl alcohol (control) 2. Epilation followed by cleaning the skin with isopropyl alcohol 3. Pre-soaking the skin with oleic acid followed by cleaning the skin with isopropyl alcohol. The serum vitamin B12 concentration was determined by chemiluminescence methodology (Advia Centaur-XP). Blood was drawn immediately prior to and 10 min after each vitamin B12 administration, with the latter blood collection 30 min after the initiation of ION. The serum vitamin B12 absorbed systemically by transdermal ION was calculated from the measured rise in the serum concentration and the estimated blood volume. Results: The control group had an average of 5.8% (0.88 ± 0.90 mg; p<0.05) of vitamin B12 systemically absorbed. Epilation prior to ION was the most effective method to facilitate delivery of vitamin B12 with the average vitamin B12 systemically absorbed of at least 26.5% (3.97 ± 3.25 mg; p<0.005). The method of pre-soaking the skin with oleic acid was the least effective to promote absorption of vitamin B12 with 1.87% systemically absorbed (0.28 ± 0.28 mg; p<0.05). Minor, transient skin irritation was the only adverse reaction observed. Conclusion: Epilation prior to transdermal ION administration of vitamin B12 achieved the greatest delivery of agent of the three skin preparation methods tested. However, the transdermal administration of agent after only cleaning the skin with alcohol offered reasonably adequate systemic delivery with less preparatory effort and without the discomfort associated with epilation. Because of the variability in drug absorption among individuals, the anticipated systemic dose of a positively charged compound of similar molecular weight delivered by ION may be safely estimated by measuring the absorption of vitamin B12.
Keywords: Methylcobalamin; Vitamin B12; Iontophoresis; Epilation; Oleic acid, Skin permeability; Transdermal drug administration.
Abstract
Background: Poor skin permeability precludes the use of the transdermal route for the administration of most medications that require entry into the systemic circulation. However, charged compounds may be delivered systemically by Iontophoresis (ION). The relative safety and efficacy of the transdermal delivery of vitamin B12 (Methylcobalamin) by ION was determined by testing three different skin preparations.
Subjects and Methods: Vitamin B12 15 mg was transdermally administered to 8 healthy subjects after the skin was prepared for ION delivery by three methods that were performed on each subject in a random order 1. Cleaning the skin with isopropyl alcohol (control) 2. Epilation followed by cleaning the skin with isopropyl alcohol 3. Pre-soaking the skin with oleic acid followed by cleaning the skin with isopropyl alcohol. The serum vitamin B12 concentration was determined by chemiluminescence methodology (Advia Centaur-XP). Blood was drawn immediately prior to and 10 min after each vitamin B12 administration, with the latter blood collection 30 min after the initiation of ION. The serum vitamin B12 absorbed systemically by transdermal ION was calculated from the measured rise in the serum concentration and the estimated blood volume.
Results: The control group had an average of 5.8% (0.88 ± 0.90 mg; p<0.05) of vitamin B12 systemically absorbed. Epilation prior to ION was the most effective method to facilitate delivery of vitamin B12 with the average vitamin B12 systemically absorbed of at least 26.5% (3.97 ± 3.25 mg; p<0.005). The method of pre-soaking the skin with oleic acid was the least effective to promote absorption of vitamin B12 with 1.87% systemically absorbed (0.28 ± 0.28 mg; p<0.05). Minor, transient skin irritation was the only adverse reaction observed.
Conclusion: Epilation prior to transdermal ION administration of vitamin B12 achieved the greatest delivery of agent of the three skin preparation methods tested. However, the transdermal administration of agent after only cleaning the skin with alcohol offered reasonably adequate systemic delivery with less preparatory effort and without the discomfort associated with epilation. Because of the variability in drug absorption among individuals, the anticipated systemic dose of a positively charged compound of similar molecular weight delivered by ION may be safely estimated by measuring the absorption of vitamin B12.
Keywords
Methylcobalamin; Vitamin B12; Iontophoresis; Epilation; Oleic acid, Skin permeability; Transdermal drug administration.
Introduction
Transdermal delivery of medication offers the benefits of ease, safety and comfort of delivery that deedle-dependent administration methods often lack. Much of the time, the transdermal route is used to ensure an adequate concentration of medication at the local tissue site, but considerable uncertainty exists regarding the amount of agent absorbed both locally and into the systemic circulation. Only a few transdermally-administered drugs, such as nicotine, nitroglycerin, testosterone and fentanyl have been approved by the FDA for systemic therapy by passive diffusion. In this proof-of-principle study, the effects of three skin preparation approaches were tested for the ability of each of the methods to modify the efficiency of active transdermal administration of vitamin B12 (e.g., Methylcobalamin) mediated by Iontophoresis (ION). Theoretically, bypassing of epidermis through skin appendages such as hair follicles may facilitate transdermal delivery of medications. Hair epilation allows for open hair follicles to act as gateways to the follicular capillaries [1] improving absorption. Pre-soaking the skin with fatty acids has previously been reported to improve transdermal flux [2]. The two aforementioned methods of delivery of vitamin B12 were compared to the method of merely cleaning of the skin with isopropyl alcohol prior to application of the agent.
Methods
Vitamin B12, a charged compound with a molecular mass of 1,344 g, was employed as the test agent to quantify the changes in skin permeability to positively charged ions driven by ION into the systemic circulation under three different conditions. Vitamin B12 was chosen as the agent for the work reported herein because of its wide margin of safety, the ionic nature of the molecule, its availability, and the presence of reliable and readily accessible means to accurately determine its serum concentration.
Eight participants were recruited for this study, of which 7 were male and 1 was female, with ages ranging between 28 to 74 years old. The inclusion criteria parameters were: male or female between ages 18-80 years old. The exclusion criteria included history of ingrown hair, diabetes mellitus, allergies to substances employed, concurrent illness and pregnancy. The sequence of administration of each of the three methods of skin preparation for each individual was assigned in a random order by using a random digit table.
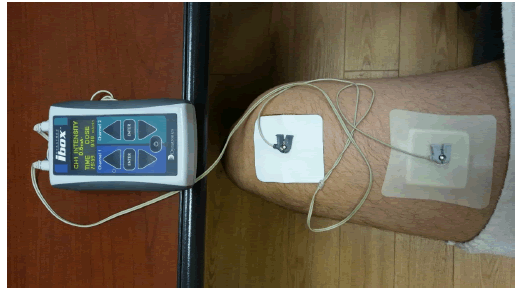
The primary outcome measure of this study was the dose of vitamin B12 systemically absorbed by ION for each of the skin preparation methods performed, as determined by the increase in the serum concentration of the agent. The three methods used to prepare the skin under the positive electrode that delivered the vitamin B12 were: 1. Cleansing of the skin with 70% Isopropyl alcohol (control), 2. Cleansing of the skin with 70% isopropyl alcohol followed by hair removal by epilation, 3. cleansing of the skin with 70% isopropyl alcohol followed by soaking the skin with oleic acid (oleic acid) [2-5]. To remove variability prior to performing each of the three methods of pre-treatment of the skin before application of vitamin B12, the skin was wiped with 70% isopropyl alcohol, sprayed with a thin layer of 20% benzocaine (Americaine aerosol spray) and covered with an occlusive plastic film for 10 min to allow for the benzocaine to exert its analgesic action; after which the skin was wiped with a deionized water-moistened paper towel, followed by dry paper towel and then followed by wiping with 70% isopropyl alcohol. The second skin area (7 × 7 cm) was cleansed with alcohol and 0.5 ml of 1.0% citric acid dissolved in 0.9% normal saline solution prior to placement of the negative electrode (cathode) to the inner knee region approximately 10 cm from the edge of the positive therapy electrode (anode) to complete the electrical circuit (Figure 1).
The control skin cleansing approach without any additional intervention has been previously described for the skin preparation prior to the placement of the anode and cathode patches. The epilation approach, after cleansing the skin with a 70% isopropyl alcohol pad, epilation (Remington EP 7030 epilator) from an area of approximately 5 × 5 cm (2 × 2 inches); the depilated area was then covered with a thin layer of 0.2% sodium lauryl sulfate in de-ionized water prior to placement of the anode patch. The oil soaking approach used a thin layer of oleic acid to bathe the skin for 40 min before wiping it from the skin with a paper towel and then cleansing the area with a 70% isopropyl alcohol pad prior to placement of the anode patch. An elevated room temperature (73°F-76°F) was maintained during all Ion sessions to minimize peripheral vasoconstriction and assure adequate blood flow in the dermal capillaries. Vitamin B12 was applied under the anode electrode patch, which in turn was attached to the prepared skin on the anterior thigh region.
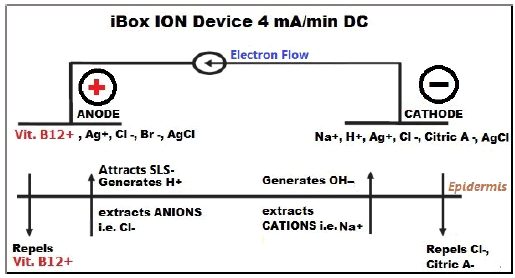
ION is a non-invasive drug delivery method whereby a molecular ion is repulsed by a weak electric field to permit penetration of the stratum corneum (Figure 2).
The technique of ION was modified in the same manner for all three methods tested to decrease skin irritation, improve thermochemical safety, and to maximize the drug dose delivered into the systemic circulation. Vitamin B12 (15 mg) was dissolved in 4 ml of deionized water, soaked into the anode patch reservoir, which was applied to the prepared patch of skin. The ION technology employed consisted of Dynatron® iBox™ (Salt Lake City, Utah) that delivered an electric current of 4.0 mA/min for 20 min through the skin [6]. The iBox™ ION device was attached to the electrode patches that were in contact with the skin by wire leads [7] a multimeter was attached to the electrodes in parallel to record the voltage required to deliver 4 mA/min, overcoming the innate electrical resistivity of the skin during ION. Subjects were queried for the presence of any sensations associated with ION at regular intervals throughout the procedure.
Blood was collected prior to ION and then again 30 min after initiating ION, which was 10 min after completion of administration of vitamin B12 by ION. The blood was centrifuged for 5 min at 2,400 RPM with the formed blood cell elements removed and the serum delivered to the clinical laboratory for automated measurement of vitamin B12 by chemiluminescence (Advia Centaur-XP). The amount of vitamin B12 delivered into the systemic circulation was based on the subject’s blood volume that was estimated using an online calculator [8] The distribution of vitamin B12 into extravascular body compartments was not taken into consideration in the calculation of the total amount of agent delivered transdermally, which then would have resulted in a greater dose being absorbed than that being reported herein due to the unavoidable distribution of the agent to connective tissues, visceral organs and its urinary excretion.
This study was approved by the Institutional Review Board of the James J Peters VA Medical Center (JJP VAMC). Signed informed consent was obtained from each subject prior to participation.
The increase in the serum concentration of the vitamin B12 from the baseline serum concentration was determined after epilation, oil soaking and control methods. Mean, standard deviation and the pvalue were calculated for the serum concentrations of vitamin B12 following ION under each of the three skin preparatory approaches using an online statistical calculator [9]. Because the serum vitamin B12 concentration could only increase or stay the same, a one-tailed Ttest was used to determine the presence of a significant difference between the two means. The results with a p-value of <0.05 being deemed sufficient to reject the null hypothesis of no difference in serum vitamin B12 levels following ION after different skin preparations. A one-way ANOVA was applied to determine if a significant difference in absorption of agent was present among the serum vitamin B12 levels after each of the three skin preparation approaches.
Results
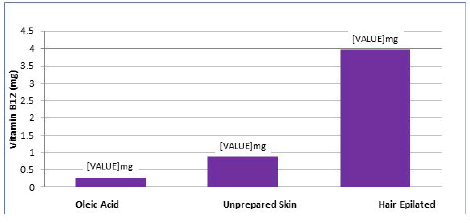
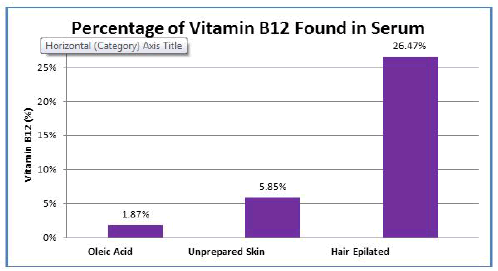
Of the 8 subjects who were recruited for this study, all 8 subjects completed the ION delivery of vitamin B12 for each of the three skin preparations. The group that had the control skin preparation showed a modest, but statistically significant, increase in the concentration of serum vitamin B12 after ION administration. The mean increase in vitamin B12 was 0.88 ± 0.90 mg, or 5.85% of the applied dose delivered into the systemic circulation (Figures 3 and 4) (p<0.05). Epilation was associated with the greatest increase in serum concentration of vitamin B12 after ION. An average of 3.97 ± 3.25 mg or 26.47% of the applied dose was absorbed (p=0.005) (Figures 3 and 4). Of note, in two subjects the serum vitamin B12 concentration exceeded the maximum threshold of detection (>2000 mcg/mL). Thus, the average absorption of vitamin B12 was obviously greater than the 3.97 ± 3.25 mg reported above. The preparation method of initially soaking the skin with oleic acid was associated with 0.28 ± 0.27 mg of vitamin B12 absorbed or 1.87% of the applied dose (Figures 3 and 4), which was the least amount absorbed of the three methods tested (p<0.05).
ANOVA analysis of the increase in mean serum concentrations of vitamin B12 after each of the three skin preparations had an f-ratio value of 8.76532 with a p<.005. Significant differences (p<0.05) were found for each of the comparisons among the methods applied.
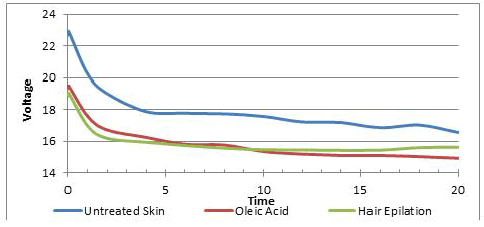
Monitoring the electric activity of the I-Box, during all three experiments, a consistent trend was observed, presenting as an initially-steep downward slope in the magnitude of voltage that gradually flattened-out, representing the voltage required to maintain the electric current at constant 4 mA/min (Figure 5).
The control method had the highest initial skin resistance of 5734 Ohm with an average voltage of 22.9 V at the outset of ION, following an average trend of decrease to 4541 Ohm of resistance and 16.6 V at 20 min of ION. The second-highest initial skin resistance observed was with the oleic acid method, showing an average initial resistance of 4878 Ohm and voltage of 19.5 V, with average values of 4006 Ohm and 14.9 V at 20 min of ION. With the epilation method, the initial resistance was 4768 Ohm and voltage of 19.1 V. All three curves for resistance followed a steady downward asymptotic trajectory from the onset of ION.
When prompted to report sensations at regular intervals, no subject complained of pain or other untoward sensations anywhere, including at the site of electrode attachment. There was no swelling, burns or infections related to the ION procedure. Upon removal of electrode patches, blanching erythema was invariably present, silhouetting the areas of contact of both positive and negative electrode patches. The electrode patch-shaped erythema resolved completely within one hour of removal of the anode patch and within 3 h of removal of the cathode patch. Punctate salmon red staining due to absorption of B12 was pronounced and almost uniformly present in the skin footprint of the anode patch of each subject in the epilation group, which faded completely over the ensuing 3-5 days; in the oleic acid group, the skin staining was absent or light in coloration; in the control group, the skin staining was moderately present in 6 of 8 subjects and faded completely over the ensuing 2-3 days. No signs or symptoms of skin infection or damage of any type were observed or reported on questioning at 24 or 48 h after ION.
Discussion
The current clinical utility of ION as a modality for drug delivery is predominantly restricted to the local tissue delivery of glucocorticoids for the management of painful muscle and joint conditions associated with inflammation. The benefits of ION in delivery of agents into the systemic circulation include avoiding first pass hepatic metabolism, which occurs with oral medications; absence of the discomfort associated with puncturing of the skin with needles and avoidance of stress that people with hypodermic needle phobia experience on sight or feel of a needle. Transdermal delivery of sumatriptan by ION for treatment of migraine headaches was initially approved but the approval was later withdrawn by the FDA [10]. Fentanyl has received FDA approval to be administered by ION relief of pain [11].
In this study, the primary endpoint was the amount of vitamin B12 delivered into the systemic circulation, which was observed to be depend upon the skin preparation employed. We have conducted this work in order to develop and test an improved method of ION to be used in follow-on research of the systemic absorption and effects of other agents delivered via ION. Due to the significant differences in absorption observed for the three skin preparations performed, the results reached statistical significance with a relatively-small number of subjects in each group.
Hair epilation was found to be the superior method of skin preparation for ION of the three approaches tested. It may be noted that mere skin cleansing resulted in the systemic absorption of 5.4% of the vitamin B12 dose applied to the skin. Several subjects undergoing skin epilation had few to no hair on their legs, which appeared to be somewhat related to a lower amount of vitamin B12 delivered systemically for those individuals. Of note, after hair epilation, two of the subjects had such fine absorption of vitamin B12 that the resulting serum concentration exceeded the upper threshold of detection.
To our knowledge, no prior report has observed that hair epilation enhanced the transcutaneous delivery of an ionic substance by ION. Limited literature exists in support of bathing the skin with fatty acids to facilitate ION delivery of agents. Rat skin pretreated with various fatty acid preparations, including oleic acid, increased the flux of Arginine Vasopressor (AVP) in comparison to skin not pretreated with the enhancer and, furthermore, oleic acid in combination with ION significantly increased the permeation of AVP in comparison to pretreatment with fatty acids and ION alone; as determined by Fourier transform infrared spectroscopy, oleic acid interacted with the skin lipids to cause fluidization of stratum corneum lipids and disruption of the its lipid lamellae [12] Enhancement of ION flux across rat and porcine skin by unsaturated fatty acids of insulin [13,14] and midodrine hydrochloride have been reported [15]. However, despite these prior favorable findings regarding pre-treatment with fatty acids to facilitate absorption, the current study demonstrated that bathing the skin with oleic acid markedly decreases, and certainly does not increase, transcutaneous absorption of vitamin B12 by ION, with only an average of 1.87% absorbed systemically.
In prior work by the authors, the objective was maximizing transcutaneous absorption of fairly small-sized, positively charged compounds with the objective to administer a dual drug combination, neostigmine and glycopyrrolate, to induce a safe, predictable, and relatively rapid bowel evacuation. Our initial work was performed by preparing the skin with oleic acid, which provided an approximately 56% rate of success in inducing a bowel evacuation (10 of 18 subjects) in those subjects who were previously shown to respond to intravenous administration of neostigmine with bowel evacuation [16]. However, in subsequent work in which application of these medications was performed without bathing the skin in an oil, greater than a 90% efficacy of bowel evacuation was achieved [17] a finding that is consistent with the findings of our study herein.
This work was performed to test the comparative safety and efficacy of different preparatory approaches for the transdermal delivery of an agent by ION. However, there exists individuals who have pernicious anemia and are unable to absorb vitamin B12 orally but have a fear of needles known as trypanophobia. Because the Recommended Daily Allowance (RDA) for vitamin B12 is 2.4-2.8 μg [18] and because approximately 880 μg was delivered systemically with no prior skin preparation (the mean value absorbed that is over 300-times higher than the minimal RDA for adults), this route of administration for vitamin B12 would be sufficient for the treatment of vitamin B12 deficiency. Of consideration, intravenous delivery of vitamin B12 to achieve serum concentrations in excess of 300-1000 ng/ml, which is the maximum concentration that can be bound by serum proteins [19] thus resulting in the rapid urinary excretion of excess vitamin.
The absence of skin preparation other than superficial cleansing prior to ION appears to be the most viable option for general clinical application because of its simplicity, ease of use, negligible time to perform and, for many agents, an adequate delivery into the circulation. Epilation, despite delivering a several fold higher amount of vitamin B12 into circulation, would likely result in poorer patient compliance because of increased time to perform and the discomfort associated with a more complicated procedure.
Given the observed variability of absorption among subjects with varying amounts of hair and differing dermal microvasculature density and health, the dose of a positively charged ionic substance of similar molecular weight (e.g., drug) that can be anticipated to be delivered via ION may be safely estimated for each patient by using the absorption of vitamin B12 as a surrogate agent.
Conclusion
The safe systemic delivery of vitamin B12 by ION was demonstrated by all methods tested. The epilation method of skin preparation was the most efficient means to deliver vitamin B12 into the systemic circulation followed by merely cleansing the skin, which resulted in adequate absorption of vitamin B12. An unanticipated finding was that bathing the skin in a fatty acid solution proved to be the least effective approach and appeared even to impede absorption despite literature to the contrary that supported its use. The work presented employed vitamin B12 as a prototypical, positively charged agent to test the efficacy of its transdermal absorption by ION without regard to its potential therapeutic value. However, because of the convenience and relative efficacy of the transdermal systemic delivery of vitamin B12 by ION after only cleaning the skin with an alcohol pad, this approach may be considered as a viable administration route in treatment of vitamin B12 deficiency states in patients who are needle-adverse.
Contributions
This research was supported by the Department of Veterans Affairs Rehabilitation Research and Development Service (#B9212-C) and the James J. Peters VA Medical Center. Dr. William A. Bauman is the guarantor of this submission. Dr. Bauman assisted with protocol design, protocol implementation and the preparation of the manuscript. Dr. Anton Sabiev was responsible for protocol design, subject recruitment, protocol implementation, and the preparation of this manuscript. Dr. Mark A Korsten assisted in the conceptualization of the protocol design and the preparation of this manuscript. All authors listed on this study have read and approved the final version being submitted for your consideration.
Conflicts of Interest
The authors have no conflicts of interest.
Funding
Department of Veterans Affairs Rehabilitation Research and Development Service. National Center for the Medical Consequences of Spinal Cord Injury (#B9212-C).
References
- Grace H, Daniel B (2000) An unexpected finding in percutaneous absorption observed between haired and hairless guinea pig skin. J Pharm Sci 86: 398-402
- Wang Y, Fan Q, Song Y, Michniak B (2003) Effects of fatty acids and iontophoresis on the delivery of midodrine hydrochloride and the structure of human skin. Pharm Res 20: 1612-18.
- Rastogi SK, Singh J (2005) Effect of chemical penetration enhancer and iontophoresis on the in vitro percutaneous absorption enhancement of insulin through porcine epidermis. Pharm Dev Technol 10: 97-104.
- Pillai O, Panchagnula R (2004) Transdermal iontophoresis of insulin. Influence of pretreatment with fatty acids on permeation across rat skin. Skin Pharmacol Physiol 17: 289-97.
- Nair V, Panchagnula R (2003) Effect of iontophoresis and fatty acids on permeation of arginine vasopressin through rat skin. Pharmacol Res 47: 563-9.
- IBOX, Dynatron ibox™ 2 made by Dynatronics Corp. 7030 Park Centre Drive, Salt Lake City, UT 84121.
- NEW: ionto⁴ Iontophoresis Electrodes, Richmar.
- https://reference.medscape.com/calculator/648/estimated-blood-volume
- https://www.socscistatistics.com/tests/tsinglesample/default2.aspx
- Garnock-Jones KP (2013) Sumatriptan Iontophoretic transdermal system: a review of its use in patients with acute migraine. Drugs 73: 1483-90.
- Power I (2007) Fentanyl HCl Iontophoretic Transdermal System (ITS): clinical application of iontophoretic technology in the management of acute postoperative pain. Br J Anaesth 98: 4-11.
- Nair VB, Panchagnula R (2003) Effect of iontophoresis and fatty acids on permeation of arginine vasopressin through rat skin. Pharmacol Res 47: 563-9.
- Pillai O, Panchagnula R (2004) Transdermal iontophoresis of insulin.VI.Influence of pretreatment with fatty acids on permeation across rat skin. Skin Pharmacol Physiol 17: 289-97.
- Rastogi SK, Singh J (2005) Effect of chemical penetration enhancer and iontophoresis on the in vitro percutaneous absorption enhancement of insulin through porcine epidermis. Pharm Dev Technol 10: 97-104.
- Wang Y, Fan Q, Song Y, Michniak B (2003) Effects of fatty acids and iontophoresis on the delivery of midodrine hydrochloride and the structure of human skin. Pharm Res 20: 1612-18.
- Korsten MA, Lyons BL, Radulovic M, Cummings TM, Sikka G, et al. (2018) Delivery of neostigmine and glycopyrrolate by iontophoresis: a nonrandomized study in individuals with spinal cord injury. Spinal Cord 56: 212-217.
- Sabiev AV, William AB, Shahzad S, Ann M, Christopher MC et al. (2019) Transdermal administration of neostigmine and glycopyrrolate by Iontophoresis decreases time of bowel care and increases completeness of bowel evacuation in persons with chronic constipation secondary to spinal cord injury. J Clin Med 10: 1655.
- Institute of Medicine Dietary Reference Intakes: Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic acid, Biotin, and Choline. Washington (DC): National Academies Press; 2000.
- Mollin DM, Ross GIM (1953) Vitamin B12 Concentrations of serum and urine in the first 72 hours after intramuscular injections of the Vitamin B12. J Clin Pathology 6: 54–61.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi