Research Article, Int J Ophthalmic Pathol Vol: 0 Issue: 0
Clinical Outcome of Reconstruction of Lacrimal Canalicular Laceration with Monocanalicular Intubation System
Triptesh Raj Pandey*, Ben Limbu, Purnima Rajkarnikar Sthapit, Hom Bahadur Gurung, Rohit Saiju
Department of Ophthalmology, Tilganga Institute of Ophthalmology, Nepal
*Corresponding Author: Triptesh Raj Pandey
Department of Ophthalmology, Tilganga Institute of Ophthalmology, Nepal
E-mail: triptesh@gmail.com
Received: July 26, 2021 Accepted: August 20, 2021 Published: August 27, 2021
Citation: Pandey TR, Limbu B, Sthapit PR, Gurung HB, Saiju R, et al. (2021) Clinical Outcome of Reconstruction of Lacrimal Canalicular Laceration with Monocanalicular Intubation System. Int J Ophthalmic Pathol 10:7.
Abstract
Aim: To evaluate the clinical outcome of lacrimal canalicular laceration repair with self-retaining monocanalicular intubation system.
Materials and methods: All patients who underwent canalicular laceration repair with monocanalicular intubation system from 1st January 2016 to 31st December 2017 at a tertiary eye care center were retrospectively analyzed. Demographics, operative details and clinical outcomes were noted. Anatomical and functional successes were defined by a patent nasolacrimal duct on lacrimal sac syringing and absence of epiphora respectively.
Results: Out of 26 patients, 20 (76.92%) were males. The mean age at presentation was 27.15 years (range, 1 to 60 years). Lower canalicular injuries occurred in 19 cases (73.06%) and upper canalicular injuries occurred in 5 cases (19.23%), 2 cases involved both upper and lower canaliculi. Fall injuries and the hook-like objects comprised the major etiologies for the canalicular lacerations (14/26 cases, 53.84%). The mean duration of injury to repair was 49.58 ± 93.61 hours (range, 4 hours to 20 days) and mean duration for stent removal after surgery was 4.69 months (range, 2 months to 6 months). Three cases (11.53%) had stent migration. Punctual slit and wound gaping occurred in 1 case each. Anatomical success was achieved in 18 (85.71%) and functional success was achieved in 22 cases (84.61%).
Conclusion: Canalicular injuries are more common in young male patients, mostly secondary to fall injuries and hook-like objects. Clinical outcomes of monocanalicular intubation in canalicular lacerations are excellent irrespective of the delay in presentation without significant complications.
Keywords: Canalicular laceration, Epiphora, Monocanalicular intubation, Stent migration
Introduction
Eyelid injuries commonly occur as a result of blunt or sharp periocular injuries and may involve canalicular system in up to 16% of eyelid lacerations [1]. All age groups of patients may be affected; especially children and teenagers are at high risk [1-3]. If the canalicular system is not repaired initially, patients may have symptoms of tear overflow due to the disruption of the lacrimal canaculi anatomy. The principles of repairing a canalicular injury involve identification of the torn ends of the canaliculus, suturing of the cut ends under high magnification and intubating the canaliculus to prevent fibrosis and subsequent stenosis and thereby maintaining its patency [4,5]. If surgical repair of the lacerated canaliculus is not appropriate, the patient may develop symptomatic Epiphora [6]. Numerous surgical techniques have been described for the repair of canalicular lacerations; these can be divided into monocanalicular intubation and bicanalicular intubation techniques. A variety of materials have been used to stent the torn canaliculus in the past. Medical grade Silicone, because of its inert nature, flexibility, and easy availability, has emerged as the material of choice for lacrimal stenting [7,8].
In this study, we describe the epidemiological and clinical characteristics of patients with canalicular lacerations and evaluate the surgical outcomes of reconstruction of lacrimal canalicular laceration with self-retaining monocanalicular intubation system.
Methods
In this study, a retrospective analysis of all the patients who underwent canalicular laceration repair with monocanalicular intubation system, over a period of 2 years (1st January 2016- 31st December 2017) was done. The data collected for the study included each patient’s demographic information, history and mode of injuries, time interval between injury and presentation, associated other ophthalmic injuries, time interval between injury and surgical intervention, intra-operative findings, postoperative findings and complications, stent related complications, time of stent removal, anatomical and functional success following stent removal. Anatomical success was defined as patent nasolacrimal drainage system on lacrimal sac irrigation, and functional success was defined as the absence of epiphora after removal of the stent. Clinical success was defined as the presence of anatomical and/or functional success. Monocanalicular intubation stent used in this study is a medical grade silicone implant of length 40 mm and diameter 0.64 mm for reconstructing traumatic canalicular lacerations.
Surgical management consisted of identifying the cut ends of the canaliculus under an operating microscope. The mono-canalicular stent was then placed within the lacerated canaliculus through punctum, and repair of the eyelid laceration was performed using standard surgical techniques. Pericanalicular repair was done with 8-0 polyglactin suture and skin and muscle repair was done with 6-0 polyglactin suture under local anesthesia in adults and general anesthesia in children. Post-operatively the patients were advised topical antibiotic ointment and drops for four weeks and topical lubricants till the stent was removed.
The patients were reviewed on day 1 after surgery, at one month, at three months and at six months. The stent removal was done at 3 months at the earliest unless there were any stent related complications. In all patients, stent was removed under topical anesthesia in the office settings. Lacrimal sac syringing was done after stent removal and on subsequent visits in all adult patients and children who were co- operative. Patients with incomplete data and who had follow-up of less than three months were excluded from further analysis.
Results
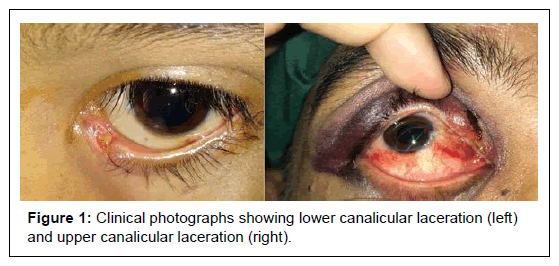
The total 26 out of 29 patients who underwent canalicular laceration repair with monocanalicular intubation system were included in the study; 3 were excluded due to lack complete medical data and/or lack of follow up. The mean age at presentation was 27.15 years (Range: 1-60 years). Majority of the patients were children (below 16 years, 9 out of total 26 cases, 34.6%) and males (Male: Female – 3.3 :1). Lower canalicular injuries occurred in 19 cases (73.06%) and upper canalicular injuries occurred in 5 cases (19.23%), 2 cases involved both upper and lower canaliculi (Table 1 and Figure 1). Fall injuries and the hook-like objects comprised the major etiologies for the canalicular lacerations (14/26 cases, 53.84%) (Table 2).
| Total patients | 26 |
|---|---|
| Male | 20 (76.92%) |
| Female | 6 (23.07%) |
| Eye involved | |
| Right | 18 (26.23) |
| Left | 8 (30.76%) |
| Canaliculus involved | |
| Upper | 5 (19.23%) |
| Lower | 19 (73.07%) |
| Both | 2 (7.69.%) |
Table 1: Demographic profile of patients undergoing canalicular laceration repair.
| Mode of injury | Number | Percent |
|---|---|---|
| Fall injuries | 8 | 30.8 |
| Hook-like objects | 6 | 23.1 |
| Sharp objects | 6 | 23.1 |
| Blunt objects | 2 | 7.7 |
| Road traffic accidents | 2 | 7.7 |
| Physical assaults | 2 | 7.7 |
| Total | 26 | 100 |
Table 2: Etiology of lacrimal canalicular lacerations.
Simultaneous globe injuries occurred among 12 cases with isolated lid injuries with canalicular lacerations occurred in 16 cases, 4 cases had other facial injuries. Periorbital injuries with ecchymosis and subconjunctival hemorrhage were the other commonly associated ophthalmic injuries among the cases (Table 3). All the cases with upper canalicular laceration (7 cases; 5 upper canaliculi, 2 bincanalicular) were associated with simultaneous globe injuries.
| Associated ophthalmic injuries | Number |
|---|---|
| Periorbital ecchymosis, subconjunctival hemorrhage | 5 |
| Full thickness lid laceration | 1 |
| Conjunctival laceration | 1 |
| Corneal epithelial defect | 2 |
| Traumatic iritis | 1 |
| Hyphema | 1 |
| Subluxated lens, vitreous hemorrhage | 1 |
| Retinal hemorrhage, commotio retinae | 3 |
| Total | 15 |
Table 3: Other associated ophthalmic injuries.
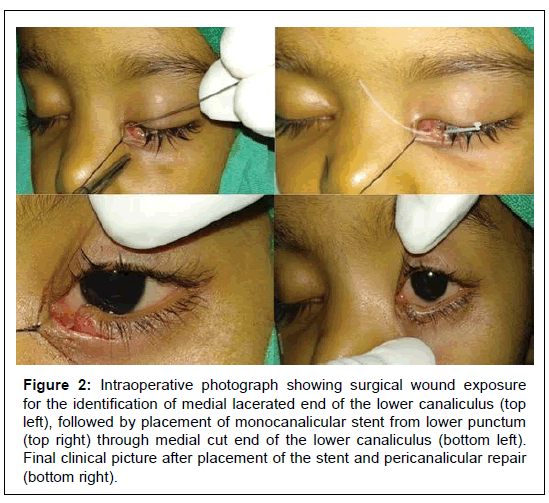
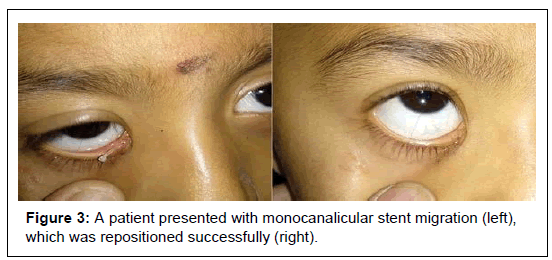
The mean duration of injury to repair was 49.58 ± 93.61 hours (Range: 4 hours to 20 days) (Figure 2) and mean duration for stent removal after surgery was 4.69 months (Range: 2 months to 6 months) (Table 4). Three cases (11.53%) had stent migration, which were successfully repositioned under topical anesthesia (Figure 3). Punctal slit occurred in 1 case (3.84%) and 1 case (3.84%) had wound gaping after 2 weeks (Table 5). Anatomoical success was achieved in 18 (85.71%) out of 21 cases who underwent syringing. Syringing could not be done in 5 pediatric cases. Similarly, functional success was achieved in 22 cases (84.61%) out of total 26.
| Mean duration from injury to repair | 49.58 ± 93.61 hours |
|---|---|
| (Range: 4 hours to 20 days) | |
| Mean duration for stent removal | 4.69 months |
| (Range: 2 months to 6 months) | |
| Anatomical success | 18/21 (85.71%) |
| Functional success | 22/26 (84.61%) |
Table 4: Surgical outcome following canalicular laceration repair.
| Complication | Number | Percent |
|---|---|---|
| Stent migration | 3 | 11.53% |
| Punctal slit | 1 | 3.84% |
| Wound gaping | 1 | 3.84% |
Table 5: Monocanalicular stent and wound related complications.
Figure 2: Intraoperative photograph showing surgical wound exposure for the identification of medial lacerated end of the lower canaliculus (top left), followed by placement of monocanalicular stent from lower punctum (top right) through medial cut end of the lower canaliculus (bottom left). Final clinical picture after placement of the stent and pericanalicular repair (bottom right).
Discussion
Canalicular lacerations are commonly associated with eyelid injuries and can lead to epiphora if not managed properly. Majority of the patients with canalicular lacerations in our study were aged less than 16 years (34.6%) and were males (76.92%). Similar findings were described in other studies, highlighting the predominance of canalicular injuries among children and young male adults [2,9-11]. In this study the most common causes of canalicular injuries were fall injuries, injuries with hook-like objects and sharp objects. Two cases occurred due to blouse-hook injuries (2 out of 6, 33.3%) while breast feeding and were peculiar to the south Asian subcontinent region, also described by Naik [2]. Dog bites are frequently described as common cause for canalicular lacerations among children, but were not involved in our study [2,12,13]. However, the etiologies for the canalicular lacerations can differ depending upon the socio-cultural variations and geographical regions.
In our study, lower canalicular injuries (73.07%) were more frequent than upper (19.23%), with 2 cases of bicanalicular injuries (7.69%). These findings were similar to the previous studies [2,3,11,14,15]. Previous studies have reported 20% to 44% of incidence of simultaneous globe injuries associated with eyelid injuries [16,17]. In our study, 12 cases (46.15%) had simultaneous globe injuries and most of them were associated with upper canaliculi injuries (7 cases, 58.33%); this finding corroborates with previous study showing that upper canaliculi injuries are frequently associated with simultaneous globe injuries [2].
The main aim of the canalicular laceration repair is to retain the anatomical anastomosis with canalicular stent followed by the reapproximation of the overlying pericanalicular tissues with suture (Figure 2). The stent is left in situ until the re-epithelisation of the canaliculus occurs. Different surgical techniques have been described for repairing canalicular injuries using both monocanalicular and bicanalicular stent. We avoided the use of bicanalicular stent because of the potential risk of iatrogenic damage to the uninvolved canaliculus and nasolacrimal lumen, and the technical difficulty of placing the stents [17]. In our study, there were 2 cases (7.69%) with bicanalicular injuries. For those bicanalicular lacerations, two separate monocanalicular stents were used, one in each canaliculus as described in literature [2,9].
If the canalicular system is not repaired initially, patients may have symptoms of tear overflow due to the disruption of the lacrimal canaculi anatomy. Thus, the early surgical intervention is of paramount importance to maintain the anatomical as well as functional patency of the repaired canaliculus. In our study, the mean duration of injury to repair was 49.58 ± 93.61 hours (Range: 4 hours to 20 days), similar to the literature [2]. It is worthwhile to try and repair the canalicular injuries with intubation at any time after the canaliclular injuries, even after weeks following the canalicular injuries [9]. Likewise, we could successfully intubate the canaliculus with the monocanalicular stent in one case even after 20 days following the canalicular injury, thus highlighting the importance meticulous surgical exploration and approach.
Punctal and canalicular slitting, stent extrusion, granuloma formation, pericanalicular infection, etc. have been reported as the complications following canalicular repair with the stent [7,9,18,19]. In our study, three cases (11.53%) had stent migration which were successfully repositioned under topical anesthesia. Premature stent loss is a major disadvantage associated with monocanalicular stent technique that can result in poor surgical outcome [1,18,20]. However, there was no case of complete extrusion of the stent in our study. Punctal slit occurred in 1 case (3.84%) for which stent removal was done 2 month and 1 case (3.84%) had wound gaping after 2 weeks which required resuturing of the wound.
The role of the stent is to aid in the healing process and epithelialization of the injured lacrimal canalicular lumen. However, there is no general consensus for the optimal duration for lacrimal canalicular stenting. Several studies have recommended the duration ranging from 3 to 12 months for canalicular stenting [20-22]. In our study, stents were targeted to be kept in situ for at least 3 month, (Range: 2 - 6 months); early stent removal was considered in 1 case (2 month) due punctal slitting without anatomical and functional success. Thus, it is desirable that the stent remain in place for a long duration of period, at least 3 months to ensure the complete healing and successful outcome with long-term patency.
Naik has reported a high functional and anatomical success rate (100% & 90 %, respectively) [2]. Likewise, in another study, the functional success rate was 92.85% and the anatomical success rate was 96.87% [13].
In our study, anatomical success was achieved in 18 (85.71%) out of 21 cases. Similarly, functional success was achieved in 22 cases (84.61%) out of total 26.
Conclusion
Any eyelid injury involving the medial canthus should be suspected for canalicular injury and managed accordingly. Reconstruction of lacrimal canalicular injuries requires canalicular stenting. We recommend the use of monocanalicular stent for canalicular laceration repair as the technic is simple, minimally invasive and very effective with high anatomical and functional success. The successful outcomes were observed even in the case who presented late with delayed surgical repair. Hence, it is advisable to attempt the surgical repair with the stent in all cases of canalicular injuries.
Limitations
This study was retrospective study with inherent limitations. A prospective, randomized comparative study is needed with different treatment modalities. Anatomical success could not be evaluated among 5 pediatric cases due to limitations of performing syringing and probing in those patients.
Disclosure
The authors report no conflicts of interest in this work.
References
- Herzum H, Holle P, Hintschich C (2001) Eyelid injuries: epidemiological aspects. Ophthalmologe 98: 1079–1082.
- Naik MN, Kelapure A, Rath S, Honavar SG (2008) Management of canalicular lacerations: epidemiological aspects and experience with Mini-Monoka monocanalicular stent. Am J Ophthalmol 145: 375–380.
- Kennedy RH, May J, Dailey J, Flanagan JC (1990) Canalicular laceration. An 11-year epidemiologic and clinical study. Ophthal Plast Reconstr Surg 6: 46–53.
- Forbes BJ, Katowitz WR, Binenbaum G (2008) Pediatric canalicular tear repairs–revisiting the pigtail probe. J AAPOS 12: 518–520.
- Cho SH, Hyun DW, Kang HJ, Ha MS (2008) A simple new method for identifying the proximal cut end in lower canalicular laceration. Korean J Ophthalmol 22: 73–76.
- Wulc AE, Arterberry JF (1991) The pathogenesis of canalicular laceration. Ophthalmology 98: 1243–1249.
- Anastas CN, Potts MJ, Raiter J (2001) Mini Monoka silicone monocanalicular lacrimal stents: Subjective and objective outcomes. Orbit Amst Neth 20: 189–200.
- Leibovitch I, Kakizaki H, Prabhakaran V, Selva D (2010) Canalicular lacerations: repair with the Mini-Monoka monocanalicular intubation stent. Ophthalmic Surg Lasers 41: 472–477.
- Alam MS, Mehta NS, Mukherjee B (2017) Anatomical and functional outcomes of canalicular laceration repair with self retaining mini-MONOKA stent. Saudi J Ophthalmol 31: 135–139.
- Reifler DM (1991) Management of canalicular laceration. Surv Ophthalmol 36: 113-132.
- Singh S, Ganguly A, Hardas A, Tripathy D, Rath S (2017) Canalicular lacerations: factors predicting outcome at a tertiary eye care centre. Orbit 36: 13–18.
- Jordan D, Ziai S, Gilberg S, Mawn L (2008) Pathogenesis of canalicular lacerations. Ophthal Plast Reconstr Surg 24: 394–398.
- Selam Y S, Halil H C, Burcu D, Mehmet D, Sönmez C, et al. (2015) Reconstructions of Traumatic Lacrimal Canalicular Lacerations: A 5 Years Experience. The Open Access J Sci and Tech 3: 1-6.
- Wu S-Y, Ma L, Chen RJ, Tsai Y-J, Chu Y-C (2010) Analysis of bicanalicular nasal intubation in the repair of canalicular lacerations. Jpn J Ophthalmol 54: 24–31.
- Kersten RC, Kulwin DR (1996) ‘‘One-stitch’’ canalicular repair. A simplified approach for repair of canalicular laceration. Ophthalmology 103: 785–789.
- Fayet B, Bernard JA, Ammar J, Karpouzas Y, Hamici S, et al. (1988) Recent wounds of the lacrimal duct. Apropos of 262 cases treated as emergencies. J Fr Ophtalmol 11: 627-637.
- Bersani TA (1999) Nasolacrimal Duct probing and intubation in M. A. Daniel, Blackwell science, 1384–1395.
- Snead JW, Rathbun JE, Crawford JB (1980): Effects of the silicone tube on the canaliculus; an animal experiment. Ophthalmology 87: 1031–1036.
- Kaufman LM, Guay-Bhatia LA (1998) Monocanalicular intubation with Monoka tubes for the treatment of congenital nasolacrimal duct obstruction. Ophthalm 105: 336-341.
- Kersten RC, Kulwin DR (1996) ‘One-stitch’canalicularrepair: A simplified approach for repair of canalicular laceration. Ophthalm 103: 785–789.
- Liang T, Zhao G, Li Y, Yang S, Zhang L, et al. (2009) Efficiency and therapeutic effect of modified pigtail probe in anastomosing lacerated lacrimal canaliculus, Chin J Traumatol 12: 87–91.
- Drnovsek-Olup B, Beltram M (2004) Trauma of the lacrimal drainage system: Retrospective study of 32 patients. Croat Med J 45: 292–294.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi