Research Article, J Otol Rhinol Vol: 7 Issue: 6
A National Survey on CO2 Transoral LASER Surgery amongst 57 UK Otolaryngologists
Kanona H1*, Farrell R1, Oswal RV2 and Tatla T1
1Northwick Park Hospital, London West Healthcare NHS Trust, Harrow HA1 3UJ, UK
2James Cook University Hospital, Middlesbrough, UK
*Corresponding Author : Hala Kanona
Northwick Park Hospital, London West Healthcare NHS Trust, Harrow HA1 3UJ, UK
E-mail: hkanona@yahoo.co.uk
Received: October 16, 2018 Accepted: November 08, 2018 Published: November 15, 2018
Citation: Kanona H, Farrell R, Oswal RV, Tatla T (2018) A National Survey on CO2 Transoral LASER Surgery amongst 57 UK Otolaryngologists. J Otol Rhinol 7:6. doi: 10.4172/2324-8785.1000359
Abstract
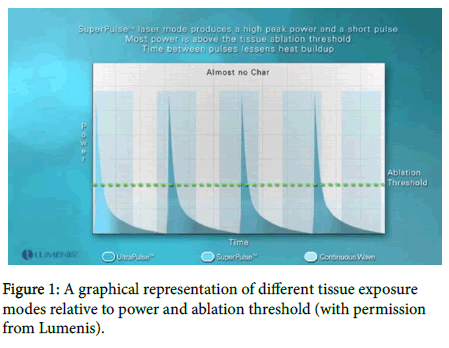
Objectives: To capture information on clinical practice using the CO2 LASER within the upper aerodigestive tract (UADT). Design: A 21 item structured questionnaire survey was sent to consultant-only ENT UK members over a 2-month period between March and May 2017 Main Outcome Measures: Variation in CO2 LASER practice with reference to subspecialty, clinical setting, LASER type, power settings, operating modes and tissue exposure modes. Results: 57 responses were received from consultants working in hospitals across the UK. The commonest indication for transoral LASER surgery (TOLS) was excision of cancer (57.1%) and the most common area of surgery performed was within the larynx (60.4%). See Figure 1 for variation in LASER operating modes. Over 95% of hospitals carry out LASER safety practices. Conclusion: A wide variation in the use of CO2 LASER exists amongst UK Otolaryngologists. The development of new guidelines may promote effective use and minimise avoidable trauma or complications.
Keywords: Survey; LASER Surgery; Otolaryngologists
Introduction
LASER applications
The use of the CO2 LASER covers many areas of practice within Otolaryngology. As well as acting as a workhorse for complex head and neck cancer resection [1], the CO2 LASER is also used to treat benign conditions such as snoring and OSA, where focus is mainly on the soft palate and tongue base. Extended applications in the treatment of other disease such as pharyngeal strictures, pouches or webs may also be used [2-4].
Physics of the CO2 LASER
With a wavelength of 10.6 micrometres, the CO2 LASER has a high coefficient of absorption for water and therefore causes vaporisation of tissues with high water content. Within ENT surgery, CO2 LASER application often involves the excision of lesions within the UADT via surgical incisions to enable removal of tumours, vaporisation of surface lesions and/or coagulation of small bleeding vessels.
The CO2 LASER has 2 main operator modes: continuous wave and pulsatile. In continuous wave mode the LASER delivers a constant stream of energy during depression of the foot pedal. This delivers a high average power, but is less accurate in energy delivery compared to the pulsatile mode. Pulsatile modes (e.g. pulser or superpulse), emit much shorter pulses of energy and have variable pulse durations thereby delivering variable amounts of energy to tissue e.g. pulser at 2-25 milliseconds versus superpulse at 200-1000 microseconds. Pulsatile mode is often used when precise control is necessary. The ultrapulse has been more recently developed to deliver a lower peak power compared to that of superpulse (200 Watts vs. 400-500 Watts respectively), and allows more energy delivery over a longer time [5]. Compared to superpulse, the ultrapulse mode can also ablate tissue more readily because each pulse reaches an ablation threshold, compared to superpulse where pulses may exceed the ablation threshold, but a higher energy in shorter bursts are delivered that may lead to thermal damage (Figure 1) [6].
The micromanipulator attaches to the microscope providing beam sizes that range from 250 microns at a focal length of 400 mm. The scanner connects between the articulating arm of the microscope and the micromanipulator and contains software that allows selection of various spot sizes, depth of tissue penetration (0.2-2 mm) and beam shape, all of which can be modified by the operator. Energy delivery can also be influenced by the degree of tissue exposure modes including continuous, repeat pulse or single pulse.
Surgical guidance for LASER use
Although the first clinical use of the CO2 LASER within the larynx was described by Strong and Jacko over 40 years ago [1,5,7] to date, there are no published guidelines on the practical application of LASER in terms of selection of LASER type, optimal power settings or suitable exposure modes for use in different tissues within the UADT. As a consequence of this, clinical practice amongst ENT Surgeons is likely to vary widely.
Aim of the Study
The aim of this survey is to capture information on the clinical use of CO2 LASER applied to tissues of the UADT. In establishing a baseline of practice, we hope to extend our focus to examine more specific areas of CO2 LASER use, for example in the treatment of glottic cancer, in order to develop new standards for LASER practice within Otolaryngology.
Materials and Methods
Design
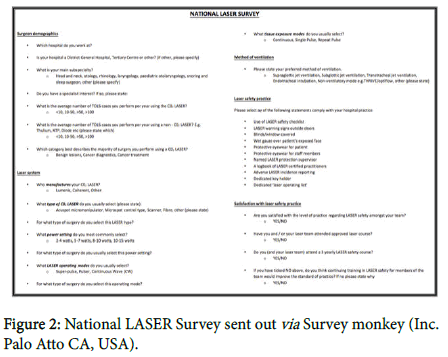
A 21-item structured survey was sent to consultant-only ENT UK members over a 2-month period between March and May 2017 (Figure 2). Surveys were created on the online platform Survey Monkey (Inc. Palo Atto CA, USA) and were distributed by a communications administrator to consultant-only members of ENT UK.
Main Outcome Measures
Main outcome measure was to assess variation in CO2 LASER practice with reference to LASER type, power settings, operating modes and tissue exposure modes. LASER safety practice was also measured.
Ethical approval
Not required.
Results
Responses to survey
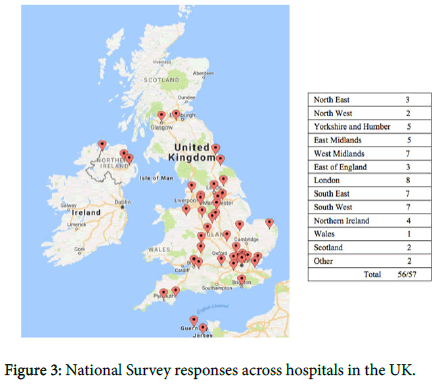
Seven hundred and eighty-one surveys were emailed to consultant members of ENT UK. Two hundred and eighty-seven surveys were opened and 57 responses were received. The average response rate per question was 84.5% equating to an average of 48/57 responses per question. Figure 3 illustrates the distribution of responses received from surgeons working in different hospitals across the UK.
Surgeon demographics
Forty-eight percent of surgeons work in a tertiary centre and 52% in a district general hospital. See Table 1, for the breakdown of surgical subspecialties and specialist interests amongst surgeons using the CO2 LASER.
| Main surgical specialty | % | Specialist interest | % |
|---|---|---|---|
| Head and Neck | 55.6 | Head and Neck | 35.5 |
| Otology | 18.3 | Phonosurgery/laryngeal/voice | 29 |
| Laryngology | 13.0 | Cholesteatoma and stapes | 16.1 |
| Rhinology | 5.6 | TOLS+/-robotics | 9.7 |
| Paediatric ENT | 3.7 | Airway | 6.5 |
| Sleep and snoring | 1.9 | Sleep and snoring | 3.2 |
| General ENT | 1.9 | ||
| Total: | 100 | Total: | 100 |
Table 1: The breakdown of surgical subspecialty and specialty interest amongst ENT surgeons using the CO2 LASER.
Over 94% of ENT surgeons use the CO2 LASER compared with 89% that use the non CO2 LASER. See Table 2, for the estimated range of TOLS cases performed annually per surgeon using the CO2 and non CO2 LASER. Indications for TOLS surgery with the CO2 LASER include cancer treatment (57.1%), surgery for benign lesions (36.7%) and diagnostic surgery (10.2%).
| Estimated case range | <10 Cases | 10-50 Cases | >50 Cases | >100 Cases |
|---|---|---|---|---|
| CO2 LASER (%) | 36.3 | 49.1 | 10.9 | 3.6 |
| Non CO2 LASER (%) | 90.2 | 7.8 | 1.9 |
Table 2: The estimated range of TOLS cases performed annually per surgeon using the CO2 and non CO2 LASER.
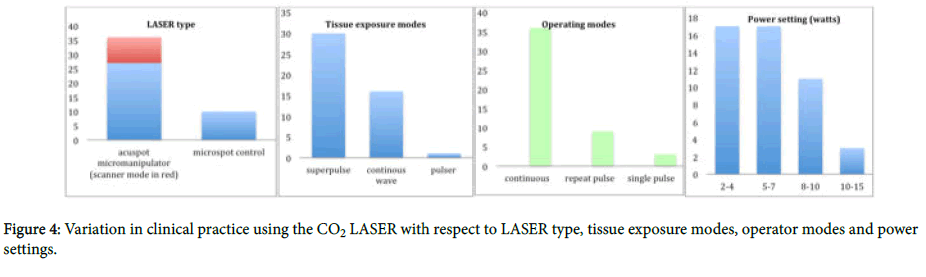
LASER systems
LASER manufacturers differed between hospitals with 78.4% using Lumenis®, 13.5% Coherent, 5.4% Sharplan and 2.7% Aesculap Meditec. Variation was seen across all operator settings with clinical use of the CO2 LASER including LASER type, power setting, operating mode and tissue exposure mode (Figure 4).
On average, LASER surgery was performed most commonly within the following anatomical sites within the UADT: larynx (60.4%), larynx and oropharynx (12.5%), larynx, pharynx and oral cavity (14.6%) and ‘other’ (12.5%) including only specific operations such as laryngoecele excision, palatal reduction, and tonsillectomy.
Method of ventilation
Preferred methods of ventilation for surgery include endotracheal intubation (52.4%), supraglottic jet (23.8%), subglottic jet (16.7%), transtracheal jet (4.8%) and opitflow™/Transnasal Humidified Rapid- Insufflation Ventilatory Exchange (THRIVE) (2.4%).
LASER safety
Over 95% of hospitals carry out the following LASER safety practices: LASER warning signs outside doors, wet gauze over patient’s exposed face, protective eyewear for staff members and named LASER protection supervisor. For breakdown of LASER safety practices across the UK, see Table 3. Ninety-four percent of consultants were satisfied with the level of safety practice within their team and 98% had attended a LASER safety course at some point. Only 21 surgeons (38.9%) had attended a 3 yearly LASER course and over 50% of consultants who did not attend a refresher course, did not feel that continued training in LASER safety would improve practice further.
| LASER safety practices | |
|---|---|
| LASER warning signs outside doors | 100.00% |
| Protective eyewear for staff members | 100.00% |
| Wet gauze over patient’s exposed face | 98.00% |
| Named LASER protection supervisor | 96.10% |
| Blinds/window covered | 94.10% |
| Use of LASER safety checklist | 90.20% |
| A logbook of LASER certified practitioners | 88.20% |
| Adverse LASER incidence reporting | 82.40% |
| Dedicated key holder | 70.60% |
| Protective eyewear for patient | 60.80% |
| Dedicated ‘LASER operating list’ | 37.30% |
Table 3: LASER safety practices within hospitals across the UK.
Discussion
Summary of findings
Various regions from across the United Kingdom were successfully captured in this national survey, however, only 7.3% from a total of 781 ENT UK members responded to the emailed survey.
Comparison with other studies
LASER settings: Our results demonstrate a wide variation in the use of CO2 LASER with respect to task-specific application. A range of LASER types and settings applied to different tissues within the UADT can give rise to a myriad of energy levels that can be delivered to tissue. The most common type of LASER used was the acuspot micromanipulator (73%) with or without the use of the scanner mode, followed by microspot control (27%). The acuspot micromanipulator is a newer generation machine that achieves a minimum spot size of 250 microns at a 400 mm focal length and has advantages over the traditional microspot control with regards to better light transmission and elimination of aiming beam errors that can occur within the operator field [8].
The most frequent power settings selected for individual surgical procedures were between 2 and 4 watts (35.4%) and 5 and 7 watts (35.4%). This however, in the context of other LASER settings (such as operating modes and tissue exposure modes), is meaningless in relation to actual extent of energy delivered to tissue. Our results demonstrate that surgery was most commonly performed for cancer treatment (57.1%), on the larynx (60.4%), using the superpulse operating mode (63.8%) with a continuous tissue exposure mode (75%). Although we are unable to prove that these settings were used in combination during surgery, these settings seem appropriately suitable for this type of surgery that aims to incise tissue (e.g. cancer resection within the larynx). This reflects an understanding of basic LASER physics and application to different tissues. This has also been illustrated by comments from responders of the survey…. “Small setting for larynx, bigger pharyngeal resection requires higher setting…..”I select the beam shape and depth of penetration and the power is determined for me”…..”older LASERs require a higher setting, newer LASERs require a lower setting.” By comparison, some surgeons chose arbitrary power settings to operate on different tissue types without any consistency in the selection of operating modes and power settings…..”my settings range from 1-10 watts even for a small case…..”I use 4 watts for the larynx, 7 watts for the rest.”
It is therefore imperative that prior to performing surgery with the CO2 LASER, one must first decide on whether the objective of surgery is to excise or debulk a tumour (e.g. a large supraglottic cancer), or perform non-ablative surgery on a superficial lesion (e.g. a vocal cord papilloma) to help guide the appropriate LASER setting. It is also important for the operator to consider minimizing the extent of thermal damage to the target and surrounding tissues by selecting an appropriate operator mode (such a superpulse), which can allow sufficient thermal relaxation time (time for tissue to lose 50% of its heat through diffusion) prior to performing surgery [9]. This, for example can be vital in cases where collateral damage to tissue may have detrimental effects on surgical outcome e.g. removal of a benign vocal cord lesion in professional voice user. The average zone of thermal damage after LASER energy to soft tissue is <0.6 mm [10-12]. Another consideration relates to coagulation which relies upon defocussing the LASER beam to achieve successful haemostasis in blood vessels that are up to 0.5 mm in size [13-16].
Consideration of all of the above factors can be challenging. Within the literature, some surgeons that operate on large cohorts of patients using the CO2 LASER have recommended task-specific LASER settings, however no consensus has been made. For example Oswett et al. specify that the lowest power setting should be used for all types of phonosurgery, compared with Shapshy and Rebeiz who recommend a spot size of 0.3 mm and power settings between 1 and 3 watts with intermittent pulses of 1/10 per second [3,4], Power expressed without power density has very little relevance to the total energy delivered by the LASER to the tissue 1. Knowledge and understanding of the concept of ‘radiant exposure’ (power density × time), tissue interaction, mode of transmission, delivery systems and LASER settings are crucial to achieving the optimum results and correct application of the LASER in surgery. Lack of understanding can lead to incorrect use of the LASER and may increase the chances of avoidable complications [3].
LASER Training
The LASER safety protocols have been introduced since the 1980’s [17]. During this time, the biggest hazard documented was LASER fire [18] and evidence has shown that regular rehearsal and training reduced the incidence of this significantly [17].
There are no specific guidelines on the frequency of attending LASER courses. Interestingly, comments from our survey by surgeons who did not attend a regular LASER course stated that “safety should become a way of life without a period of reinforcement”. Others felt that on-going in-house training was part of their standard practice and therefore, there was no need for refreshing by attending the LASER course again. Finally, some respondents simply mentioned that there had been no LASER safety events and therefore there was no need for attending annual courses.
The UK consensus statement published in 2009 on the ‘transoral LASER assisted microsurgical resection of early glottis cancer’ does recommend the acquisition of LASER skills through continuing educational courses using laryngeal dissection and mannequin [19,20]. Similarly, official guidance published by the British Standards 2004 on the ‘Safety of LASER products: A user’s guide’ specifies that “instruction and training should be completed prior to operating or working with LASER products and repeated as frequently as necessary in order to ensure continuing compliance with safety practices”6. In addition, the Department of Health stipulates that all hospitals where LASERs are used should have local rules governing safe use in accordance with their guidance [21]. Detailed guidance on clinicianspecific training found in the published document Quality Control, safety standards and regulations (written for the American Association of Physicists in Medicine and the American College of Medical Physics), advocates the credentialing of physicians following didactic LASER teaching for a minimum of 8 hours, 4 hours of direct hands-on LASER use in the lab as well as experience of performing at least 3 cases utilising a specific type of LASER in an assistant or primary role. These credentials get sanctioned by a LASER committee and must be issued prior to being able to operate the LASER independently [22].
For those surgeons who feel that ongoing LASER safety training may be of limited use practically, it may provide learning opportunities through discussion of LASER complications and ‘near misses’. In addition, in the event of a surgical complication, attendance to courses can be vital with respect to providing medico-legal defence.
Limitations of study
We were unable to demonstrate the proportion of Head and Neck Consultants that were captured within our survey. This is unfortunate as this is the group most likely to use the CO2 LASER and thus provide more abundant information on this topic. During the process of analysing survey responses, it was noted that one surgeon commented that they were unable to complete the survey, as they did not have a CO2 LASER at their institution. Regrettably, no information of the availability of CO2 LASERS to Head and Neck surgeons was assessed.
Conclusion
Although most new LASER manufacturers provide a rough guide to power settings (for example Lumenis® machines recommend a power setting of 10 watts for use in the larynx), there are no task-specific LASER setting recommendations published. It should be considered that with such wide variation between CO2 LASER practice amongst UK surgeons (as demonstrated by our survey), prescriptive taskspecific guidance with regard to appropriate LASER settings minimise incorrect use of the LASER and achieve optimum results through and correct application of the LASER. As technology advances and extended uses of the LASER with robotics develops, it will be imperative that surgeons receive proper training to enable a firm foundation of knowledge in LASER physics an application before these advances can be made, as well as being confidently embraced by all surgeons who wish to use it.
Acknowledgments
Phillppa Chinery, Communications Administrator at ENT, for her help in the management and distribution of the survey.
References
- Oswal V, Remacle M, Jovanvic S, Krespi JP, Zeitels SM, et al. (2014) Principles and Practice of Lasers in Otorhinolaryngology and Head and Neck. (2nd Edtn) Kugler Publications, Amsterdam. Netherlands.
- Amir I, Vernham GA (2015) Audit of transoral laser-assisted microsurgical resection of early laryngeal cancer. J Laryngol Otol 129: 372-376
- Shapshap S, Rebeiz E (1997) Lasers in Otolaryngology. In: Cummings C (ed) Otolaryngology Head and Neck Surgery, Elsevier Mosby, Philadelphia, pp: 2136.
- Ossoff RH, Coleman JA, Courey MS, Duncavage JA, Werkhaven JA, et al. (1994) Clinical applications of lasers in otolaryngology-Head and neck surgery. Lasers Surg Med 15: 217-248
- Strong MS, Jako GJ (1972) Laser surgery in the larynx. Early clinical experience with continuous CO2 laser. Ann Otol Rhinol Laryngol 81: 791-798
- Introducing the Acupulse Fractional C02 Laser.
- Outzen KE, Illum P (1995) CO2-laser therapy for carcinoma of the larynx. J Laryngol Otol 109: 111-113
- Ossoff RH, Werkhaven JA, Raif J, Abraham M (1991) Advanced microspot microslad for the CO2 laser. Otolaryngol Head Neck Surg 105: 411-444
- Yan Y, Olszewski AE, Hoffman MR, Zhuang P, Ford CN, et al. (2010) Use of lasers in laryngeal surgery. J Voice 24: 102-109
- Wilder-Smith P, Arrastia M, Liaw LH, Berns M (1995) Incision properties and thermal effects of three CO2 lasers in soft tissue. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 79: 685-691
- Fitzpatrick RE, Goldman MP (1991) The depth of thermal necrosis using the CO2 Laser: A Comparison of the superpulsed mode and conventional mode. J Dermatol Surg Oncol 17: 340-344
- Guttenberg SA, Emery RW (2004) Laser physics and tissue interaction.Oral Maxillofac Surg Clin North Am. 16: 143-147
- Bartels KE, Bartels KE (2002) Lasers in veterinary medicine-where have we been and where are we going? Vet Clin Small Anim 32: 495-515
- Berger N, Eeg PH (2006) Veterinary Laser Surgery: A Practical Guide. Blackwell Publishing, Iowa USA.
- Holt TL, Mann FA (2002) Soft tissue application of lasers. Vet Clin North Am Small Anim Pract 32: 569-599
- Hernandez-Divers SJ (2008) Radiosurgery and laser in zoological practice: Separating fact from fiction. J Exot Pet Med 17: 165-174
- Ossoff RH (1989) Laser safety in otolaryngology-head and neck surgery: Anesthetic and educational considerations for laryngeal surgery. Laryngoscope 99: 1-26
- Lim RY, Kenney CL (1986) Precaution and safety in carbon dioxide laser surgery. Otolaryngol Head Neck Surg 95: 239-241
- Dailey SH, Kobler JB, Zeitels SM (2004) A laryngeal dissection station: Educational paradigms in phonosurgery. Laryngoscope 114: 878-882
- Stasche N, Quirrenbach T, Barmann M, Krebs M, Harrass M, et al. (2005) IMOLA-A new larynx model for surgical training. Education in transoral laser microsurgery of the upper airways. HNO 53: 874-875
- Safety of laser products-Part 14: A users guide (2004) British Standard.
- Brahmavar S, Hetzel F (2001) Medical Lasers: Quality control, safety standards and regulations. Joint Report. AAPM General Medical Physics Committee and American College of Medical Physics.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi