Case Report, J Otol Rhinol Vol: 7 Issue: 4
Elective Sphenopalatine Artery Ligation for Recurrent Epistaxis
Symeonides P* and Mirza S
ENT Department, Royal Hallamshire Hospital, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, UK
*Corresponding Author : Panas Symeonides
ENT Department, Royal Hallamshire Hospital, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, UK
E-mail: p.symeonides@googlemail.com
Received: July 09, 2018 Accepted: July 24, 2018 Published: August 1, 2018
Citation: Symeonides P, Mirza S (2018) Elective sphenopalatine artery ligation for recurrent epistaxis. J Otol Rhinol 7:4. doi: 10.4172/2324-8785.1000353
Abstract
Introduction: Epistaxis is a very common presenting complaint. A small percentage of patients will require surgical intervention for severe epistaxis.
Methods: We describe our experience in 3 consecutive patients and how we perform endoscopic sphenopalatatine artery ligation (ESPAL), as an elective procedure for patients with multiple hospital admissions for epistaxis.
Results: All patients remain free of epistaxis up to date. Conclusions: Elective ESPAL is an effective treatment option for a carefully selected group of patients.
Keywords: Recurrent epistaxis; Surgical management of epistaxis; Endoscopic sphenopalatine artery ligation
Introduction
Epistaxis is a common presenting complaint to the emergency department and General Practice. It has been reported that 60% of the population will have at least one episode of epistaxis during their life [1]. Only 10% though will require hospitalisation and the majority will be managed with simple measures like chemical cautery or nasal packing. A small percentage of 1-2% will require surgical intervention for severe epistaxis [2].
Endoscopic sphenopalatine artery ligation (ESPAL) for acute epistaxis has been investigated extensively and it provides a low morbidity, cost-effective alternative to prolonged posterior nasal packing and inpatient stay, internal maxillary artery (IMA) ligation or arterial embolization [3]. It has been suggested that ESPAL should be the first line treatment for medically fit patients with intractable acute posterior epistaxis [4].
To our knowledge there are no studies describing the use of ESPAL as an elective procedure, reserved for those patients who have multiple admissions or hospital attendances. Severe recurrent epistaxis with no obvious bleeding source on anterior rhinoscopy and nasoendoscopy, raises the suspicion of posterior epistaxis relating to the sphenopalatatine artery (SPA). For these patients epistaxis can be very troublesome, interrupting their daily activities, work and social life.
We present our experience with elective ESPAL.
Case Reports
Case 1
A 59 years old male presented with a six-month history of recurrent left epistaxis, lasting up to an hour. His past medical history included treatment for bowel cancer and hypertension on regular Aspirin. In the past, he had repeated silver nitrate cautery to the left nasal septum which made no difference. Nasal examination in the ENT clinic showed no obvious bleeding point on anterior rhinoscopy or nasoendoscopy. A CT scan was performed as a precaution given his previous history of malignancy, but this was clear. The options were discussed with the patient who opted for an elective ESPAL. He has no further epistaxis for over a year since his operation.
Case 2
A medically fit 35 years old female presented with a five-year history of recurrent left epistaxis, occurring three times a week and lasting up to ten minutes. She had silver nitrate cautery to a possible bleeding source at the left Little’s area but continued to be symptomatic and represented to the ENT department. Repeated nasoendoscopy showed no obvious bleeding source or lesions. She was offered an elective ESPAL and remains free of epistaxis for over 2 years.
Case 3
A 78 years old male presented with a three-month history of recurrent right epistaxis, lasting up to ten minutes. Like the other two patients he had multiple nasal cautery in the past. He had a complicated medical history, including severe aortic stenosis and ischaemic heart disease and was on Aspirin amongst other medications. He was scheduled for aortic valve replacement and coronary artery bypass grafting, but his operation was cancelled twice because of pre-operative epistaxis. The opinion of interventional radiology was sought by the cardiac surgeons, which deemed the patient high risk for cerebrovascular complications with percutaneous arterial embolisation. The patient was then referred to ENT and underwent an elective ESPAL. He remained epistaxis free and had his cardiac surgery.
How we do it
We perform elective ESPAL under general anaesthesia with controlled hypotension intra-operatively and the patient in a supine, “head-up” position on the operating table.
The nasal cavity is prepared with 5mls of Moffett’s solution (100mg of cocaine and 1mg of adrenaline made up to 10mls in volume with Normal saline or Sodium bicarbonate). We use a MADgicTM laryngotracheal mucosal atomisation device for the uniform spread of the solution on the nasal mucosa. The remaining 5mls are applied on neuropatties and introduced into the nasal cavity and around the middle meatus after draping the patient. If further vasoconstriction is required during surgery, 1:10,000 adrenaline solution is used.
Zero degree and angled nasoendoscopes are used to examine the nasal cavity thoroughly for any underlying lesion or potential bleeding points with particular attention given to the floor and roof of the nasal cavity, posterior septum, lateral nasal wall and post nasal space.
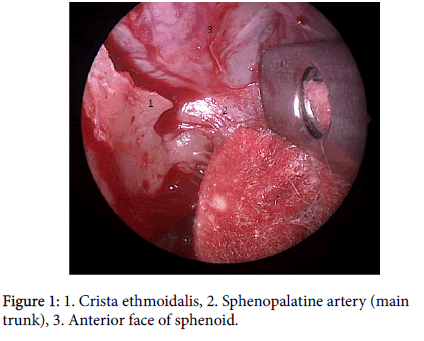
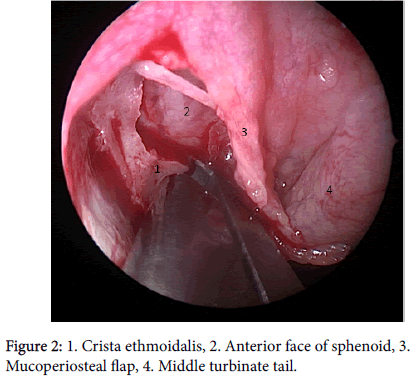
The procedure is performed with a 30° nasoendoscope, though a 0° nasoendoscope can be employed. The uncinate process, ethmoid bulla and attachment of the posterior tail of the middle turbinate in the middle meatal area are identified. Two to three neuropatties soaked in Moffett’s solution are applied to this area to further decongest the mucosa. A vertical incision of about 1cm is made onto the palatine bone posterior to the uncinate and natural maxillary ostium, anterior to the middle turbinate attachment, and inferior to the ethmoid bulla. An entry into the maxillary sinus is not usually performed but it may occur if the bone is thin. Creating an antrostomy or widening an accessory maxillary ostium can be useful for the inexperienced surgeon to increase the surgical field and allow identification of the posterior maxillary wall as a landmark for the SPA, which arises behind this. A mucoperiosteal flap is elevated posteriorly with a suction Freer’s elevator, keeping a broad field of dissection. The flap is then elevated more inferiorly in the direction of the Eustachian tube orifice for about 1 cm, before it is elevated superiorly. The crista ethmoidalis, a protuberance of bone may be identified and the SPA can usually be seen just posterior to this being ‘tented up’ (Figure 1). The crista ethmoidalis may be removed with a curette or with a 2 mm Kerrison punch (Figure 2). This exposes more of the main trunk of the SPA. Careful dissection aided by a ball probe allows exposure around the artery for effective cautery using a suction bipolar cautery forceps. The artery is then cut with scissors away from the foramen to avoid retraction of the proximal stump into the pterygopalatine fossa and persistent bleeding. The stump can be further cauterised after cutting.
We continue to raise our flap posterior-medially onto the anterior face of the sphenoid sinus and up to the nasal septum, cauterising and dividing any further branches of the SPA. Branches may also arise inferior to the main trunk of the SPA, just posterior to the inferior turbinate. Once all the branches are divided we replace the flap. NasoporeR absorbable nasal pack is placed in the nasal cavity if required.
Elective patients are usually discharged the same day with SterimarR nasal douching.
Discussion
Posterior epistaxis accounts for only a small percentage of all the patients presenting with epistaxis but tends to respond variably to conservative measures [5]. It still poses a clinical dilemma to the ENT surgeon as to the management and timing of any surgery. Traditionally, surgery was reserved for patients who failed nasal packing and involved the ligation of the internal maxillary artery via Caldwell-Luc approach, with considerable failure and complication rates. In 1992, Budrovich et al., [6] described the endoscopic ligation of the terminal branch of the IMA, the sphenopalatatine artery. Achieving control of the artery proximal to the nasal cavity reduces the risk of forming a collateral blood supply and failure rates [2,7].
ESPAL has gained popularity over the years for the acute management of severe epistaxis due to its low morbidity and costeffectiveness when compared with percutaneous arterial embolisation. Generally, in our institution, percutaneous arterial embolisation is performed under a general anaesthetic and therefore reserved for patients who failed surgical intervention.
The failure of ESPAL is mainly due to the inability to identify all the branches of the SPA, the slipping of surgical clips when used and missed bleeding from the ethmoidal arteries [8]. The variation in the anatomy and position of the sphenopalatine foramen and its accessory foramina and the extensive branching of the SPA [9] (sometimes more than four branches), can provide a challenge intra-operatively. Less frequently, persistent bleeding occurs from anastomotic branches of the pharyngeal artery distal to the point of ligation near the sphenopalatine foramen. We therefore advocate extending the dissection of the mucoperiosteal flap over the anterior face of the sphenoid sinus and continue medially cauterising all the branches with bipolar diathermy before diving them. We do not use surgical clips in our ESPAL.
As in our cases, a small cohort of patients with posterior epistaxis will respond only temporarily to conservative measures. These patients will present to the ENT department and often have multiple nasal cautery to suspected anterior bleeding points or nasal packing and inpatient admissions. This may initiate a vicious circle of repeated mucosal trauma and epistaxis with increased risk for the development of adhesions and septal perforations amongst other complications [10]. Furthermore, frequent admissions and hospital appointments have a financial impact both for the patient and the health system. According to figures taken from NHS tariffs 2015 – 2016, the cost of one hospital admission for epistaxis can vary from £692 to £1820 depending on comorbidities whilst an elective ESPAL costs between £1497 and £1690, making the latter a cost-effective option for an appropriately selected group of patients.
Conclusion
The impact of recurrent hospital attendances was evident in all of our cases. It is well recognised that patients with chronic conditions adjust their aspirations, lifestyle, and employment leading to increased levels of frustration and eventually anxiety and depression [11].
In patients with recurrent posterior epistaxis, elective ESPAL is an effective treatment.
References
- Viehwag TL, Robertson JB, Hudson JW. Epistaxis: diagnosis and treatment (2006) J Oral Maxillofac Surg 64: 511-518.
- Ram B, White PS, Saleh HA, Odutoye T, Cain A (2000) Endoscopic endonasal ligation of the sphenopalatine artery. Rhinology 38: 147-149.
- Rudmik L, Smith TL (2012) Management of intractable spontaneous epistaxis. Am J Rhinol Allergy 26: 55-60.
- Dedhia RC, Desai SS, Smith KJ, Lee S, Schaitkin BM, et al. (2013) Cost-effectiveness of endoscopic sphenopalatine artery ligation versus nasal packing as first-line treatment for posterior epistaxis. Int Forum Allergy Rhinol 3: 563-566.
- Villwock JA, Jones K (2013) Recent Trends in Epistaxis Management in the United States. JAMA Otolaryngol Head Neck Surg 139: 1279-1284.
- Budrovich R, Saetti R (1992) Microscopic and endoscopic ligature of the sphenopalatine artery. Laryngoscope 102: 1391-1394
- Thkar A, Sharan CJ (2005) Endoscopic sphenopalatine artery ligation for refractory posterior epistaxis. Iran J Otorhinolaryngol 57: 215-218.
- McDermott AM, O’Cathain E, Carey BW, O’Sullivan P, Sheahan P (2015) Sphenopalatine Artery Ligation for Epistaxis: Factors Influencing Outcome and Impact of Timing of surgery. Otolaryngology-Head and Neck Surgery 154: 547-552.
- Rezende GL, Soares RVY, Moraes WG, Pires de Oliveira CAC, Nakanish M (2012) The sphenopalatine artery: a surgical challenge in epistaxis. Braz J Otorhinolaryngol 78: 42-47.
- Gandomi B, Arzaghi MH, Khademi B, Rafatbakhsh M (2013) Endoscopic Cauterization of the Sphenopalatine Artery to Control Severe and Recurrent Posterior Epistaxis. Iran J Otorhinolaryngol 25: 147-154.
- Turner J, Kelly B (2000) Emotional dimensions of chronic disease. West J Med 172: 124-128.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi