Research Article, J Otol Rhinol Vol: 7 Issue: 4
Effects of Injectable Aminoglycosides on the Auditory Performance of Individuals with Drug Resistant Tuberculosis in Osun State, Nigeria
Ayo Osisanya1*, Adekunle Adekola2 and Patience Oyeme Fada1
1Audiology and Speech Pathology Unit, Department of Special Education, University of Ibadan, Nigeria
*Corresponding Author : Ayo Osisanya
Audiology and Speech Pathology Unit, Department of Special Education, University of Ibadan, Nigeria
Tel: 08144110703
E-mail: ayoosisanya@gmail.com
Received: Janaury 15, 2018 Accepted: February 02, 2018 Published: February 10, 2018
Citation: Osisanya A, Adekola A, Fada PO (2018) Effects of Injectable Aminoglycosides on the Auditory Performance of Individuals with Drug Resistant Tuberculosis in Osun State, Nigeria. J Otol Rhinol 7:4. doi: 10.4172/2324-8785.1000351
Abstract
Ototoxicity caused by injectable aminoglycosides are capable of causing cochleotoxicity which is characterised as death of auditory hair cells (hearing loss) and vestibulotoxicity manifesting as balance disorders. Ototoxicity is always as a result of insidious effects of aminoglycosides on auditory system, with a kind of irreversible (permanent) hearing loss which is common among individuals being treated for Drug Resistant Tuberculosis (DRTB). Therefore, this study examined the effect of injectable aminoglycosides on the auditory performance of patients with DRTB in Osun state. Twenty (20) DRTB patients comprising of 14 males and 6 females were purposively selected to participate in this ex post facto research. Instruments used include Otoscope to diagnose infection of the middle ear and outer parts of the ear, Maico ST 20 portable diagnostic audiometer to determine the hearing threshold of the participants, and audiograms to record the test results. Baseline audiometry revealed that 35% of the participants had mild hearing loss before commencement of treatment with injectable aminoglycosides, while 70% of the participants had severe to profound hearing loss after completion of injectable aminoglycosides. 65% of the participants had tinnitus in addition to hearing loss, while 55% had high frequency loss only. Therefore, health workers should ensure that people with DRTB are well educated about the side effects of injectable aminoglycosides and be encouraged to access audiologic follow up and rehabilitation, while alternative injectable drugs with reduced or milder side effects are employed for treatment of Drug Resistant Tuberculosis.
Keywords: Auditory performance; Drug resistant tuberculosis; Hearing loss; Injectable aminoglycosides; Tuberculosis; Ototoxicity
Introduction
Hearing is the ability to perceive sounds generated over a wide spectrum of frequencies. Structurally the human ear is sensitive to a frequency band within that spectrum expressed in decibels (dB) and frequencies capable of being heard by humans are called audio or sonic [1]. In humans and other vertebrates, hearing is performed primarily by the auditory system: mechanical waves, known as vibrations are detected by the ear and transduced into nerve impulses that are perceived by the brain (primarily in the temporal lobe). Like touch, audition requires sensitivity to the movement of molecules in the world outside the organism. Both hearing and touch are types of mechano-sensation [2,3]. But with human beings, hearing is very essential and needed for survival as conversation promotes intra and interpersonal relationship in the human world.
This normal conversations use frequencies of 500 to 4,000 Hz at 45 to 60 dB, but after 40 years of age, hearing typically declines gradually. Asides from head trauma, diseases such as meningitis and jaundice noise which are known as common causes of acquired hearing loss, aminoglycosides used for treatment of tuberculosis have also been observed with capacity to cause hearing loss due to its long term use and the toxicity nature of the drugs.
Tuberculosis (henceforth, TB) is one of the leading infectious diseases in the world and it is responsible for more than two million deaths and nine million new cases annually [4]. TB is a major public health problem in Nigeria, a country of 169 million inhabitants, with the country currently ranking 10th among the 22 high TB burden countries of the world and fourth highest in Africa (after South Africa, Ethiopia and DR Congo) Global Tuberculosis Report (2012). All forms of TB globally ranges from 8.7–12.2 million with estimated death of 1.2–1.6 million while in drug resistant tuberculosis cases, between 0.52-0.64 million are infected with 0.16–0.34 deaths (Global Burden of DR-TB, 2015).
Emergence of resistance to drugs used to treat tuberculosis and particularly drug resistant tuberculosis (Henceforth DR-TB) has become an obstacle to effective global TB control [5]. Incomplete and inadequate treatment is the most important factor leading to its development, suggesting that it is often a man-made problem [6]. Inappropriate treatment results in unacceptably low cure rates and the continued spread of tuberculosis in the community because of selection of Mycobacterium tuberculosis isolates that are resistant to anti- tubercular drugs [7]. Taking into consideration the high success rate of TB treatment under Directly Observed Treatment (DOT) policy, the principal cause for the generation of drug resistant TB generally appears to lay in the low degree of patient’s compliance with treatment [8].
In 2013, an estimated 9.0 million people developed TB and 1.5 million died from the disease, while 360,000 of whom were HIVpositive. TB is slowly declining each year and it is estimated that 37 million lives were saved between 2000 and 2013 through effective diagnosis and treatment. Nigeria, being one of the 22 high burden countries for Tuberculosis in the world has a prevalence of 497 per 100, 000 population [9]. In a similar study conducted by Javadi, Abtahi, Gholami, Tabars, and Salamzadeh in the year 2011 on the incidence in amikacin ototoxicity in resistant tuberculosis patients, at Masih Daneshvari Hospital located in Iran and their findings showed a higher prevalence of hearing loss, which is more in the male population than in the female among the population. The study has shown 90% of the male population and 52.38% of the female population. Prior to 2012, there was no national survey to determine the prevalence of tuberculosis disease (TB) in Nigeria. Estimates of the burden of TB in the country relied on indirect assessment by the WHO which is based on the existing TB surveillance data. The accuracy of such estimates largely depends on the quality of the routine surveillance information, which in itself is affected by the completeness of TB notification and instances of TB under-diagnosis. Therefore, it became imperative to conduct a nationwide prevalence survey of TB to obtain a good direct estimate of the burden of TB in the country.
Tuberculosis is a major public health problem in Nigeria, a country of 169 million inhabitants, with the country currently ranking 10th among the 22 high TB burden countries of the world and fourth highest in Africa (South Africa, Ethiopia and DR Congo). In the 2012 Global Tuberculosis Report, WHO’s disease burden estimates, expressed in rates per 100,000 population, were 161 (25- 420) for prevalence and 108 (50-186) for incidence. TB deaths (1.1 million among HIV-negative people and 0.4 million among HIVpositive people). These summations are higher than those included in the 2013 global TB report, primarily because of upward revisions to estimates of the number of TB cases and deaths in Nigeria following the finalization of results from the country’s first-ever national TB prevalence survey (completed in 2012). Given the size of the population and the high TB burden in Nigeria, these revisions have affected global estimates. Though most TB cases and deaths occur among men, the burden of disease among women is also high. In 2013, there were an estimated 3.3 million cases and 5,10,000 TB deaths among women, as well as an estimated 5,50,000 cases and 80,000 deaths among children. TB mortality is unacceptably high given that most deaths are preventable if people can access health care for a diagnosis and the correct treatment is provided. Short-course regimens of first-line drugs that can cure around 90% of cases have been available for decades.
In 2010, 8.8 million people fell ill with Tuberculosis globally, and a total of 1.4 million people died as a result of the disease, most of these cases and deaths (about 95%) are occurring in developing countries. The disease which affects both adults and children remains a major cause of mortality despite availability of effective treatment [10]. The Human Immunodeficiency virus (HIV) epidemic has triggered an increase in the number of TB cases globally. HIV infection and tuberculosis are common and often co-occurring conditions, forming a lethal combination, each speeding the other’s progress, and resultant increase in mortality. Also an issue of global concern presently is the emergence of drug-resistant tuberculosis, which is on the increase in many countries of the world.
Tuberculosis is both curable and preventable. WHO recommended strategy for global tuberculosis control which is a shortcourse, clinically administered treatment [11]. This Directly Observed Treatment short-course (DOTS) has been found to be an effective means of administering anti-TB drugs, significantly reducing the rates of relapse and drug resistance as well as improving the treatment compliance rate [12,13]. Default rate ranged between 20% and 44.2% as reported by previous studies [14-17]. Treatment default or poor adherence to treatment means patient remain infectious for longer and are more likely to relapse, could result in treatment failure as well as foster emergence of drug resistant tuberculosis [12,14,17,18]. It has also been shown that defaulters have the tendency to default again [17] and 20% defaulters in Babatunde et al. [19] certain factors have been found in previous studies to be contributory to poor treatment outcomes among TB patients. HIV co-infection is a very important factor for default and mortality in tuberculosis patients [10,16,18,20-22]. Delay in tuberculosis diagnosis has been identified as a risk factor for failure to comply with treatment, while non-consent for HIV testing was also identified as a factor for poor treatment outcome [11].
Aminoglycosides were introduced in the 1940’s and are highly effective treatment for DR-TB and gram negative infection [23]. The ototoxic effects of aminoglycosides shortly became more evident after their introduction and have limited their use although in developing countries they are still widely used due to their broad antimicrobial spectrum and low cost [24]. People with TB require retreatment when they fail or default from initial treatment or relapse following initial treatment success.
In aminoglycoside ototoxicity, hearing loss initially occurs in the high frequencies (6000 and 8000 Hz for conventional audiometry) and may progress to the lower frequencies, thus affecting speech intelligibility. The hearing loss may begin shortly after the initiation of treatment or may initially appear several days after treatment. Tange et al. [25] reported that 8 of the 23 cisplatin-treated patients they studied demonstrated significant auditory changes above 8000 Hz. Thus, the inclusion of high-frequency audiometry in monitoring these patients is advisable [26].
According to Fausti et al. [26], Follow-up testing 2 years later revealed total recovery for one patient, but continued deterioration for the other patient and also reported the case of one patient whose audiograms indicated further deterioration of hearing across the frequency range during a follow-up test 5 weeks post treatment. The final follow-up, however, revealed no further changes.
In line with WHO/IAUTLD recommendation and available local evidence, Drug-Resistant TB in Nigeria is currently treated with a standardized second-line anti-TB drugs for a minimum period of 20 months [28].
Standardized second-line anti-TB drugs for Nigeria:
8 months of intensive phase: which represents the period of injectable agent, i.e. Kanamycin is used in addition with pyrazinamide, Cycloserine, Levofloxacin and Prothionamide.
12 months of continuation phase: which is the period after the injectable is stopped and the other four mentioned drugs above are continued [28].
According to Moore et al. [29] the risk factors for aminoglycosideinduced ototoxicity include the following:
1. Renal dysfunction: Aminoglycosides are primarily excreted by the kidney; hence serum aminoglycoside levels can increase with renal dysfunction.
2. Advanced age
3. Bacteraemia
4. Cumulative dose
5. Concomitant ototoxic drugs
6. Higher serum aminoglycoside concentrations
7. Genetic predisposition
Hearing loss caused by array of ototoxic drugs is often dosedependent and sometimes can be reversed when the drug therapy is discontinued (e.g. loop diuretics, quinine, salicylates). Sometimes, the damage could be permanent where the hearing loss will be irreversible. Ototoxic medications known to cause permanent damage include all commonly used aminoglycoside antibiotics, such as gentamicin (family history may increase susceptibility), streptomycin, amikacin, kanamycin and neomycin. They all affect the vestibular system (organ of balance) as well as the cochlea although streptomycin has a greater effect on the former and neomycin acts mainly on the latter [30].
Aminoglycoside antibiotics are used in the treatment of gramnegative bacterial infections like tuberculosis; tularemia and other hospital acquired serious infections. Dose-limiting side effects include cochlear and/or vestibular toxicity and nephrotoxicity. Cochlear toxicity is primarily due to death of outer hair cells in the organ of Corti [1]. In Rybak et al. [31], the outer hair cells in the part of the cochlear where high frequencies are detected, die first but successively lower frequencies are then affected. Loss of inner hair cells follows after some delay. The treatment of DR-TB cannot rely upon isoniazid and rifampicin, the two most powerful drugs for the treatment of tuberculosis [32]. Thus, depending on the individual susceptibility pattern, residual first-line oral drugs must be appropriately combined with additional second line drugs comprising injectable aminoglycosides (amikacin, kanamycin, capreomycin), fluoroquinolones (ciprofloxacin, ofloxacin, levofloxacin, moxifloxacin, gatifloxacin), old bacteriostatic second line antituberculosis agents (ethionamide, protionamide, cycloserine, paraamino salicylic acid, thiocetazone) and anti-tuberculosis agents with unclear efficacy (clofazimine, amoxicillin/clavuanate, clarithromycin, linezolid) [5].
A crucial issue related to long-term administration of the injectable group is toxicity. Ototoxicity and nephrotoxicity are well recognized as dose-related adverse effects of aminoglycosides [33]. Ototoxicity and nephrotoxicity have been of major concern because of the narrow therapeutic range of these agents and the wide variability in pharmacokinetics among patients [34]. Amikacin is a semi-synthetic aminoglycoside and shows excellent activity against Mycobacterium tuberculosis and atypical mycobacteria and has been used in the treatment of disseminated atypical Mycobacterium infection in AIDS patients. As well Kanamycin, an antibiotic elaborated by Streptomyces kanamyceticus has shown activity against Mycobacterium tuberculosis. But as the therapy of this disease is protracted and involves the administration of large total doses of the drug, with the risk of ototoxicity and nephrotoxicity, kanamycin should be used only in infection with organisms that are resistant to the most commonly used agents [35]. It is more toxic to cochlea with well documented ototoxicity but is still being commonly used in clinical settings (in developing countries) for DR-TB where cost considerations are a major factor in patient compliance (because of having one fourth the cost of amikacin and one tenth the cost of capreomycin) [36].
Capreomycin is an antimicrobial cyclic peptide elaborated by Streptomyces capreolus and is effective both in vitro and in experimental tuberculosis. It has proven to be of value in the therapy of ‘resistant’ or treatment failure tuberculosis when given with ethambutol or isoniazid [37]. The toxicity profile of capreomycin is similar to that of aminoglycosides and has been discussed along with aminoglycosides in the present study [38]. Cost of therapy with capreomycin is quite high compared to amikacin and kanamycin and is used only in few patients of DR-TB showing resistance to amikacin and kanamycin. Initial ototoxic drug exposure typically affects cochlear regions coding the high frequencies. Continued exposure results in spread of damage to progressively lower frequencies. Early identification of ototoxic hearing loss provides physicians the opportunity to adjust the therapeutic treatment in order to minimize or prevent hearing loss requiring rehabilitation, depending on a patient’s overall treatment picture [39,40]. The present study was conducted to study the effect of second line aminoglycosides (amikacin, kanamycin and capreomycin) on the hearing status in patients of DR-TB after long term use as a part of multi-drug therapy.
Ototoxicity is the major irreversible toxicity of aminoglycosides. Cochlear damage can produce permanent hearing loss, while damage to vestibular apparatus results in dizziness, ataxia and/or nystagmus. Aminoglycosides appear to generate free radicals within the inner ear, with subsequent permanent damage to sensory cells and neurons resulting in permanent hearing loss [41]. Different studies have reported hearing loss as an adverse drug reaction in patients of DR-TB ranging from 6–18% [32,42-45]. The finding that higher frequencies are involved before the lower frequencies may be used as a monitoring procedure for the detection of ototoxicity and has the potential for minimizing irreversible communication deficits in patients receiving aminoglycoside therapy [46]. In all the patients showing hearing loss, the aminoglycoside was stopped and changed to another second line drug done. Incidence of hearing loss may have been reduced because the aminoglycoside was stopped immediately at the outset of ototoxicity and substituted with another second line drug.
The first row outer hair cells (OHCs) in the basal turn tend to be affected earlier than inner apical cells and type I cells are affected before type II cells. The progression of hair cell loss in cochlea tends to be from basal to apical and from OHCs to inner hair cells (IHCs) to supporting cells to more central neural structures like spiral ganglion cells [47]. This stepwise progression of damage explains the clinical findings of high frequency hearing loss occurring first with ototoxic drugs.
Consequent upon the above, the study is designed to investigate the prevalence and patterns of hearing loss among the individuals treated with aminoglycosides due to drug resistant tuberculosis in Osun state, Nigeria.
Purpose of study
The main purpose of this study was to survey the prevalence and pattern of hearing loss among patients with Drug Resistant tuberculosis in Osun state, Nigerian.
Research questions
The following questions were raised to guide the study:
what is the prevalence of hearing loss before treatment with aminoglycosides?
what is the prevalence of hearing loss after treatment with aminoglycosides?
what is the prevalence of high frequency loss among the participants?
what is the incidence of tinnitus among persons treated with aminoglycosides?
Methods
Twenty (20) participants which comprised of Fourteen (14) male and Six (6) female classified as having drug resistant tuberculosis within age range of 15 and 55 years were involved in this research. The participants were purposively selected as individuals being treated for drug resistant tuberculosis within the age range of 15 and 55 years.
The research adopted the descriptive research design of the expostfacto type. This research design was adopted because it helped to describe record, analyse, and interpret the condition that exists naturally.
Three instruments were used for the study namely, otoscope, audiometer and audiogramme.
In order to identify the participants for the study, the assessment procedure was in two stages. At the first stage, relevant information such as personal data, health status, auditory function, risk factors of hearing loss and so on were obtained from the participants and then each participant was screened with a clinical otoscope which was used to look into their ear canals. This was done to screen for ear symptoms, presence of cerumen (ear wax), shed skin, pus, canal skin edema, foreign body, and various ear diseases that could obscure any view of the eardrum and also severely compromise their eligibility for the second stage of the assessment which was audiometric evaluation.
The second stage was carried out in a sound free environment with a patient at a time, and appropriate instruction was given to each participant. MAICO ST 20 diagnostic audiometer was used to determine the degrees, types and hearing configurations of all the participants during which headphone was placed on the ears of each participant and different pure tone was introduced into their ears to elicit response according to instruction given. This procedure was applied to all participants until each hearing threshold was established. Results were recorded on the audiogramme for further interpretation.
The data collected was then analyzed with the use of descriptive statistics of frequency count and percentage.
Results
Research question 1: what is the prevalence of hearing loss before treatment with aminoglycosides?
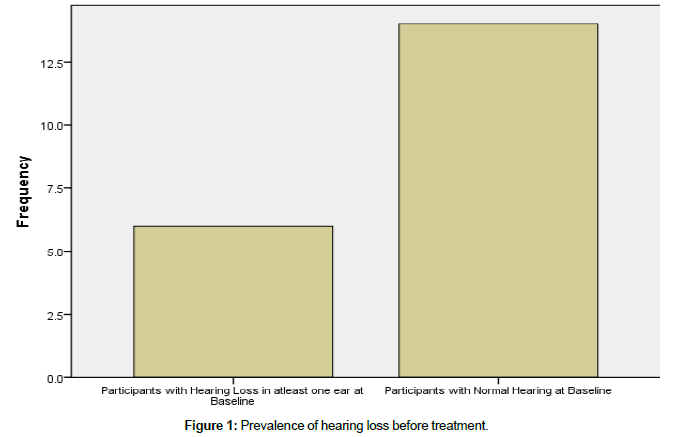
Figure 1 showed that 65% of the participants had a normal hearing threshold before commencing treatment with the use of aminoglycoside injectables while 35% of the participants had hearing loss at mild – moderate level. This implies that majority of patients commence treatment with their hearing apparatus and functionality intact.
Research question 2: what is the prevalence of hearing loss after treatment with aminoglycosides?
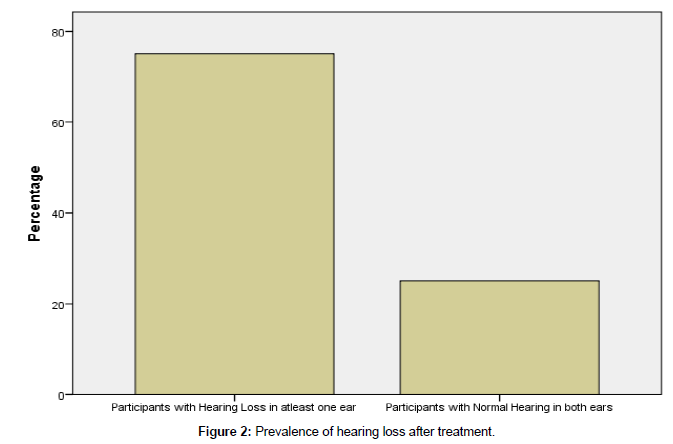
Figure 2 showed that 15 (75%) of the participants had hearing loss in at least one ear after commencement of treatment for DRTB with aminoglycosides while 5 (25%) participants still maintained their normal hearing even after treatment. The implication of this is that prolonged use aminoglycosides to treat DRTB leads to hearing loss amongst participants.
Research question 3: what is the prevalence of high frequency loss among the participants?
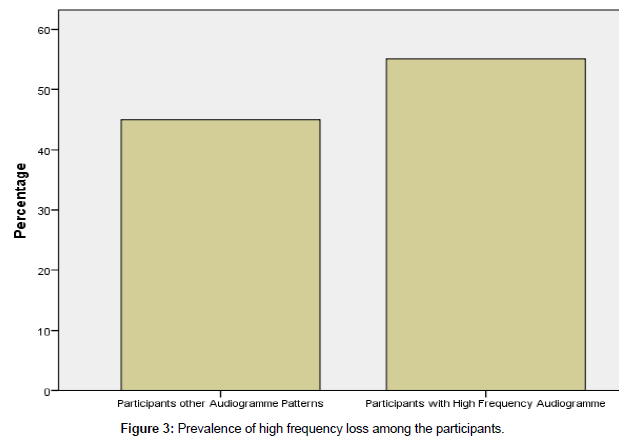
Figure 3 revealed that 11 (55%) of the participants had high frequency audiogramme pattern while 9 (45%) of the participants had other forms of audiogrammes. The implication of this is that participants treated with aminoglycosides usually have a high frequency audiogramme indicating the presence of high frequency loss.
Research Question 4: what is the incidence of tinnitus among persons treated with aminoglycosides?
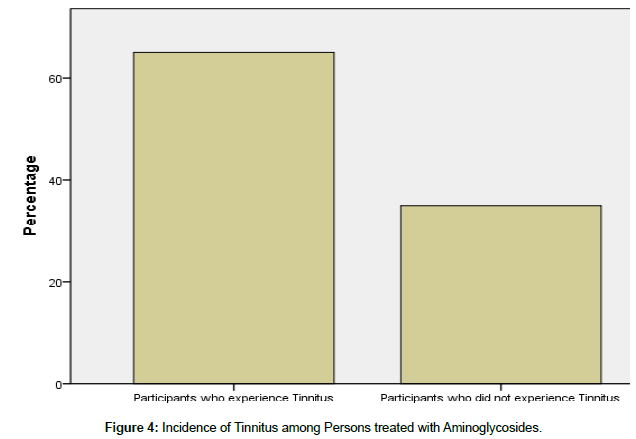
Figure 4 showed that 13 (65%) of the participants had tinnitus while 7 (35%) of the participants did not experience tinnitus during the study. This implies that participants who undergo treatment for DRTB with the use of aminoglycosides usually experience tinnitus.
Discussion of Findings
Prevalence of hearing loss among persons treated with Aminoglycosides
This study revealed that 70% of the participants had normal functional auditory apparatus while 30% had hearing loss in atleast one ear before commencing treatment with aminoglycosides. This implies that normal hearing acuity is prevalent among patients before commencement of treatment but at the end of the studies, 75% of the DR-TB patients had Hearing Loss in atleast one ear while 25% of the participants did not have Hearing Loss in any ear at the end of the treatment with aminoglycosides. This implies that majority of patients with DR-TB have Hearing Loss after commencement of treatment. Based on the above distribution of percentage of individuals with hearing loss in at least on ear, it is evident that hearing loss is prevalent among the individuals with DR-TB after treatment with aminoglycosides. This study corroborated with the findings of Petersen et al. [48] recorded that hearing loss among participants under treatment of DR-TB with aminoglycosides varied from 7-90% of the patients done with the treatment [49-60].
Prevalence of high frequency loss among persons treated with Aminoglycosides
This study has revealed that 55% of the participants had High Frequency pattern of the audiogram while 45% was distributed among other patterns of audiograms. This is in line with previous studies which have postulated that High Frequency Loss (HFL) is prevalent among patients with DR-TB. This study corroborates with the findings of Olaosun et al. [61]. The implication of this study is that HFL occurs among DR-TB treatment using aminoglycosides [62-64].
Prevalence of tinnitus among persons treated with Aminoglycosides
This study reveals that 65% of the participants experience tinnitus while 35% do not experience tinnitus which indicates that individual under treatment for drug resistant tuberculosis experiences tinnitus. This corroborated with the findings of Bauman et al. [65] showed that tinnitus is a form of the cochlear side effects of ototoxicity which was also stated in Duthey et al. [1].
Conclusion
This study investigated and provided first-hand information on the incidence of hearing loss among individuals with tuberculosis being treated with aminoglycosides in Osun state of Nigeria. In addition, the study examined the effect of aminoglycoside drugs on hearing mechanism and thereby indicating patterns of hearing loss among individuals treated for drug resistant tuberculosis. Bearing this in the mind, relevant literatures were reviewed; data were collected through the Pure Tone Audiometry machine, analysed and interpreted. The results of this study corroborated with some existing results which had established correlation between the dependent variables and dependent variable and also contradict other studies. The following are the findings of the study: The study revealed the Patients under treatments with aminoglycosides are more likely to have hearing loss than not and among the patients that is treated with aminoglycosides; the study also revealed that the audiograms of patients under aminoglycosides treatment will first reflect in a high frequency pattern and type of hearing loss and with treatment continuation; the patients develop usually within the mild to moderate range of hearing loss which is almost not noticed by the patient; and the research revealed patients under aminoglycosides treatment will likely experience tinnitus than not during the course of treatment and even after treatment in some cases.
Recommendations
Based on the findings of this study, the following recommendations were made:
On the use of aminoglycosides
Safer and milder drugs with less toxicity rate should be used instead of amikacin and kanamycin in the treatment of individuals with drug resistant tuberculosis.
Possible prolonged period of aminoglycoside injectable should be staggered to 3-4 days per week instead of daily usage to reduce the rate of incidence of hearing loss and other associated comorbid disorder.
On hearing preservation
i. Frequent and correspondent audiological assessments should be encouraged, for this will help in monitoring the functional and non-functional auditory systems of the participants under treatment.
ii. Baseline Pure Tone Audiometry (PTA) should be done before the treatment commence.
iii. Patients with slight deviation from pure tone audiometric baseline results should be considered as much as be treated with safer injectables, like capreomycin with fewer side effects immediately the deviation is observed during follow up audiological assessments.
iv. Other side effects of using aminoglycosides should be evaluated alongside with PTA
v. Clinical trials of other drugs with lesser toxicity should be considered.
vi. Concerted effort should be geared towards awareness and advocacy about management of DRTB.
References
- Duthey B (2013) Priority medicines for europe and the world:“a public health approach to innovation. WHO Background paper.
- Kung C (2005) A possible unifying principle for mechanosensation. Nature 436: 647.
- Peng AW, Salles FT, Pan B, Ricci AJ (2011) Integrating the biophysical and molecular mechanisms of auditory hair cell mechanotransduction. Nat Commun 2: 523.
- Harris T, Heinze BM (2013) Tuberculosis (TB), aminoglycoside and HIV-related hearing loss.
- World Health Organization (2006) Guidelines for management of drug resistant tuberculosis. Geneva, Switzerland.
- Sharma SK, Alladi M (2006) Multidrug resistant T B: a menace that threatens to destabilize tuberculosis control. Chest130: 261-272.
- Schluger NW, Harkin TJ, Rom WN (1996) Principles of therapy of tuberculosis in the modern era: In Tuberculosis, Rom WN, Garay S (eds). Brown and company, New York, USA.
- Volmink J, Graner P (2007) Interventions for promoting adherence to tuberculosis management. Cochrane Database Syst Rev.
- World Health Organization (2010) Roadmap for rolling out XpertMTB/RIF for rapid diagnosis of TB and MDR-TB. Geneva, Switzerland.
- Burton NT, Forson A, Lurie MN, Kudzawu S, Kwarteng E, et al. (2011) Factors associated with mortality and default among patients with tuberculosis attending a teaching hospital clinic in Accra, Ghana. Trans R Soc Trop Med Hyg 105: 675-682.
- Rojas CM, Villegas SL, Piñeros HM, Chamorro EM, Durán CE, et al. (2010) Clinical, epidemiological and microbiological characteristics of a cohort of pulmonary tuberculosis patients in Cali, Colombia. Biomedica 30: 478-481.
- Erhabor GE, Aghanwa HS, Yusuph M, Adebayo RA, Arogundade FA, et al. (2000) Factors influencing compliance in patients with tuberculosis on directly observed therapy at Ile-Ife, Nigeria. East Afr Med J 77: 5.
- Erhabor GE, Adewole O, Adisa AO, Olajolo OA (2003) Directly observed short course therapy for tuberculosis--a preliminary report of a three-year experience in a teaching hospital. J Natl Med Assoc 95: 1082.
- Salami AK, Oluboyo PO (2003) Management outcome of pulmonary tuberculosis: a nine year review in Ilorin. West Afr J Med 22: 114-119.
- Daniel OJ, Oladapo OT, Alausa OK (2006) Default from tuberculosis treatment programme in Sagamu, Nigeria. Niger J Med 15: 63-67.
- Belo MT, Luiz RR, Teixeira EG, Hanson C, Trajman A (2011) Tuberculosis treatment outcomes and socio-economic status: a prospective study in Duque de Caxias, Brazil. Int J Tuberc Lung Dis 15: 978-981.
- Saka D, Aydogdu M, Calisir HC, Cimen F, Ogretensoy M (2011) The treatment results of retreatment pulmonary tuberculosis patients in our clinic. Tuberks toraks 59: 111-119.
- Muture BN, Keraka MN, Kimuu PK, Kabiru EW, Ombeka VO, et al. (2011) Factors associated with default from treatment among tuberculosis patients in nairobi province, kenya: A case control study. BMC Public Health 11: 696.
- Babatunde OA, Elegbede OE, Ayodele LM, Ojo OJ, Ibirongbe DO, et al. (2012) Two Year Trend Analysis of Default Rate in Tuberculosis Patients in Federal Medical Center, Ido-Ekiti, Ekiti State, Nigeria. J Asian Scient Res 2: 798.
- Arentz M, Narita M, Sangaré L, Kah JF, Low D, et al. (2011) Impact of smear microscopy results and observed therapy on tuberculosis treatment in Mombasa, Kenya. IntJ Tuberc Lung Dis 15: 1656-1663.
- Bassett IV, Chetty S, Wang B, Mazibuko M, Giddy J, et al. (2012) Loss to follow-up and mortality among HIV-infected people co-infected with TB at ART initiation in Durban, South Africa. J Acquir Immune Defic Syndr 59: 25.
- Nansera D, Bajunirwe F, Elyanu P, Asiimwe C, Amanyire G, et al. (2012) Mortality and loss to follow-up among tuberculosis and HIV co-infected patients in rural southwestern Uganda. Int J Tuberc Lung Dis 16: 1371-1376.
- Tran Ba Huy P, Bernard P, Schacht J (1986) Kinetics of gentamicin uptake and release in the rat.Comparison of inner ear tissues and fluids with other organs. J Clin Invest 77: 1492-1500.
- Saunders JE, Greinwald JH, Vaz S, Guo Y (2009) Aminoglycoside ototoxicity in Nicaraguan children: patient risk factors and mitochondrial DNA results. Otolaryngol Head Neck Surg 140: 103-107.
- Tange RA, Dreschler WA, van der Hurst RJMA (1985) The importance of high tone audiometry in monitoring of ototoxicity. Arch Otolaryngol 242: 77-81.
- Yung MW, Dorman EB (1986) Electrocochleography during intravenous infusion of cisplatin. Arch Otolaryngol 112: 823-826.
- Fausti SA, Rappaport BZ, Schechter MA, Frey RH, Ward TT, et al. (1984) Detection of aminoglycoside ototoxicity by high-frequency auditory evaluation: selected case studies. Am J Otolaryngol 5: 177-182.
- National Tuberculosis and Leprosy Control Programme, Annual Report 2008. Abuja: NTBLCP, Nigeria.
- Moore RD, Lietman PS, Smith CR (1987) Clinical response to aminoglycoside therapy: importance of the ratio of peak concentration to minimal inhibitory concentration. J Infect Dis 155: 93-99.
- Forge A (2012) Mechanisms of Hearing Loss of Cochlear Origin. Nova Science Publishers, New York USA.
- Rybak LP, Whitworth CA, Mukherjea D, Ramkumar V (2007) Mechanisms of cisplatin-induced ototoxicity and prevention. Hearing research 226: 157-167.
- Espinal MA (2003) The global situation of MDR-TB. Tuberculosis 83: 44-51.
- De Jager P, Van Altena R (2002) Hearing loss and nephrotoxicity in long-term aminoglycoside treatment in patients with tuberculosis. Int J Tuberc Lung Dis 6: 622-627.
- Ackerman BH, Bailie GR, Zaske DE (1984) Aminoglycoside therapy: Improving patient response and safety. Postgraduate medicine 75: 177-185.
- Chambers HF, Sande MA (1996) The Aminoglycosides: In The Pharmacological Basis of Therapeutics, McGraw-Hill, New York, USA.
- Matz GJ (1993) Aminoglycoside cochlear ototoxicity. Otolaryngol Clin North Am 26: 705-712.
- Mandell GL, Petri WA (1996) Drugs used in chemotherapy of tuberculosis, mycobacterium avium complex disease and leprosy: In The Pharmacological Basis of Therapeutics. McGraw-Hill, New York, USA.
- Hesling CM (1969) Treatment with capreomycin, with special reference to toxic effects. Tubercle 50: 39-41.
- Campbell KC, Durrant J (1993) Audiologic monitoring for ototoxicity. Otolaryngol Clin North Am 26: 903-914.
- Fausti SA, Helt WJ, Gordon JS, Reavis KM, Philips DS, et al. (2007) Audiologic monitoring for ototoxicity and patient management. Thomson-Delmar Learning, New York, USA.
- Selimoglu E (2007) Aminoglycoside-induced ototoxicity. Curr Pharm Des 13: 119-126.
- Nathanson E, Gupta R, Huamani P, Leimane V, Pasechnikov AD, et al. (2004) Adverse events in the treatment of multidrug resistant tuberculosis: results from the DOTS-Plus initiative. Int J Tuberc Lung Dis 8: 1382-1384.
- Jaramillo E (2008) Guidelines for the programmatic management of drug-resistant tuberculosis. World Health Organization, Geneva, Switzerland.
- Furin J, Mitnick C, Shin S, Bayona J, Becerra M, et al. (2001) Occurrence of serious adverse effects in patients receiving community based therapy for multidrug resistant tuberculosis. Int J Tuberc Lung Dis 5: 648-655.
- Wang S, Bian Q, Liu Z, Feng Y, Lian N, et al. (1999) Capability of serum to convert streptomycin to cytotoxin in patients with aminoglycoside-induced hearing loss. Hear Res 137: 1-7.
- Fausti SA, Rappaport BZ, Schechter MA, Frey RH, Ward TT, et al. (1984) Detection of aminoglycoside ototoxicity by high-frequency auditory evaluation: selected case studies. Am J Otolaryngol 5: 177-182.
- Huizing EG, deGroot JC (1987) Human cochlear pathology in aminoglycoside ototoxicity: a review. Acta Otolaryngl Suppl 436: 117.
- Petersen L, Rogers C (2015) Aminoglycoside-induced hearing deficits–a review of cochlear ototoxicity. SAf Fam Pract 57: 77-82.
- World Health Organisation / Regional Office for Europe (2001) Health and nutritional status of the elderly in the Former Yugoslav Republic of Macedonia: Results of a national household survey. Geneva, Switzerland.
- Campbell KC, Meech RP, Klemens JJ, Gerberi MT, Dyrstad SS, et al. (2007) Prevention of noise-and drug-induced hearing loss with D-methionine. Hearing research 226: 92-103.
- Duggal P, Sarkar M (2007) Audiologic monitoring of multi-drug resistant tuberculosis patients on aminoglycoside treatment with long term follow-up. BMC Ear, Nose and Throat Disorders 7: 5.
- World Health Organization (2013) Global Tuberculosis Report, Guidelines for management of drug resistant tuberculosis. Geneva, Switzerland.
- Harries AD, Dye C (2006) Tuberculosis. Ann Trop Med Parasitol100: 415.
- Javadi MR, Abtahi B, Gholami K, Moghadam BS, Tabarsi P (2011) The incidence of amikacin ototoxicity in multidrug-resistant tuberculosis patients. Iran J Pharm Res 10: 905-911.
- National Tuberculosis and Leprosy Control Programme, Annual Report 2008. Abuja: NTBLCP, Nigeria.
- Nigeria Federal Ministry of Health, Strategic Framework for Implementation of TB-HIV activities 2007-2009. Abuja: Federal Ministry of Health, 2007.
- Yone EW, Kengne AP, Kuaban C (2011) Incidence, time and determinants of tuberculosis treatment default in Yaounde, Cameroon: a retrospective hospital register-based cohort study. BMJ open 1: e000289.
- Yone EW, Kuaban C, Kengne AP (2012) HIV testing, HIV status and outcomes of treatment for tuberculosis in a major diagnosis and treatment centre in Yaounde, Cameroon: a retrospective cohort study. BMC infect Dis 12: 190.
- Schacter D, Gilbert D, Wegner D (2011) Sensation and Perception: In Charles Linsmeiser, Psychology. Worth Publishers, USA.
- Wang S, Bian Q, Liu Z, Feng Y, Lian N, et al. (1999) Capability of serum to convert streptomycin to cytotoxin in patients with aminoglycoside-induced hearing loss. Hear Res 137: 1-7.
- Olaosun AO, Adekunle AO, Gbadamosi MOA, Ogundiran O, Fada P, et al. (2016) Ototoxicity in drug-resistant tuberculosis patients - a case report emphasizing the importance of audio-vestibular monitoring during treatment. IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) 15: 69-74.
- World Health Organization (2013) WHO media centre. Up-dated February 2013.
- World Health Organization (2011) Global Tuberculosis Control: WHO Report 2011. Geneva, Switzerland.
- World Health Organization (2008) Molecular Line Probe Assays for the rapid screening of patients at risk of multidrug-resistant tuberculosis (MDR-TB). Policy Statement. Geneva, Switzerland.
- Bauman N (2003) When Your Ear Ring, Cope with your tinnitus.Center for Hearing Loss Help. Stewartson, USA.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi