Research Article, J Womens Health Issues Care Vol: 6 Issue: 2
Association of Lumbopelvic Pain with Pelvic Alignment and Gait Pattern during Pregnancy
Saori Morino1,2, Masaki Takahashi1, Ayumi Tanigawa1, Shu Nishiguchi3, Naoto Fukutani3, Daiki Adachi3, Yuto Tashiro3, Takayuki Hotta3, Daisuke Matsumoto4, Tomoki Aoyama3,*
1Department of System Design Engineering, Faculty of Science and Technology, Keio University, Kanagawa, Japan
2Japan Society for the Promotion of Science, Tokyo, Japan
3Department of Physical Therapy, Human Health Sciences, Graduate School of Medicine, Kyoto University, Kyoto, Japan
4Department of Physical Therapy, Faculty of Health Sciences, Kio University, Nara, Japan
*Corresponding Author : Tomoki Aoyama
Department of Human Health Sciences, Graduate School of Medicine, Kyoto University, 53 Kawahara-cho, Shogoin, Sakyo-ku, Kyoto 606-8507, Japan
Tel: +81 75 751 3935
Fax: +81 75 751 3909
E-mail: aoyama.tomoki.4e@kyoto-u.ac.jp
Received: February 16, 2017 Accepted: March 14, 2017 Published: March 20, 2017
Citation: Morino S, Takahashi M, Tanigawa A, Nishiguchi S, Fukutani N, et al. (2017) Association of Lumbopelvic Pain with Pelvic Alignment and Gait Pattern during Pregnancy. J Womens Health, Issues Care 6:2. doi: 10.4172/2325-9795.1000263
Abstract
Study background: Management of lumbopelvic pain (LPP) during pregnancy is important and the anatomical and movement aspects may be related to LPP. This study aimed to investigate the association of LPP with pelvic alignment and gait pattern during pregnancy.
Methods: Fifty-seven pregnant women were categorized into either the LPP or non-LPP (NLPP) group. Anterior pelvic tilt and bilateral difference in pelvic tilt as pelvic asymmetry were measured. An inertial measurement unit was attached at the participants’ L3 spinous process to measure 3-axes acceleration during gait. The degrees of movement symmetry, gait variability, and trunk movement were expressed as the autocorrelation peak (AC), coefficient of variance, and root mean square (RMS), respectively. An independent t-test was used to investigate differences in pelvic alignment and gait parameters between the groups. Multivariate stepwise logistic regression analysis was used to identify parameters that affected LPP. Additionally, multivariate linear regression analyses were performed to determine the parameters affected by LPP. Each significant parameter (from the previous analysis) was included as a dependent variable. Meanwhile, the presence or absence of LPP, BMI, and pregnancy months were included as explanatory variables.
Results: In the LPP group, pelvic asymmetry was significantly higher, and the AC and RMS were significantly lower than that in the NLPP group. In the multivariate analysis, pelvic asymmetry and AC significantly affected LPP, while LPP significantly affected pelvic asymmetry and RMS.
Conclusion: Pelvic asymmetry and movement asymmetry during gait affect LPP, while LPP affect pelvic asymmetry and trunk movement during gait. Therefore, evaluating both of the pelvic alignment and gait pattern especially focusing on asymmetry is important for management LPP during pregnancy.
Keywords: Asymmetry; Gait analysis; Lumbopelvic pain; Posture; Pregnancy
Introduction
Lumbopelvic pain (LPP) is common discomfort experienced by women during and after pregnancy with approximately 45% of pregnant women and 25% of postpartum women experience this pain [1]. Unfortunately, pregnancy-related LPP often adversely influences these women’s activities of daily living, such as cleaning, working outside the home, and even sleeping [1,2]. Thus, LPP is known to lower the quality of life for many women during and after pregnancy [3]. Therefore, the factors that are related to LPP during pregnancy should be identified and, if possible, addressed to allow for a more comfortable pregnancy.
The main factors that are related to LPP during pregnancy are thought to be increased joint laxity such as sacroiliac joint (due to pregnancy-related hormones) and pelvic anteversion (due to pregnancy-related abdominal swelling) [4,5]. Moreover, various other anatomical and physiological changes also occur in women’s bodies during pregnancy. For example, one previous study has reported a differing degree of pelvic anteversion in the right and left sides during pregnancy [6]. Therefore, the investigation of relationship between physiological aspects especially focusing on pelvic positioning and LPP during pregnancy is needed.
In addition to physiological and posture aspects, movement patterns during daily activity are typically thought to be strongly associated with low back pain [7]. On this point, changes in movement patterns during daily activities (such as gait pattern, step and stride length, stance phase, and joint motion during gait) have been observed as pregnancy progresses [8,9]. The changes in the gait pattern mechanics are characterized by changes in the woman’s physiological shape and dimensions, particularly in the trunk [10]. In addition, these movements are thought to be related to lower back pain, especially those that are accompanied by flexure and rotation of the trunk, such as sitting and active bending [11]. Similarly, pregnancy-related LPP often adversely influences the daily activities, such as carrying, sitting, and walking [12]. Furthermore, Wu et al. have indicated that gait speed was significantly reduced in post-partum women with pregnancy-related pelvic pain, compared to that in healthy women [13]. Therefore, changes in gait pattern during pregnancy may also be related to LPP during pregnancy.
Therefore, the static and dynamic aspects and LPP may be mutually related during pregnancy. However, the relationship between LPP and both of these static and dynamic aspects in the same subjects has not been established for pregnant women. Therefore, this study aimed to investigate the association of LPP with static pelvic alignment and gait pattern during pregnancy.
Materials and Methods
Participants
Pregnant women were recruited at an event that was held for pregnant women and mothers in Aichi Prefecture, Japan, during March 2013. Among the attendees, 57 women who were between the third and tenth month of pregnancy, and who had no history of lower back, foot, ankle, knee, musculoskeletal, and neuromuscular trauma or disease, were included in this study. The inclusion criterion was a pregnancy without serious orthopedic disorders or neurological diseases, and participants with external injuries that affect the gait analysis were excluded for recruitment. The women who met the inclusion criterion in the attendees of the event were investigated and there was no one excluded after the recruitment of this study.
Questionnaire
Personal characteristics (age, height, and mass), month of pregnancy, and the presence or absence of LPP were determined using a questionnaire.
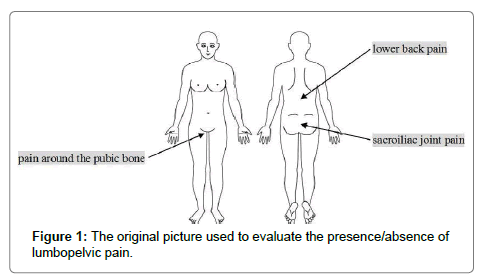
The presence or absence of LPP was evaluated using a picture of the human body (Figure 1) and the question “Do you currently have any pain in your lower back, sacroiliac joint, or around your pubic bone or have you had any pain there during your pregnancy? Please refer to the picture for these pain locations.” If there was anything participants can’t understand about the question, the researcher of this study (midwife or physical therapist) answered. Based on the answers of participants, they were categorized into LPP and non-LPP (NLPP) groups according to the presence or absence of LPP.
Pelvic alignment
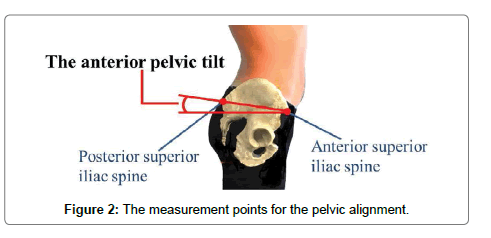
Pelvic alignment was measured using a palpation meter (Performance Attainment Associates, St. Paul, MN, USA). The anterior pelvic tilt was measured bilaterally by placing the caliper tips of the palpation meter in contact with the ipsilateral anterior and posterior superior iliac spines (Figure 2). This method is valid, reliable, and cost-effective for calculating any discrepancy between the patient’s landmarks [14]. Before the measurement, the researchers (two physical therapists) learned use method of the palpation meter and practiced repeatedly. In order to verify accuracy, the measurers measured pelvic alignment of a woman separately by the above method. The verification procedure was repeated twice, two weeks apart. As the result, the measurement procedure showed acceptable intra and inter-rater reliability with Intraclass Correlation Coefficients (ICC 1.1) of 0.998 (95% CI 0.995â€ÂÂ0.999) and 0.998 (95%CI 0.992â€ÂÂ1.000) for the anterior pelvic tilt in this study. During the pelvic alignment measurements, the participants took off their shoes and stood with hands crossed in front of their chest. Left and right anterior pelvic sagittal tiltings were measured in degrees. The mean left and right pelvic tilt degrees, and the bilateral difference in pelvic tilt were defined as anterior pelvic tilt and pelvic asymmetry, respectively.
Gait procedure and apparatus
All participants were evaluated using a smooth, horizontal, 14-m walkway. Gait was measured in a 10-m long middle section of the walkway, which was created by applying 2 lines (2 m from each end of the walkway) to allow for acceleration and deceleration. Participants performed the tests at their preferred speeds and while wearing shoes that did not mostly influence their gait.
The acceleration and angular velocity of the participant’s trunk were measured during the gait testing using a triaxial accelerometer (MVP-RF-8, MicroStone Co., Nagano, Japan). The sensor unit contained a tri-axial angular rate gyroscope and a linear accelerometer. Based on the method used by Moe-Nilssen and Helbostad [15], the sensor units were attached to a fixed belt at the level of the L3 spinous process, which is used to assess motion of the trunk during gait. However, we also considered it likely that the accelerometers attached to the body might experience various inclination states, due to the body’s curvature. To correct for any potential effects of these inclinations, we calibrated the accelerometer before each gait trial to take into account the static gravity component. The signals were sampled at a frequency of 200/s and were wirelessly transferred to a personal computer via a Bluetooth. To identify the walk cycle, a pressure sensor (FlexiForce, Nitta Co., Osaka, Japan) was attached to the participant’s heel, and this sensor was synchronized with the accelerometer. The heel contact event was defined as the time when the sensor’s voltage increased. The participants were timed as they walked over the 10-m portion of the walkway, and their gait speed was expressed in meters per second.
Data analysis
Signal processing was performed using MATLAB (The MathWorks Co., Release 2013b, Tokyo, Japan). Based on the method used by Nishiguchi, et al. [16], the autocorrelation peak (AC), coefficient of variance (CV), and root mean square (RMS) of the acceleration peak intervals were calculated using trunk acceleration data from 10 strides that were performed while walking in a steady state. Autocorrelation is useful for finding repeating patterns in a signal, and symmetry is a fundamental property of autocorrelation, therefore a higher AC value indicates a greater degree of symmetry during movement. The CV indicates the degree of gait variability, which was defined as the variability in the time that elapsed between the heel contacts for two consecutive footfalls. A higher RMS value indicated greater movement of the trunk. RMS is affected by gait speed (it is proportional to the square of gait speed), therefore we adjusted the RMS by dividing it by the square of the gait speed [17].
Ethical considerations
Written informed consent was obtained from each participant, in accordance with the guidelines approved by the Research Ethics Committee and the Declaration of Human Rights, Helsinki, 1975. The study’s protocol was approved by the Research Ethics Committee of Kio University (Approval No. H25-47).
Statistical analysis
Differences in age, mass, height, and month of pregnancy between the LPP and NLPP groups were evaluated using the independent t-test. We also initially used an independent t-test to evaluate the differences in the pelvic tilt, pelvic asymmetry, and each gait parameter between the LPP and NLPP groups. After this initial analysis, a multivariate step-wise logistic regression analysis was used to identify which parameters affected LPP, from among the factors that were statistically different when the two groups were compared. Finally, we performed multivariate linear regression analyses to determine which parameter was affected by LPP; each of these parameters was included as a dependent variable, and the presence or absence of LPP, body mass index, and month of pregnancy were used as explanatory variables. Statistical analyses were performed using SPSS version 20.0 (SPSS, Chicago, IL, USA), with a significance threshold set at 0.05.
Results
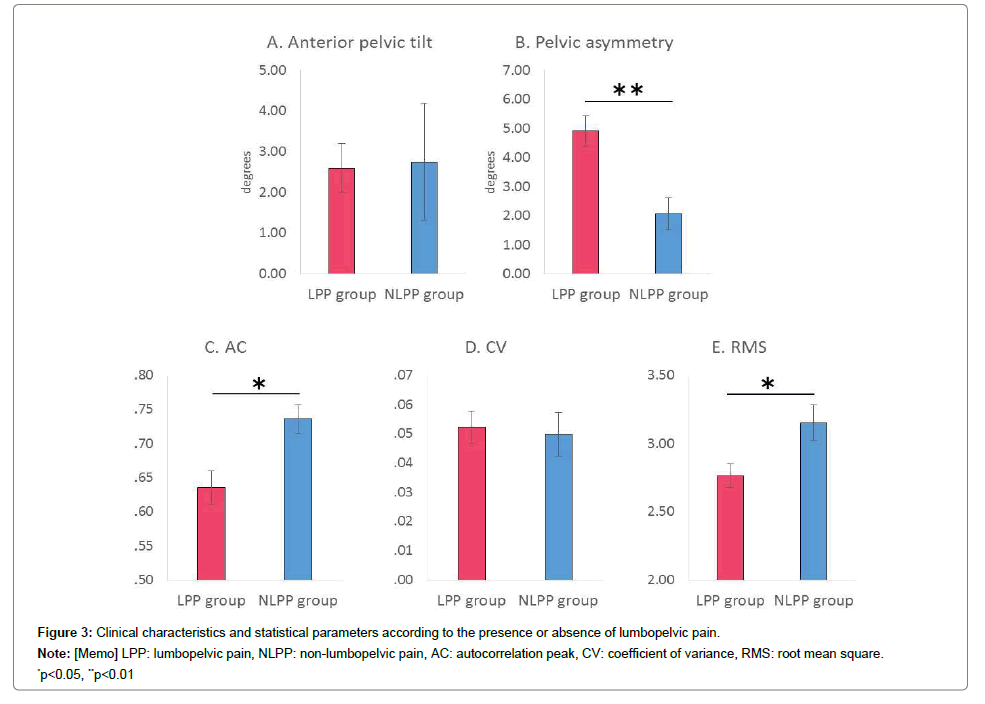
The demographic data of the LPP and NLPP groups are shown in Table 1. The prevalence of LPP was 75.4% (LPP group; n=43, NLPP group; n=14), although no significant differences were observed between the groups regarding age, height, mass, and month of pregnancy (Table 1). The pelvic asymmetry of the LPP group was significantly greater than that in the NLPP group (4.91 [SD 3.41]° vs. 2.07 [SD 2.06]°, respectively; p=0.001), although no significant differences were observed in the anterior pelvic tilt (2.59 [SD 3.94]° vs. 2.75[SD 5.40]°, respectively; p ï¼Ã‚Â0.907) (Figure 3). Among the gait parameters, the AC and RMS of the LPP group were significantly lower than those in the NLPP group (AC: 0.64 [SD 0.16] vs. 0.74 [SD 0.08], respectively; p ï¼Ã‚ 0.004, RMS: 2.77 [SD 0.57] vs. 3.15 [SD 0.49]; p ï¼Ã‚Â0.027), although no significant difference was observed in the CV (0.052 [SD 0.036] vs. 0.050 [SD 0.028]; p ï¼Ã‚Â0.827) (Figure 3). In the multivariate step-wise logistic regression analysis, pelvic asymmetry (odds ratio and 95% confidence interval: 1.499 [1.069– 2.101]) and AC (0.001 [0.000–0.911]) significantly affected LPP (Table 2). In contrast, in the multivariate linear regression analysis, LPP significantly affected pelvic asymmetry (β / p-value: 3.014/0.004) and RMS (–0.382/0.037) (Table 3).
| Presence of LPP† | ||||
|---|---|---|---|---|
| Total (n = 57) |
LPP† group (n = 43) |
NLPP‡group (n = 14) |
p-value | |
| Age (years) | 29.9 [SD 3.7] | 29.8 [SD 3.8] | 30.2 [SD 3.7] | 0.733 |
| Height (cm) | 158.4 [SD 5.5] | 158.2 [SD 5.6] | 158.9 [SD 5.3] | 0.687 |
| Mass (kg) | 57.1 [SD 7.9] | 57.9 [SD 8.5] | 54.7 [SD 4.9] | 0.189 |
| Month of pregnancy (month) | 6.7 [SD 1.8] | 6.7 [SD 1.5] | 6.8 [SD 2.3] | 0.837 |
† LPP: lumbopelvic pain, ‡ NLPP: non-lumbopelvic pain.
Table 1: Demographic differences according to the presence of lumbopelvic pain.
| Parameter | Odds ratio | 95% CI † | p-value |
|---|---|---|---|
| Pelvic asymmetry | 1.499 | 1.069–2.101 | 0.019* |
| AC ‡ | 0.001 | 0.000–0.911 | 0.047* |
| RMS § | 0.286 | 0.074–1.095 | 0.068 |
Table 2: Parameters associated with lumbopelvic pain in a multiple stepwise regression analysis.
| Independent variable | Regression coeeficient | Standard regression coefficient | p-value | R2 value | |
|---|---|---|---|---|---|
| Pelvic asymmetry | 0.173 | ||||
| LPP † | 3.014 | 0.997 | 0.004* | ||
| BMI ‡ | –0.092 | 0.166 | 0.582 | ||
| Month of pregnancy | 0.399 | 0.257 | 0.126 | ||
| AC § | 0.109 | ||||
| LPP † | –0.093 | 0.047 | 0.052 | ||
| BMI ‡ | –0.004 | 0.008 | 0.609 | ||
| Month of pregnancy | 0.015 | 0.012 | 0.213 | ||
| RMS || | 0.089 | ||||
| LPP † | –0.382 | 0.179 | 0.037* | ||
| BMI ‡ | –0.002 | 0.030 | 0.953 | ||
| Month of pregnancy | 0.019 | 0.046 | 0.682 |
*p<0.05
Table 3: Parameters associated with pelvic asymmetry, the autocorrelation peak, and root mean square in a multiple linear regression analysis.
Discussion
The current study investigated the association of LPP with both of static and dynamic aspects during pregnancy. Based on the results, higher pelvic asymmetry and lower AC had affected LPP during pregnancy. A previous study among adults has reported that static pelvic asymmetry is associated with lower back pain [18]. Besides, in the study of pregnant women, Damen et al. reported that pelvic pain is associated with asymmetric laxity of the sacroiliac joints [19], and Sipko, et al. observed asymmetric of pelvis alignment and irritation of pelvic and lumbar ligaments [20]. These results suggest that changes in pelvic alignment can easily occur during pregnancy and the resulting pelvic malalignment is related to LPP. We observed a similar result among pregnant women in this study. In addition, the lower AC of the LPP group indicated that pregnant women with LPP exhibited greater asymmetry during their gait. These results were similar to Selles, et al. who observed greater asymmetry among patients with lower back pain (compared to a control group) when they examined the phase-relations of the body’s left and right sides during gait [21]. It is possible that the asymmetry change in the static aspect occurs easily during pregnancy, due to the loosening action of pregnancy-related hormone on the body joints. Moreover, we observed motion asymmetry during gait in the participants of this study, as well as static pelvic asymmetry in pregnant women with LPP. Therefore, the static pelvic asymmetry might be related to asymmetry of the dynamic gait pattern. For example, it has been proposed that pelvic asymmetry alters the body mechanics, placing strain on various body segments, which subsequently contributes to musculoskeletal pain [22]. Therefore, our results indicate that both the static and dynamic aspects asymmetry might affect LPP during pregnancy.
In addition, our results indicate that LPP had an effect on lower RMS and higher pelvic asymmetry during pregnancy. The lower RMS indicated that the pregnant women with LPP moved their trunk less during gait, compared to the women in the NLPP group. Similarly, Al-Eisa, et al. have observed that pain-free people exhibit a broader range of movement in the lower thoracic region, compared to people with lower back pain [11]. Wu, et al. have also reported that pregnancy-related pelvic girdle pain decreased the rotation between the pelvis and lumbar segment, the lumbar segment and the thorax, and the pelvis and the thorax, especially at higher velocities [23]. Similarly, we observed that pregnant women with LPP tended to avoid excessive movement of the trunk during gait to reduce the pain they experienced. Furthermore, several study have demonstrated that the maximum gait speed is lower for people with pelvic girdle or lower back pain, compared to that for healthy people [13,24]. Therefore, pregnant women are compelled to control their trunk movement during gait (due to pain), which deteriorates their gait function. Moreover, we observed that LPP resulted in greater static pelvic alignment asymmetry among pregnant women. Thus, pelvic asymmetry appears to cause LPP, and untreated LPP can result in exacerbated chronic asymmetry.
Our results indicate that both the static and dynamic aspects mutually related to LPP during pregnancy. Thus, it is possible that these associations might create a vicious cycle, and treatment or prevention of LPP during pregnancy is needed to break this cycle. However, treatment via medication or surgery should be avoided during pregnancy, given the potential adverse effects on the mother and fetus [25]. Therefore, the factors that contribute to LPP must be identified, as these might be safe to treat. Our results indicate that greater pelvic and gait pattern asymmetry might affect LPP during pregnancy. Therefore, it is important to evaluate both the static and dynamic aspects of the pelvic region to prevent or treat LPP during pregnancy. Furthermore, treatment strategies that focus on the asymmetry of these aspects might be effective in resolving the LPP during pregnancy.
There were several limitations in the current study. First, this study used a cross-sectional design, rather than a longitudinal observational design. Therefore, further research is needed to investigate the causality of the relationships that we observed. Second, we investigated the presence of LPP using a self-reported questionnaire, rather than via an orthopedic diagnosis, and we classified the participants according to the presence of pain, rather than the extent of the pain. Thus, detailed pain data were not available, and the prevalence of LPP in this study was higher than that reported in a previous study [3]. However, we captured the features of static and dynamic aliment that were related to LPP via the self-assessed pain data. Third, we did not evaluate other factors that may affect pelvic asymmetry and gait strategy, such as the level of pregnancy-related hormones, muscular strength, or physical flexibility. Therefore, this is a pilot study suggesting association of LPP with static pelvic alignment and dynamic gait pattern during pregnancy that warrants further more detailed investigations. However, despite these limitations, the findings of the present study may encourage measurement of static and dynamic pelvic alignment, which may help to cure LPP.
In the current study, the association of LPP with static and dynamic aspects of pregnancy was investigated and it was revealed that pelvic asymmetry and lower back movement during gait were related to LPP during pregnancy. The results indicate that greater pelvic and lower back movement asymmetry might affect LPP during pregnancy. Meanwhile, LPP might affect movement of the trunk during gait and pelvic asymmetry.
Acknowledgements
This work was supported by JSPS KAKENHI Grant Number 15J07748. We are especially grateful to all of the participants for their willingness to participate. We are also grateful to the members of Humanalysis Square, Kyoto University, the members of Takahashi Laboratory, Keio University, and the members of Kio University for their helpful advice and auxiliary measurement.
References
- Wu WH, Meijer OG, Uegaki K, Mens JM, van Dieen JH, et al. (2004) Pregnancy-related pelvic girdle pain (PPP), I: Terminology, clinical presentation, and prevalence. Eur Spine J 13: 575-589.
- Liddle SD, Pennick V (2015) Interventions for preventing and treating low-back and pelvic pain during pregnancy. Cochrane Database Syst Rev 9: Cd001139.
- Katonis P, Kampouroglou A, Aggelopoulos A, Kakavelakis K, Lykoudis S, et al. (2011) Pregnancy-related low back pain. Hippokratia 15: 205-210.
- Kristiansson P, Svardsudd K, von Schoultz B (1996) Serum relaxin, symphyseal pain, and back pain during pregnancy. Am J Obstet Gynecol 1342-1347.
- Borg-Stein J, Dugan SA (2007) Musculoskeletal disorders of pregnancy, delivery and postpartum. Phys Med Rehabil Clin N Am 18: 459-476.
- Franklin ME, Conner-Kerr T (1998) An analysis of posture and back pain in the first and third trimesters of pregnancy. J Orthop Sports Phys Ther 28: 133-138.
- Schaller A, Froboese I (2004) Movement coaching: study protocol of a randomized controlled trial evaluating effects on physical activity and participation in low back pain patients. BMC Musculoskelet Disord 391.
- Branco MA, Santos-Rocha R, Vieira F, Aguiar L, Veloso AP (2016) Three-dimensional kinematic adaptations of gait throughout pregnancy and post-partum. Acta Bioeng Biomech 18: 153-162.
- Bertuit J, Feipel V, Rooze M (2015) Temporal and spatial parameters of gait during pregnancy. Acta Bioeng Biomech 17: 93-101.
- Gilleard WL (2013) Trunk motion and gait characteristics of pregnant women when walking: report of a longitudinal study with a control group. BMC Pregnancy Childbirth 13: 71.
- Al-Eisa E, Egan D, Deluzio K, Wassersug R (2006) Effects of pelvic asymmetry and low back pain on trunk kinematics during sitting: a comparison with standing. Spine (Phila Pa 1976) E135-E143.
- Sydsjo A, Sydsjo G, Wijma B (1998) Increase in sick leave rates caused by back pain among pregnant Swedish women after amelioration of social benefits. A paradox. Spine (Phila Pa 1976) 23: 1986-1990.
- Wu W, Meijer OG, Jutte PC, Uegaki K, Lamoth CJ, et al. (2002) Gait in patients with pregnancy-related pain in the pelvis: an emphasis on the coordination of transverse pelvic and thoracic rotations. Clin Biomech (Bristol, Avon) 678-686.
- Herrington L (2011) Assessment of the degree of pelvic tilt within a normal asymptomatic population. Man Ther 16: 646-648.
- Moe-Nilssen R, Helbostad JL (2002) Trunk accelerometry as a measure of balance control during quiet standing. Gait Posture 60-68.
- Nishiguchi S, Yamada M, Nagai K, Mori S, Kajiwara Y, et al. (2012) Reliability and validity of gait analysis by android-based smartphone. Telemed J E Health 18: 292-296.
- Menz HB, Lord SR, Fitzpatrick RC (2003) Acceleration patterns of the head and pelvis when walking on level and irregular surfaces. Gait Posture 35-46.
- Al-Eisa E, Egan D, Wassersug R (2004) Fluctuating asymmetry and low back pain. Evolution and Human Behavior 25: 31-37.
- Damen L, Buyruk HM, Guler-Uysal F, Lotgering FK, Snijders CJ, et al. (2001) Pelvic pain during pregnancy is associated with asymmetric laxity of the sacroiliac joints. Acta Obstet Gynecol Scand 1019-1024.
- Sipko T, Grygier D, Barczyk K, Eliasz G (2010) The occurrence of strain symptoms in the lumbosacral region and pelvis during pregnancy and after childbirth. J Manipulative Physiol Ther 33: 370-377.
- Selles RW, Wagenaar RC, Smit TH, Wuisman PI (2001) Disorders in trunk rotation during walking in patients with low back pain: a dynamical systems approach. Clin Biomech 175-181.
- Egan D, Al-Eisa E (1999) Pelvic skeletal asymmetry, postural control, and the association with low back pain: a review of the evidence. Critical Reviews in Physical and Rehabilitation Medicine 11: 299-338.
- Wu WH, Meijer OG, Bruijn SM, Hu H, van Dieen JH, et al. (2008) Gait in Pregnancy-related Pelvic girdle Pain: amplitudes, timing, and coordination of horizontal trunk rotations. Eur Spine J 17: 1160-1169.
- van den Hoorn W, Bruijn SM, Meijer OG, Hodges PW, van Dieen JH (2012) Mechanical coupling between transverse plane pelvis and thorax rotations during gait is higher in people with low back pain. J Biomech 342-347.
- Costantine MM (2014) Physiologic and pharmacokinetic changes in pregnancy. Front Pharmacol 5: 65.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi