Case Report, J Otol Rhinol Vol: 8 Issue: 1
Debride and Conquer: A New Angle in Endoscopic Removal of Antrochoanal Polyps
Clare SM Hutchinson1*, Fearghal Toner2 and Keith Trimble3
1Plastic Surgery, Ulster Hospital, Dundonald, Belfast BT16 1RH, UK
2ENT Royal Victoria Hospital, Belfast, Northern Ireland, UK
3Consultant Paediatric Otolaryngology, Royal Belfast Hospital for Sick Children, Belfast, Northern Ireland, UK
*Corresponding Author : Clare Hutchinson
Plastic Surgery, Ulster Hospital Dundonald, 26 Jameson Street, Belfast BT7 2GU, UK
Tel: 07724247789
E-mail: clare_hutchinson@hotmail.co.uk
Received: January 22, 2019 Accepted: February 11, 2019 Published: February 18, 2019
Citation: Hutchinson CSM, Toner F, Trimble K (2019) Debride and Conquer: A New Angle in Endoscopic Removal of Antrochoanal Polyps. J Otol Rhinol 8:1. doi: 10.4172/2324-8785.1000370
Abstract
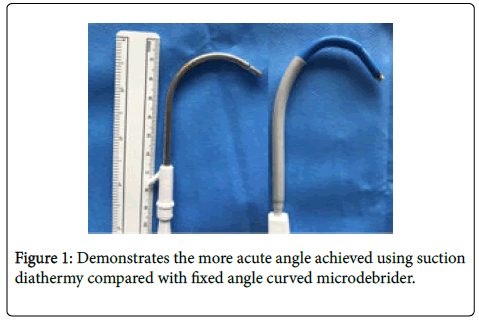
Objective: Antrochoanal Polyps can be problematic to remove fully due to their location and instruments available. Method: Using a combination of paediatric and adult sized instruments, viewed with 30 and 70 degree endoscopes, we could partially remove the polyp through a large middle meatal antrostomy (MMA). Being unable to reach the remaining stalk, despite proceeding to an inferior antrostomy (IA), we realised the need for a more acute-angled instrument. By curving the monopolar Valleylab suction diathermy (MVSD), mimicking the curved microdebrider, we inserted this through our MMA. With an endoscope and a curved ball probe through the IA, we further increased the angle of the MVSD and cauterised the base of the polyp. Results: Clinically the polyp appeared to be fully resected. Conclusion: Consideration must be given to the infraorbital nerve and its relation to the base of the polyp. With this in mind, it is a safe technique.
Keywords: Nasal polyps; Nasal obstruction; Nasal mucosa; Maxillary sinus; Paranasal sinus diseases
Introduction
Antrochoanal Polyps are benign lesions arising from the epithelium of the maxillary sinus. They are more commonly found in young patients, and males are affected more than females. Presentation is most commonly unilateral nasal obstruction, then rhinorrhea [1]. Perhaps the higher incidence of upper respiratory tract infections in children, with associated nasal symptoms is the reason for a more advanced disease presentation in children [2]. Complete surgical excision by endoscopic polypectomy is safe and is the treatment of choice [1]. Unfortunately, the rates of successful resection using endoscopic approach are less in children (88.9%) than a combined approach used in adults (93.1%) [2] and recurrence has been shown to be as high as 29% [3].
Case Report
During a revision excision of antrochoanal polyp pedicled on the anterior wall of the left maxillary sinus in a 12-year-old boy we encountered some difficulty both viewing and removing the lesion. Using a combination of paediatric and adult sized instruments, viewed with 30 and 70 degree endoscopes, we attempted to navigate through a large middle meatal antrostomy (MMA), created during the initial surgical procedure, for access. With these instruments, and with the use of a straight microdebrider, we were able to remove a large proportion of the polyp; however, it was clear that a residual “root” was remaining. Even with assistance from the 70 degrees endoscope, we were unable to fully view its base.
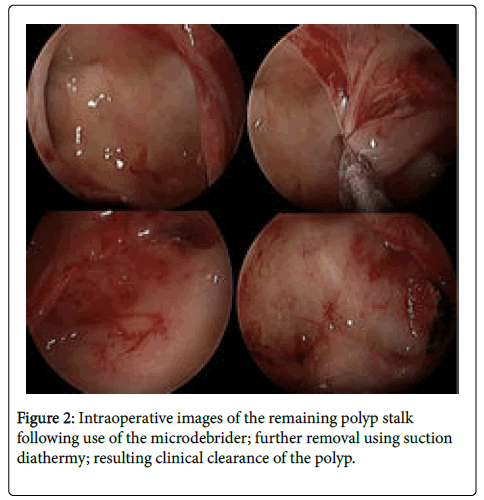
To improve our view, we proceeded to an inferior antrostomy (IA). While the IA allowed us to obtain an excellent view of the base of the polyp in the anterolateral wall of the maxillary sinus we were unable to reach the polyp base via the MMA even with use of the most curved 3.5 mm RAD 120 degree microdebrider blade. We decided to attempt the use of a monopolar Valleylab suction diathermy device to coagulate the base of the polyp and avoid recurrence. Due to its malleability we could manipulate it to the correct length and angle to reach the anterior maxillary wall. By curving the suction monopolar diathermy to mimic the curved microdebrider (Figure 1) we were able to insert this through the MMA. With an endoscope through the IA as well as a curved ball probe, we were able to further increase the angle of the suction diathermy and coagulate the base of the polyp. The infraorbital nerve was identified and avoided using direct endoscopic visualisation. Clinically the polyp appeared to be fully resected (Figure 2). Pathological examination confirmed antrochoanal polyp with chronic inflammatory cell infiltrate and no malignancy or granulomatous disease.
Discussion
The location of these lesions and the instruments available, which means that complete removal, can be problematic. The difficulty achieving complete removal as well as their late presentation in children may contribute to the high rates of recurrence. Whilst they are a rare condition in adults they make up to 33% of polyp disease in children [4-10].
Consideration must be given during excision to the infraorbital nerve and its close relation to the polyp’s base, therefore direct vision during excision is a must. With our technique this is possible. Successful and safe surgery, with complete excision to reduce recurrence, could lead to avoidance of multiple procedures in children. Our preference is to avoid a Caldwell Luc approach and minimize the risk of infraorbital injury. Our technique allowed us to avoid performing any further removal of normal healthy tissue for the purpose of gaining access to the maxillary sinus. While such removal is appropriate in the adult population it can lead to greater incidence of post-op complications such as crusting and bleeding which are much less manageable in the paediatric population.
Conclusion
The anterolateral wall of the maxillary sinus can prove challenging to reach.
Antrochoanal polyps have a high recurrence rate in children (29%).
With limited access due to our patient’s age we were unable to reset the base of an antrochoanal polyp recurrence with conventional instruments.
Using a monopolar Valleylab suction diathermy, moulded to the appropriate angle and length, we were able to achieve a macroscopically clear resection.
References
- Gendeh BS, Long YT, Misiran K (2004) Antrochoanal polyps: Clinical presentation and the role of powered endoscopic polypectomy. Asian J Surg 27: 22-25
- Lee DH, Yoon TM, Lee JK, Lim SC (2016) Difference of antrochoanal polyp between children and adults. Int J Pediatr Otorhinolaryngol 84: 143-146
- Orvidas LJ, Beatty LJ, Weaver AL (2001) Antrochoanal polyps in children. Am J Rhinol 15: 321-325
- Segal N, Gluk O, Puterman M (2012) Nasal polyps in the pediatric population. B-ENT 8: 265-267.
- Yonekawa H (1988) A clinical study of Reinke`s edema. Auris Nasus Larynx 15: 57-78.
- Umeno Kadota H, Yurita S, Adachi K, Inguchi T, Fukushima J, et al. (2010) Case study on vocal fold polyps. Otologia Fukoka 56: 19-23.
- Yanagisawa E, Hausfeld JN, Pensak ML (1983) Sudden airway obstruction due to pedunculated laryngeal polyps. Ann Otol Rhinol Laryngol 92: 340-343.
- Sellami M, Chaabouni MA (2017) Giant laryngeal polyp: An unusual indication of tracheostomy. Pan Afr Med J 26: 76.
- Pathak RD (2000) Fibromyxomalarynx-emergency management. Indian J Otolaryngol Head Neck Surg 52: 177-178.
- Asajima R, Komoda Y, Sai Y, O ku S, Nosaka S (1997) Anesthetic management for the resection of a giant laryngeal polyp: A case report. J Jpn Soc Clin Anes 17: 384-387.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi