Research Article, J Womens Health Vol: 12 Issue: 2
Disparities in Utilization of Mammogram Screening and Incidence of Postmenopausal Metastatic Breast Cancer in Asian American Women
Megan Reddy1*, Arya Aliabadi2, Caitlin R Johnson1, Daniel S Kapp3, John K Chan1 and Cheng-I Liao41California Pacific Medical Center, 795 El Camino Real, San Francisco, CA, 94109, USA
2Department of Obstetrics and Gynecology, University of California Los Angeles, 10833 Le Conte Ave, Los Angeles, CA, 90095, USA
3Department of Radiation Oncology, Stanford University School of Medicine, 875 Blake Wilbur Dr, Stanford, CA, 94304, USA
4Department of Radiation Oncology, Stanford University School of Medicine, 875 Blake Wilbur Dr, Stanford, CA, 94304, USA
*Corresponding Author: Megan Reddy
California Pacific Medical Center
795 El
Camino Real, San Francisco, CA
94109, USA
E-mail: Megan.Reddy@SutterHealth.org
Received: 10 May, 2023, Manuscript No. JWHIC-23-98334;
Editor assigned: 12 May, 2023, PreQC No. JWHIC-23-98334 (PQ);
Reviewed: 26 May, 2023, QC No. JWHIC-23-98334;
Revised: 02 June, 2023, Manuscript No. JWHIC-23-98334 (R);
Published: 12 June, 2023 DOI: 10.4172/2325-9795.1000430.
Citation: Reddy M, Aliabadi A, Johnson CR, Kapp DS, Chan JK, et al. (2023) Disparities in Utilization of Mammogram Screening and Incidence of Postmenopausal Metastatic Breast Cancer in Asian American Women. J Womens Health 12:3.
Abstract
Introduction: The incidence of metastatic breast cancer is rising, but few studies have analyzed Asian American women with a focus on screening and obesity rates.
Methods: Data from the U.S. Cancer Statistics were examined for trends and incidence rates of breast cancer. Using the Center for Disease Control data mammogram compliance and obesity rates in Asian women were analyzed.
Results: Over our 18-year study period, the incidence of postmenopausal metastatic breast cancer increased by 2.19% annually in Asian women compared to only 1.03% in White women. Asians also had higher rates of mammogram non-compliance compared to other racial groups. Of Asians, the rates of obesity in postmenopausal women were highest in those aged 65-74 years.
Discussion: Compared to other races, Asians have the highest increase in the incidence of metastatic breast cancer with lower rates of screening mammograms. Further research is needed to better understand these disparities.
Keywords: Breast cancer screening; Mammogram, Race; Disparities; Obesity; Asian; Postmenopausal
Abbreviations
U.S: United States; USCS: United States Cancer Statistics; SEER: National Cancer Institute’s Surveillance, Epidemiology, and End Results; CDC: Centers for Disease Control and Prevention; BRFSS: Behavioral Risk Factor Surveillance System; AAPC: Average Annual Percent Change; ABPC: Average Biennial Percent Change; CI: Confidence Interval; BMI: Body Mass Index
Introduction
Breast cancer remains the most common cancer and the second most common cause of cancer death among women in the United States. It is estimated that 297,790 new cases of breast cancer and 43,170 deaths will occur in women in 2023, with a rising incidence [1]. Up to six percent of new breast cancer cases are diagnosed in the metastatic stage, and most of these women are postmenopausal [2].
Given that breast cancer is screenable, access to mammography may detect cancers in an early stage before the development of metastases. Prior studies have found that Black and Hispanic women have lower access to and adoption of mammogram screening; however, few studies have focused on the Asian population. In addition to access to healthcare, there is limited information on trends such as obesity among minority subgroups [3].
In this current report, we examined the trends and incidence rates of postmenopausal metastatic breast cancer in Asian American women. Furthermore, we explored risk factors that may be responsible such as obesity rates and lack of screening mammography. We then performed an intersection analysis to identify subgroups at risk based on demographics and geographic regions.
Methodology
Data were obtained from the United States Cancer Statistics (USCS) database from 2001-2018, including the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program, and the Centers for Disease Control (CDC) and Prevention Behavioral Risk Factor Surveillance System (BRFSS) from 2000-2018 for this cross-sectional study [4]. Data were then analyzed for females with postmenopausal breast cancer diagnosed with metastatic disease. Intersection analysis was performed by race, region of location in the U.S, and mammography rates. The incidences and trends of metastatic breast cancer per 100,000 women were calculated using SEER*Stat 8.3.9.2 and the joinpoint regression program 4.9.0.0. The trend was presented as Average Annual Percent Change (AAPC) or Average Biennial Percent Change (ABPC). Trends were characterized by AAPC with 95% Confidence Intervals (CI) and significant if p<0.05. Furthermore, using the CDC data we examined the rates and trends of obesity as Body Mass Index (BMI) ≥ 30 among women by race and age.
Results
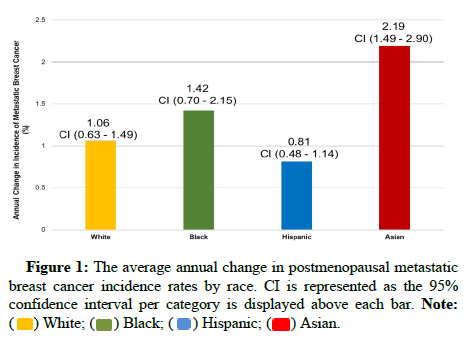
Using USCS data from 2001-2018, we showed that the incidence of metastatic breast cancer increased from 16.58 to 19.48 (per 100,000 women). Over the 18-year study, the incidence rate of metastatic breast cancer increased the most for postmenopausal Asian women at 2.19% annually (p<0.001) compared to only 1.42%, 1.06%, and 0.81% (p<0.001) in Black, White, and Hispanic women, respectively (Figure 1). On intersection analysis, Asian women residing in the U.S. Northeast region were found to have the highest annual increase at 2.52% (p<0.05).
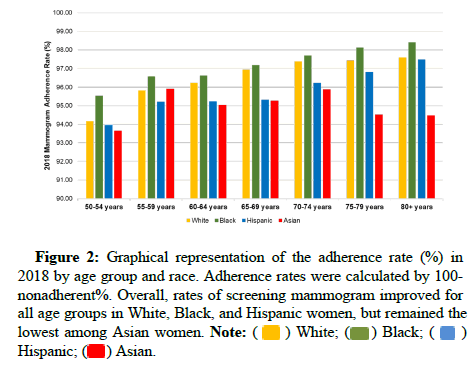
Using the screening data from the Behavioral Risk Factor Surveillance System survey over the 18 years of our study, White, Black, and Hispanic women improved their screening compliance by 3.43%, 3.32%, and 1.24% (p<0.05), whereas the compliance of Asian women did not change (0.80%, p=0.41). More specifically, up to 6.35% of Asian women aged 50-54 never had a mammogram. Rates of mammogram adherence in 2018 by race and age are displayed in Figure 2. Furthermore, on intersectional analysis, we found that over all age groups, Asian women aged 50-54 residing in the West region of the U.S. appear to have the highest rate of non-compliance at 6.50%.
Figure 2: Graphical representation of the adherence rate (%) in 2018 by age group and race. Adherence rates were calculated by 100-nonadherent%. Overall, rates of screening mammogram improved for all age groups in White, Black, and Hispanic women, but remained the lowest among Asian women. Note:
( ) White; (
) White; ( ) Black; (
) Black; ( ) Hispanic; (
) Hispanic; ( ) Asian.
) Asian.
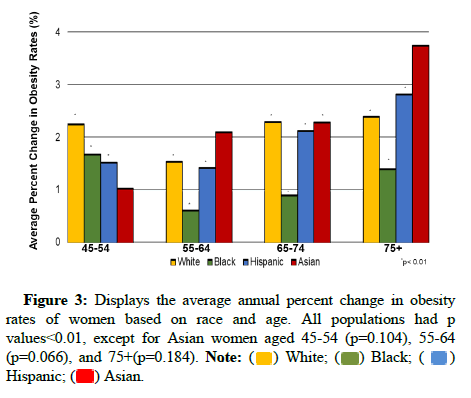
Given previously identified significant risk factors associated with breast cancer, we examined the rates and trends of obesity using the Centers for Disease Control survey data [5]. Our results demonstrated that obesity incidence has been increasing for Asian American women from 9.06 per 100,000 in 2001 to 12.80 per 100,000 in 2016 (p<0.01). Particularly among postmenopausal Asian women, the incidence of obesity increased most in those aged 65-74 years, with an annual increase of 2.29% (p<0.004) as depicted in Figure 3.
Discussion
Over our 18-year study, we found that postmenopausal Asian women had the highest increase in metastatic breast cancer incidence per year. In addition to the increased rates of obesity in this population, Asian women did not have an improvement in mammogram compliance compared to other races.
Similarly to our findings, researchers used the National Health and Nutrition Examination Survey in a population-based study, demonstrating a significant trend of increasing obesity rates in Asian Americans [6]. Although their study only used seven years of data from the U.S., we incorporated data analysis from 2001-2016. Further research is needed to analyze the Asian American population and modifications of BMI threshold for obesity, waist circumference, and abdominal adiposity.
Other researchers have portrayed that Asian Americans are less likely to undergo cancer screening than other races. This disparity may be explained by differences in cultural perceptions of Western medicine, medical literacy, language barriers, environmental exposures, availability of healthcare insurance, and additional social determinants of health [7]. In this current report, our intersection analysis showed that Asians residing in the Western U.S. have high rates of non-compliance, suggesting implications for a pilot project directed at vulnerable populations.
This study is limited by the lack of a single dataset which may account for varying estimates of cases based on the prevalence of the Asian American population. Additionally, our data did not obtain further classification of Asian subgroups and by their immigration status. We also only focused on postmenopausal metastatic breast cancer without regard to subtype or genomic characterization of breast cancers. Future studies are needed to identify further risk factors, gaps in care, and expansion to include other chronic diseases in this demographic.
Our data suggest that tailored population-based interventions aimed at addressing obesity and improving screening mammography are needed for Asian American women who remain at higher risk for postmenopausal metastatic breast cancer.
References
- Siegel RL, Miller KD, Wagle NS, Jemal A (2023). Cancer statistics, 2023. CA Cancer J Clin 73(1):17-48.
[Crossref] [Google Scholar] [Pubmed]
- National Program of Cancer Registries and Surveillance, Epidemiology and End Results Program. Cancer Stat Facts: Female Breast Cancer (2022)
- Ahmed AT, Welch BT, Brinjikji W, Farah WH, Henrichsen TL, et al (2017). Racial disparities in screening mammography in the United States: a systematic review and meta-analysis. J Am Coll Radiol 14(2):157-165.
[Crossref] [Google Scholar] [Pubmed]
- Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. BRFSS Prevalence & Trends Data (2015)
- Devericks EN, Carson MS, McCullough LE, Coleman MF, Hursting SD (2022). The obesity-breast cancer link: a multidisciplinary perspective. Cancer Metastasis Rev. 41(3):607-625.
[Crossref] [Google Scholar] [Pubmed]
- Liu B, Du Y, Wu Y, Snetselaar LG, Wallace RB, et al (2021). Trends in obesity and adiposity measures by race or ethnicity among adults in the United States 2011-18: population based study. BMJ 372:n365.
[Crossref] [Google Scholar] [Pubmed]
- Lee RJ, Madan RA, Kim J, Posadas EM, Yu EY (2021). Disparities in cancer care and the Asian American population. Oncologist 26(6):453-460.
[Crossref] [Google Scholar] [Pubmed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi