Case Report, J Physiother Rehabil Vol: 3 Issue: 1
Effectiveness of Physiotherapy for Children with Spastic Diplegic Cerebral Palsy: A Case Report
Mst Rabea Begum1* and Md Shujayet Goni2
1Paediatric Unit, Physiotherapy Department, Centre for the Rehabilitation of the Paralysed (CRP), Savar, Dhaka, Bangladesh
2Paediatric Unit, Physiotherapy Department, CRP, Savar, Dhaka-1343, Bangladesh
*Corresponding Author : Mst Rabea Begum
Senior Clinical Physiotherapist, Physiotherapy Department, Centre for the Rehabilitation of the Paralysed (CRP), Savar, Dhaka-1343, Bangladesh
Tel: +8801675793257
E-mail: physio_miilee@yahoo.com, drrabea3@gmail.com
Received: March 27, 2019 Accepted: April 15, 2019 Published: April 25, 2019
Citation: Begum MR, Goni MS (2019) Effectiveness of Physiotherapy for Children with Spastic Diplegic Cerebral Palsy: A Case Report. J Physiother Rehabil 3:1. doi: 10.4172/jptr.1000118
Abstract
This case study shows the effectiveness of physiotherapy for 4 years old boy with diplegic cerebral palsy. The aim was to find out the effectiveness of physiotherapy for 4 years old boy with diplegic cerebral palsy to improve gross motor function. Before starting physiotherapy treatment, he had lots of impartments on gross motor function and the GMFCS was III, MACS-II, CFCSI, EDACS-I. This child is still continuing physiotherapy session and GMFCS-I, MACS-I. After receiving intensive physiotherapy improved gross motor function specially standing, walking, stair climbing and jumping as well as improving balance and posture. The Modified ash worth scale, goniometer, GMFM, 10 m walk test and TUG were used as outcome measures. There was markedly improved on gross motor function by physiotherapy for this diplegic cerebral palsy.
Keywords: Cerebral Palsy; Diplegia; Gross motor function
Introduction
Cerebral palsy is one of the motor disorders in children. According to Rosenbaum et al., [1] “Cerebral palsy (CP) describes a group of permanent disorders of the development of movement and posture, causing activity limitations, which are attributed to non-progressive disturbances that occurred in the developing fetal or infant brain. The motor disorders of cerebral palsy are often accompanied by disturbances of sensation, perception, cognition, communication, and behavior, by epilepsy, and by secondary musculoskeletal problems”.
The prevalence of CP is approximately 3 to 4 per 1000 live births in United States. Spastic CP is more common and it is estimated 61% to 76.9% of all Cerebral Palsy cases [2]. In Bangladesh especially in rural area the prevalence of cerebral palsy (CP) is 3.4 per 1000 children. Majority of them were male. The spastic CP accounts for 79.6% [3].
The functional classification system is used to classify the cerebral palsy child. The gross motor function classification system (GMFCS) classifies the gross motor function according to the age group. This system has 5 age banned comprises 0 to 2 years, 2 to 4 years, 4 to 6 years, 6 to 12 and 12 to 18 years. Each age group has 5 levels. Level I has the least problem whereas level V has more problem.
The manual ability function classification system (MACS) is used to distribute the handle objects in activities in daily living for children with cerebral palsy such as eating, dressing, playing, drawing or writing. This scale is valid from 4 to 18 years for cerebral palsy. The MAC has five ordinal levels from I to V. The level I has minor problem, IV and V has more limitation in handle objects [4].
Eating and drinking is classified by eating and drinking ability classification system (EDACS). It describes the five level from I to V for cerebral palsy and applicable for 3 years to older [5]. Communication is categorized by communication function classification system which is valid from 2 to 12 years in children with cerebral palsy. Five levels focus the severity of communication [6].
Case Report
The study was submitted to Research and Monitoring department of CRP. The ethical board received our opinion and permitted to take informed consent from mother. This case study showed the effectiveness of physiotherapy for this child. A boy who was 4 years old and the clinical diagnosis is spastic diplegic CP. This child has no cognitive deficit. The level of GMFCS-I, MACS-I, EDACS-I and CFCSI for him. This child came to CRP in 2016 at Pediatric unit and received admission for 14 days. In this time he has received intensive physiotherapy program.
On that time GMFCS was classified in 2 to 4 aged groups. Her mother’s complain: child was not able to stand and walk independently, always maintain ‘w’ sitting position. This child’s gait was crouch and need hand held mobility. In 2016, a 2 years old boy was diagnosed as spastic diplegic CP. This child came to CRP in 2016 at Pediatric unit and received admission for 14 days. In this time he has received intensive physiotherapy program. The GMFCS was level III. According to the assessment the child was pre-term baby and birth weight was less than 2 kg.
On that time GMFCS was classified in 2 to 4 aged groups. After admission mother of child was decided to take more regular physiotherapy from physiotherapist. But now the level of GMFCS-I and CFCS-I for him. The child has abnormal gait, problem in gait speed, higher function.
The assessment
The subjective and objective assessment was used to find out the problem of this child. The present complains are- present hypertonicity (1+) gait problem (speed, coordination), mild difficulty in higher function (jumping, running), mild tightness in hamstrings (b/l), muscular weakness present weight bearing and shifting problem, slouch posture. To assess the tonicity the physiotherapist used modified ash worth scale (MAS), to assess the hamstring tightness used goniometer, GMFM-66 IS was used to measure gross motor function, 10-meter walk test and time up and go (TUG) for walking speed and balance with AFO.
Physiotherapy treatment
This child is receiving physiotherapy session 3 to 4 sessions per week for 45 minutes in day.
Parental education: Care giver education plays a vital role for any treatment. Therapist was provided instruction to child’s mother about condition, prognosis and physiotherapeutic management.
Slow passive stretching: Though child has present hyper tonicity in lower extremities, slow passive stretching is used to normalize tonicity in 10 repetitions, 1 set, 20 seconds hold in each repetition. The physiotherapist was advised to mother to do this maneuver in this way for 2 times a day.
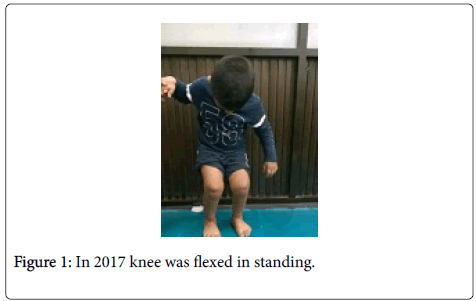
Range of motion exercise: Firstly PROM exercise-10 repetition was applied to maintain normal Passive movement of knee extension and ankle dorsiflexion. In 2017 reduced active knee extension but there was markedly improvement was found in 2019 (Figures 1 and 2).
Balance training: Balance training was applied by using ball throwing and catching practice, reaching practice in standing position with minimum support to improve balance in standing position. Wobble board and physio ball was used in standing to improve pelvic movement which can enhance balance.
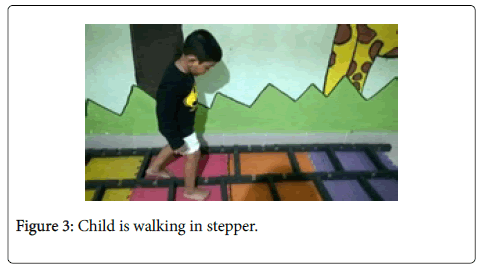
Gait training: To correct gait reeducation was applied in stepper, stepping practice in front of wooden box, weight shifting exercise was practiced for correction walking pattern (Figure 3).
Weight bearing exercise: Static weight bearing exercise was applied by using gaiters in front of wall independently to improving proprioception and weight bearing of lower extremities through knee joint. Standing frame also used for 30 minutes to improve weight bearing. The standing frame helps to reduce the spasticity by inhibiting motor neuron excitability through prolonged stretch [7].
Assistive device
Ankle Foot Orthosis (AFO) was prescribed to educate gait with maintaining proper biomechanics of foot and ankle, leg gaiters for prolonged stretching to normalize tone and maintain normal ROM and also standing frame static bearing of lower extremities. Though reduced gastrocnemius tightness, now child is sometimes using AFO but in standing frame uses AFO.
Gross motor function classification system was used to classify at the level of III when he was admitted on 2016. After receiving regular physiotherapy treatment now this child is in level I in GMFCS. Improved the MACS level, reduced tonicity, reduced hamstring muscle tightness as well as improved balance. This child is also read in class play group and performing better performance in William and Mairy Tailor Schools which is the only one inclusive school in Bangladesh.
The outcome of physiotherapy is shown in Table 1.
| Outcomes | Before treatment | In 2016 (after admission) | In 2019 |
|---|---|---|---|
| Gross motor | Level III | Level III | Level I |
| Handle objects | Not applicable due to age | Not applicable due to age | I |
| Eating and drinking | Not applicable due to age |
Not applicable due to age |
I |
| Communication | Not applicable due to age |
Not applicable due to age |
I |
| Muscle tone | 2 | 2 | 1+ |
| AROM (knee extension) | Loss 35° | Loss 25° | Loss 5 to 10° |
| Weight bearing | Poor | Fair | Good |
| Posture | Poor (slouch) | Improving | Improved |
| GMFM (crawling and kneeling) | Not used | 73.05% | 95.24% |
| GMFM (standing) | Not used | 46.15% | 94.87% |
| GMFM (walking, running and jumping) | Not used | 15.28% | 90.28% |
| 10 m walk test | Unable to do | Not tested | 0.649 m/sec |
| TUG | Unable to do | Not tested | 0.11 m/sec |
Table 1: Distribution of improvement.
Discussion
The aim of this study was to show the effectiveness of physiotherapy on gross motor function for diplegic cerebral palsy. This study showed that physiotherapy is effective for this diplegic boy. Now this child can walk independently though the pattern is not mildly correct. Therefore, improved his gross motor function especially standing, walking, stair climbing, jumping and also balance. In GMFM-88 version used 3 dimensions only. Though child is diplegic he had good rolling, lying and sitting ability. From 2016 this three dimension including crawling and kneeling, standing and walking, running and jumping improved dramatically. Studies showed that intensive physiotherapy is effective on gross motor function for children with cerebral palsy in all dimension of GMFM [8].
When the child was admitted as inpatient services the goal was to provide mother’s education about condition of the child, prognosis and physiotherapeutic management, to prevent secondary complication, to improve standing balance and to educate gait as possible if they continue physiotherapy services regularly. The improvement is dramatically changed. Now the goal is to improve gait, reduce fall and to enhance higher function as well as improve quality of life. The physiotherapist is applying neurodevelopmental therapy, rood’s technique, strength training and gait training. Physiotherapy treatment improved child’s gross motor function, social skills as well as activities of daily living for diplegic cerebral palsy [9].
This case report showed that physiotherapy intervention is effective for diplegic cerebral palsy.
Conclusion
This study focused that physiotherapy treatment is effective to improve gross motor function for the children with cerebral palsy. The insufficiency of literature on the subject, further research is needed with a larger number of participants, in order to better clarify the benefits of the physiotherapy management among cerebral palsy children.
Conflict of Interest
No conflict of interest between the authors.
References
- Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, et al. (2007) A report: The definition and classification of cerebral palsy April 2006. Dev Med Child Neurol 109: 8-14.
- Boyle CA, Boulet S, Schieve LA, Cohen RA, Blumberg SJ, et al. (2011) Trends in the prevalence of developmental disabilities in US children, 1997-2008. Pediatrics 127: 1034-1042.
- Khandaker G, Muhit M, Karim T, Smithersâ€ÂSheedy H, Novak I, et al. (2018) Epidemiology of cerebral palsy in Bangladesh: A populationâ€Âbased surveillance study. Dev Med Child Neurol 61: 601-609.
- Eliasson AC, Krumlinde-Sundholm L, Rösblad B, Beckung E, Arner M, et al. (2006) The Manual Ability Classification System (MACS) for children with cerebral palsy: Scale development and evidence of validity and reliability. Dev Med Child Neurol 48: 549-554.
- Sellers D, Bryant E, Hunter A, Morris C (2017) The eating and drinking classification system (EDACS) for cerebral palsy: Reliability and stability over time. 29th Annual Meeting of the European Academy of Childhood Disability (EACD), Amsterdam RAI Convention Centre, Amsterdam.
- Hidecker MJ, Paneth N, Rosenbaum PL, Kent RD, Lillie J, et al. (2011) Developing and validating the Communication Function Classification System for individuals with cerebral palsy. Dev Med Child Neurol 53: 704-710.
- Pin TW (2007) Effectiveness of static weight-bearing exercises in children with cerebral palsy. Pediatr Phys Ther 19: 62-73.
- Park EY (2016) Effect of physical therapy frequency on gross motor function in children with cerebral palsy. J Phys Ther Sci 28: 1888-1891.
- Midha D, Uttam M, Neb M (2015) Journey of a child with spastic diplegic cerebral palsy from doldrums to hope. Indian J Cereb Palsy 1: 127-130.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi