Research Article, J Otol Rhinol Vol: 8 Issue: 1
A Rare Impaction’s Site of a Common Ingested Foreign Body on Neck in an Adult
Zahra Al-Slail1, Rashed AlGhanim2, Jyan Bhati3 and Zeinab Al Qudehy4*
1ENT resident, Dammam Medical Complex, Eastern Province, Saudi Arabia
2ENT intern, Dammam Medical Complex, Eastern Province, Saudi Arabia
3ENT specialist, Dammam Medical Complex, Eastern Province, Saudi Arabia
4ENT consultant, Pediatric Otolaryngologist, Dammam Medical Complex, Eastern Province, Saudi Arabia
*Corresponding Author : Zeinab AlQudehy
ENT consultant, Pediatric Otolaryngologist, Dammam Medical Complex, Eastern Province, Saudi Arabia
Tel: 00966504804838
Fax: 00966138901950
E-mail: drzeinabent@gmail.com
Received: November 26, 2018 Accepted: December 25, 2018 Published: January 02, 2018
Citation: Al-Slail Z, AlGhanim R, Bhati J and Qudehy ZA (2019) A Rare Impaction’s Site of a Common Ingested Foreign Body on Neck in an Adult. J Otol Rhinol 8:1. doi: 10.4172/2324-8785.1000361
Abstract
Ingestion of sharp foreign body such as fish bone is not uncommon among all ages. Fortunately, complications due to foreign body ingestion are rare; however, if present, these can cause significant morbidity to the patient. It fairly known that the fish bone can migrate within the neck causing variable symptoms and signs in clinical presentation. Migration of a foreign body from the oropharynx to the submandibular gland is extremely rare, with only one case reported in English literatures. In this short communication we are reporting what we considered as second case of migrating fish bone in an adult. The foreign body was not seen in plain radiological study done initially. The patient presented a week later with swelling of left submandibular region. Computed tomography scan showed features of sialoadenitis with fish bone seen within the submandibular gland. Patient was treated conservatively with IV antibiotics, and was discharged with follow up but unfortunately he lost his follow up. We conclude from this case that careful assessment of symptomatic patient with sharp foreign body ingestion is crucial to avoid more serious complications.
Keywords: Fish bone; Foreign body ingestion; Throat pain; Acute submandibular siloadenitis
Introduction
Foreign body ingestion is a common complaint among adults in children, and frequently seen by practicing otolaryngologist. In adults, fish bones are the most commonly encountered accidently ingested foreign bodies [1]. Complications associated with foreign body ingestion are rare, and if present, it can cause significant morbidity, and even mortality in some cases [2,3]. Cervical abscess formation can occur if the foreign body was sharp and left un-noticed and un-treated, thus migrate through the neck, with incidence of less than 1% in reported literatures [3,4]. Sharp ingested foreign body can result in death which can reach as high as 32 % in case of esophageal perforation occurred [3]. With advanced in radiological and endoscopic techniques, management of foreign body have improved significantly, and impending complications have reduced over years. In the other hand, diagnosing cause of worsening clinical symptoms in patients with migrating sharp foreign, especially in the presence of negative endoscopy, is a challenging issue.
Esophageal perforation, vascular complications, recurrent cervical infection, cervical abscesses, and mediatinitits are some of the encountered retained and migrated ingested foreign body [1,3,5,6]. A carful history and examination of patient presented with sharp foreign body ingested is advisable to avoid impending complications.
In this article, we describe a rare case of retained migrating fish bone ingested causing acute submandibular siloadenitis and stayed within the submandibular gland.
Case Report
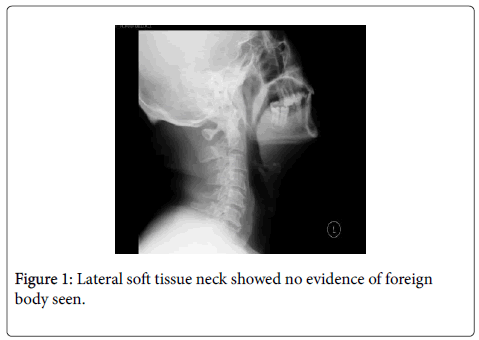
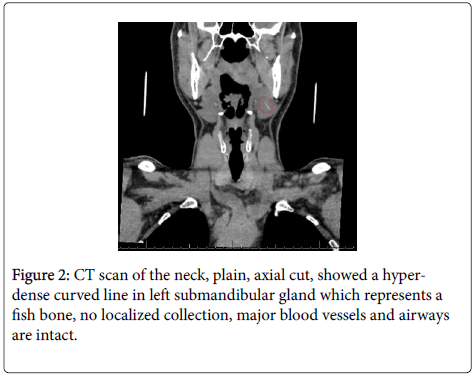
A 51year-old Egyptian male, medically free, presented to our emergency room complaining of one-week history of left throat pain after having a fish meal. Patient developed painful swelling in the left submandibular region. The pain was constant pricking sensation in nature and felt all over the left throat with no relation to food intake. Patient had no history of subjective fever, vomiting or diarrhea. Patient gave history of several emergency room visits where x-ray was done to him and was unremarkable (Figure 1), so he was discharged home on analgesic treatment. Patient continued to have the painful swelling for one week with no improvement, for which he re-visited our ER. On examination, patient was looking well, afebrile with stable vital signs. Local examination of the neck, confirmed by bimanual palpation, revealed left submandibular gland swelling measuring 2×3 cm, soft, mobile, tender, not fluctuation, with no sign of cellulitis and no obvious discharge from Wharton’s duct. Patient was admitted. A computerized tomography of neck with and with out contrast was done of the patient which show a hyper- dense curved line in left submandibular gland which represent a fish bone, no localized collection, major blood vessels and airways are intact (Figure 2). Patient was kept on Cefuroxime IV 1500 mg every eight hours for five days. During his hospital stay, he had significant improvement in the pain and in the swelling with the swelling almost disappeared at the end of the antibiotic course. Patient and due to especial work related issue, he was discharged home with instructions, that is to come to ER in case of any alarming symptoms show up such as; persistent fever, pain pricking sensation, or neck swelling. He was given close clinic follow up in one-week time with two weeks planned ultrasound neck appointment. In his first ENT clinic follow up, one-week after discharge from the hospital, he was free of symptoms, and tolerating normal diet well. Unfortunately, patient did show for his ultrasound appointment and was out of reach for almost one month [7].
Discussion
The most frequent ingested foreign bodies from otolaryngology prospective are chicken and fish bones. Beside the tonsils, the base of the tongue and the upper esophagus are the places where usually the impacted foreign bodies are found [7]. Migrating sharp ingested foreign bodies, more than others fish or chicken bones, and pins, can cause significant morbidity. It is possible that the sharp end of a foreign body causes mucosal injury on its way down, causing sudden pain and anxiety to the patient and presented to the otolaryngologist. Flexible endoscopic or rigid angled telescopic examination of the larynx performed in out patient department setting may failed to demonstrate the foreign body. Fortunately, many of these foreign bodies passed and the pain gradually subsided in one to two days. Presence of persistent pain, fever, respiratory problems, hemoptysis, or neck swelling should be taking seriously and warranty a second look endoscopic/ telescopic examination of the larynx.
Anticipating the diagnosis and role out foreign body ingestion complications can be challenging more in pediatric patients with inability to get an accurate history [5]. Several risk factors have been published, in literatures, as predictors for the occurrence of foreign body complications such as extreme of age, delayed presentation, presence of comorbidities, cricopharyngeal impaction, and negative radiological examination [8]. Therefore, absence of the ingested foreign body on initial examination can not rule out the possibility of foreign body to cause impending serious complication. Although the complications related to the migrated sharp foreign body can be immediate in form of upper respiratory airway abscesses [9], it’s migration through the pharyngeal wall can results in superficial cervical abscesses even few days to months later [7-12]. Fever, sore throat, odynophagia, and presence of neck swelling are the most common clinical presentation of neck infection following migrated ingested foreign body as seen in our patient. Several cases have reported in literatures with the migrated foreign body lodged in the lobe of the thyroid gland, burst through neck externally, pierced the internal jugular vein, presented as a mediastinal mass, pulmonary mass, cardiac tamponade, liver abscess, or even peritonitis [13-18]. Foreign body-associated sialoadenitis of submandibular gland is very rare within the literature [19]. Up to our knowledge, this is the only case presented with submandibular sialoadenitis resulted from ingested fish bone migrated from floor of the mouth and retained in the submandibular gland.
Upon encountering a case of persistent pain, fever, or suspecting complications in patients with history of foreign body ingestion, CT scan can be done. CT scan is highly accurate, with high positive value and can be used to confirm the presence of foreign body, identify its site and determine relationship of the foreign body in the neck, which is often missed by plain neck radiographs [20]. Although, CT scan is better than plain X-ray of the neck, a plain radiograph is the first line of investigation and positive findings will be the bases for patient further management.
Magnetic resonance imaging (MRI) has proven to be effective in diagnosing non-metallic migrated foreign bodies missed by a prior CT scan, but is contraindicated in suspected metallic foreign body ingestion. Some authors have suggested using ultrasound to identify the location of a migrated foreign body in the neck [1].
Management of patient with migrated ingested foreign body should be directed to the patient’s clinical presentation. Patient presented with cervical abscess due to a migrated foreign body can be managed by draining the abscess, retrieving the foreign body and administering intravenous antibiotics along with nasogastric feedings. In our case, the management was conservative with administration of intravenous antibiotics, and planning for retrieving the foreign body at later stage after reassessment of the foreign body location by ultrasound of the neck, but the patient unfortunately missed his appointment and did not show after.
Conclusion
Sharp foreign bodies ingestions, such as fish bones, are not uncommon. The sharp end of the ingested fish bone inflicts mucosal injury on its way down, causing pain and anxiety to the patient. Normal clinical examination and negative endoscopy does not role out the presence of foreign body. Many such foreign bodies pass without alarm. Persistence of symptoms, such as pain and sore throat, or sudden onset of ominous signs, such as hemoptysis, fever, or neck swelling, must direct the otolaryngologist to the possibility of a migrating foreign body. A high index of suspicion is needed to rule out retained, migrated foreign body related serious complications. A Neck CT scan plays a major role in locating the foreign body and identifying the presence of complication. Management is individualized and aimed to treat infection, and remove the foreign body. We report this case of a healthy patient presented with siloadenitis, which is an unusual presentation of common foreign body ingestion, i.e. fish bone. We valued here the importance of history taking and re-evaluation in case of persistence symptoms.
References
- Watanabe K, Amano M, Nakanome A, Saito D, Hashimoto S (2012) The prolonged presence of a fish bone in the neck. Tohoku J Exp Med 227: 49-52.
- Kerschner JE, Beste DJ, Conley SF, Kenna MA, Lee D (2001) Mediastinitis associated with foreign body erosion of the esophagus in children. Int J Pediatr Otorhinolaryngol 59: 89-97.
- Lam HC, Woo JK, van Hasselt CA (2003) Esophageal perforation and neck abscess from ingested foreign bodies: Treatment and outcomes. Ear Nose Throat J 82: 786-794.
- Nandi P, Ong GB (1978) Foreign body in the oesophagus: Review of 2394 cases. Br J Surg 65: 5-9.
- McLaughlin RT, Morris JD, Haight C (1968) The morbid nature of migrating foreign body in the esophagus. J Thorac Cardiovasc Surg 55: 188-192.
- Landis BM, Giger R (2006) An unusual foreign body migrating through time and tissues. Head Face Med 2: 30.
- Chee LW, Sethi DS (1999) Diagnostic and therapeutic approach to migrating foreign bodies. Ann Otol Rhinol Laryngol 108: 177-180
- Lai AT, Chow TL, Lee DT, Kwok SP (2003) Risk factors predicting the development of complications after foreign body ingestion. Br J Surg 90: 1531-1535.
- Nusbaum AO, Som PM, Rothschild MA, Shugar JM (1999) Recurrence of a deep neck infection: A clinical indication of an underlying congenital lesion. Arch Otolaryngol Head Neck Surg 125: 1379-1382
- Barzilai G, Braverman I, Karmeli R, Greenberg E (2001) How did it get there? A coiled metal foreign body in an unusual cervical position. Otolaryngol Head Neck Surg 124: 590-591.
- Gertner R, Bar'el E, Fradis M, Podoshin L (1991) Unusual complication of an ingested foreign body. J Laryngol Otol 105: 146-147.
- Kumar BN, Walsh RM, Courteney-Harris RG (1997) Laryngeal foreign body: an unusual complication of percutaneous tracheostomy. J Laryngol Otol 111: 652-653.
- Ohbuchi T, Tabata T, Nguyen KH, Ohkubo JI, Katoh A, et al. (2012) Thyroid gland cutaneous fistula secondary to a migratory fish bone: A case report. J Med Case Rep 6: 140.
- Joshi AA, Bradoo R (2003) A foreign body in the pharynx migrating through the internal jugular vein. Am J Otolaryngol 24: 89-91.
- Radford PJ, Wells FC (1988) Perforation of the oesophagus by a swallowed foreign body presenting as mediastinal and pulmonary mass. Thorax 43: 416-417.
- Sinha A, Shotton JC (1996) An unusual foreign body migrating from pharynx to mediastinum. J Laryngol Otol 110: 279-280.
- Sharland MG, McCaughan BC (1993) Perforation of the esophagus by a fish bone leading to cardiac tamponade. Ann Thorac Surg 56: 969-971.
- Stoica M, Sãftoiu A, Gheonea DI, Dumitrescu D, Surlin V (2007) Pyogenic liver abscess caused by accidental ingestion of a wooden toothpick: Role of preoperative imaging. J Gastrointestin Liver Dis 16: 221-222.
- Ozturk KI, Erdur O, Aksoy C (2016) Foreign body of submandibular gland. J Craniofac Surg 27: e600-e601
- Chung SM, Kim HS, Park EH (2008) Migrating pharyngeal foreign bodies: A series of four cases of saw-toothed fish bones. Eur Arch Otorhinolaryngol 265: 1125-1129.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi