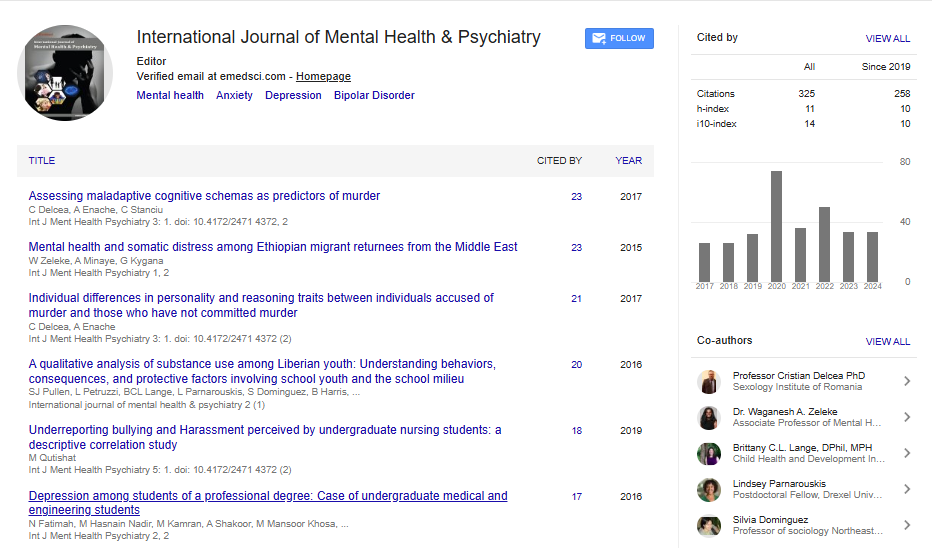
Review Article, Int J Ment Health Psychiatry Vol: 11 Issue: 1
Etiopathogenesis and Management Updates on the Comorbidity Depression-Diabetes: A Review of Literature
Roland Muyisa Muhindo*
Department of Medicine, Catholic University of the Graben, Democratic Republic of the Congo
*Corresponding Author:Roland Muyisa Muhindo*
Department of Medicine, Catholic University of the Graben, Democratic Republic of the Congo
E-mail: rolandmuyisam@gmail.com
Received date: 08 November, 2023, Manuscript No. IJMHP-23-119676;
Editor assigned date: 10 November, 2023, PreQC No. IJMHP-23-119676 (PQ);
Reviewed date: 24 November, 2023, QC No. IJMHP-23-119676;
Revised date: 16 January, 2025, Manuscript No. IJMHP-23-119676 (R);
Published date: 23 January, 2025, DOI: 10.4172/2471-4372.1000284
Citation: Muhindo RM (2025) Etiopathogenesis and Management Updates on the Comorbidity Depression-Diabetes: A Review of Literature. Int J Ment Health Psychiatry 11:1.
Keywords: Depression; Diabetes; Comorbidity; Anti-diabetic
Introduction
Depression and diabetes comorbidity is a pressing public health concern. Studies have consistently shown that depression is highly prevalent among patients with diabetes and that it is linked to increased morbidity and mortality [1-10]. Furthermore, research has established a reciprocal relationship between diabetes and depression [11]. The purpose of this review is to provide an overview of the comorbidity between depression and diabetes. Specifically, we will discuss the epidemiology, etiopathogenic mechanisms, and management strategies of this comorbidity.
Literature Review
Our review thoroughly searched for the keyword 'depression in patients with diabetes' from 2015 to 2023. We selected articles that covered the prevalence of comorbid depression and diabetes (22 articles), the etiopathogenesis of this comorbidity (8 articles), and the effective management of this condition (26 articles).
Description of the diseases
Depression: Depression is a mental health condition that presents as distinct episodes lasting a minimum of two weeks. While some episodes may last a considerable period, most are longer. Mood changes characterize these episodes, thought patterns, neuro vegetative functions, and remissions between episodes. In most cases, depression is recurrent, but a diagnosis based on a single episode is still possible. This is what is known as the classic condition of depressive disorder or major depressive disorder. As defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM5), depressive disorders include disruptive disorder with emotional dysregulation, major depressive disorder (including the major depressive episode), persistent depressive disorder (dysthymia), premenstrual dysphoric disorder, substance/drug-induced depressive disorder, depressive disorder due to a medical condition, other specified depressive disorder, and unspecified depressive disorder. These disorders are all characterized by a sad, empty, or irritable mood, accompanied by physical and cognitive changes that interfere with an individual's functioning abilities. They only differ in their duration, chronology, and assumed etiologies. This review, however, is solely focused on major depressive disorder.
Diabetes: Diabetes mellitus is a multifaceted metabolic disorder that results in chronic hyperglycemia. This occurs as a result of insufficient insulin secretion (in type 1 diabetes) and/or diminished tissue responsiveness to insulin (in type 2 diabetes). This deficient insulin action on tissues leads to disruptions in the processing of carbohydrates, lipids, and proteins.
Epidemiology
Prevalence and predictive factors: Studies conducted in various countries have reported a high prevalence of depression in patients with diabetes, with a range of associated factors. In the United States, a study found a prevalence of 19.3% in patients with type 2 diabetes, with advanced age, high HbA1c values, and the prescription of an oral antidiabetic among the associated factors [12]. In Germany, a prevalence of 30.04% of depression symptoms was observed in young patients with type 1 diabetes, and a long duration of diabetes was found to be associated with the persistence of depression symptoms in adults [13]. In Australia, prevalence rates of 8% and 11% were reported for patients with type 1 and type 2 diabetes, respectively [14]. Asian countries have also reported a high prevalence of depression in patients with diabetes, with rates varying between 11.6% and 67.5% [15]. Low income, sedentary lifestyle, and insufficient self-care are among the factors precipitating the occurrence of depression in patients with diabetes [16-1818]. In South America and Africa, prevalence rates of 35.56% and 40%, respectively, have been reported [19,20]. Poverty, depression, and diabetes have been identified as a "syndemic of non-communicable diseases" in low-income populations [21,22].
Comorbidity depression–diabetes and morbidity-mortality: Research has consistently shown that the coexistence of depression and diabetes is significantly linked to heightened morbidity and mortality rates. Farooqi A has reported that the presence of both conditions increases the likelihood of cardiovascular mortality by 47.9%, coronary artery disease by 36.8%, and stroke by 32.9% [23]. In Lithuania, this comorbidity is strongly associated with a high incidence of diabetic nephropathy and retinopathy, while in Finland it is linked to cardiovascular diseases [24]. Additionally, a study conducted in Tunisia found that 26% of patients with diabetes experienced depression, and that there is a strong correlation between depression-diabetes comorbidity and erectile dysfunction [25].
Etiopathogenic mechanisms in the depression–diabetes comorbidity
Underlying factors in the link between depression and diabetes various factors have been proposed to explain the co-occurrence of these conditions. One of the most studied mechanisms is the involvement of oxidative stress and chronic inflammation, which are common features of both depression and diabetes [26,27]. In depression, the dysregulation of the hypothalamic-pituitary axis by chronic stress, resulting in high levels of cortisol, is often implicated. Another factor that has been linked to chronic stress and depression is the amyloid beta protein, which can trigger neuro-inflammatory processes and reduce serotonin levels. These changes may also contribute to the development of Alzheimer's disease, sometimes referred to as "type 3 diabetes" (Figure 1). However, the specific mechanisms that lead to each of these conditions are not always the same [28]. Some studies have suggested that low levels of GDNF (Glial cell Derived Neurotrophic Factor) may play a role in the comorbidity of depression and diabetes. Recent research has also identified genetic factors that may contribute to both depression and diabetes. For example, Kroemer NB and Kaufmann T have found metabolic traces of the genetic risk of diabetes in the human brain, which may be associated with depression as well.
Figure 1: Schematic representation of the main common biological substrates linking increased Amyloid Beta (Aβ) levels to the development of Alzheimer's disease, depression and diabetes. Chronic stress can increase Aβ through different mechanisms. It has been proposed that alterations in APP processing and dysregulation of Aβ production and clearance can occur after increased release of stress hormones. Furthermore, reduction in serotonergic tone, neuroinflammatory pathway activation as well as microglial activation, reduction in neurotrophin levels have also been implicated. This increase in soluble forms of Aβ levels represents an early phenomenon that can ultimately lead to the development of Alzheimer's disease, depression and diabetes.
Discussion
Effective management strategies for depression in patients with diabetes
Need for systematic screening for depression in patients with diabetes: Systematic screening for depression in patients with diabetes remains the greatest way to avoid the complications of the depression–diabetes comorbidity. This screening must take into account the factors involved in the occurrence of complications. Factors associated with non-adherence to anti-diabetic treatment in depression-diabetes comorbidities: Young age, addiction to the initial anti-diabetic, socioeconomic status, visits to different doctors, and the low number of complications.
An Indian study has demonstrated the feasibility of setting up, with limited resources, regular screening for depression in patients with diabetes.
Drug use in the comorbidity depression–diabetes: After a decrease in adherence to treatment due to the occurrence of a depressive episode in patients with diabetes, a slight improvement in adherence to anti-diabetic treatment is possible in patients with diabetes and depression by the administration of antidepressants. Certain antidepressants such as sertraline are reported with some effectiveness in recently diagnosed depression in patients with type 2 diabetes. However, this still needs to be confirmed by further analytical studies.
Also, new drug development opportunities are envisaged such as the association of classic antidepressants with antidiabetics. Such is the case of the development of drugs that activate NRF2 (Nuclear factor erythroid 2-Related Factor 2), a regulator of the oxidative response; or the exploitation of the BDNF pathway (Brain-Derived Neurotrophic Factor) by inhibitors of the renin-angiotensin aldosterone system recently proposed by Balogh D, et al. In addition, Cooper DH and his collaborators analyzed the possibility of using GLP-1 receptor agonists (Glucagon-Like Peptide-1), an incretin secreted by enteroendocrine cells, initially indicated for its action on type 2 diabetes and recently its possible antidepressant properties: Promising results have been found with molecules such as dulaglutide in reducing the occurrence of depression in patients with diabetes.
Several questions about the molecules used in the depression diabetes comorbidity remain unresolved. A non-drug intervention should be preferred to the drug treatment of depression in patients with diabetes. Studies have shown that antidepressant treatments do not improve adherence to anti-diabetic treatment or that they would increase the occurrence of complications as demonstrated by a systematic analysis by Charlotte RL, et al.
Non–medicinal means in the management of depression in patients with diabetes: Regular psychiatric interventions would reduce the prevalence of depression–diabetes comorbidity and thus improve the quality of life of diabetic patients. Cognitive-behavioral interventions and physical exercises primarily reduce the occurrence of insulin resistance and are associated with an improvement in tissue sensitivity to insulin, good cardio-respiratory fitness, and a reduction in depression symptoms. Models of cognitive-behavioral management applications are in development and have demonstrated their effectiveness in the diagnosis and management of depression in patients with diabetes although some studies demonstrate limitations of psychological interventions.
Altogether, collaborative models in the management of depression in patients with diabetes are to be preferred. Thus, Groot Mary proposed the following strategies: Systematic screening for depression symptoms in patients with diabetes, securing access to behavioral therapy, good collaboration between caregivers and patients with diabetes to support self–management of diabetes, and monitoring the use and effectiveness of antidepressants.
Conclusion
The comorbidity depression-diabetes is a common public health problem. There is a necessity for systematic screening of depression in patients with diabetes. The management of depression in patients with diabetes includes medicinal and non-medicinal measures.
Conflict of Statement and Interest
There was no conflict of interest involved in this review.
Funding
No funding.
References
- Battaglia F, Cannavo D, Battaglia E, Fazio E, Minutolo G, et al. (2015) the comorbidity of depression and diabetes mellitus type 2: An observational study. Eur Psychiatry 30: 1320.
- Boehmer K, Lakkad M, Johnson C, Painter JT (2023) Primary care diabetes depression and diabetes distress in patients with diabetes. Prim Care Diabetes 17: 105–108.
[Crossref] [Google Scholar] [PubMed]
- Deschenes SS, Burns RJ, Schmitz N (2015) Associations between diabetes , major depressive disorder and generalized anxiety disorder comorbidity, and disability: Findings from the 2012 Canadian Community Health Survey—Mental Health (CCHS-MH). J Psychosom Res 78: 137–142.
[Crossref] [Google Scholar] [PubMed]
- Hsieh HM, Lin CH, Weng SF, Lin PC, Liu TL, et al. (2023) Health-related quality of life, medical resource use and physical function in patients with diabetes mellitus and depression: A cross-sectional analysis from the national health and nutrition examination survey. J Affect Disord 327: 93–100.
[Crossref] [Google Scholar] [PubMed]
- Huang W, Wang Z, Zou C, Liu Y, Pan Y, et al. (2023) Effects of metabolic factors in mediating the relationship between type 2 diabetes and depression in East Asian populations: A two-step, two-sample Mendelian randomization study. J Affec Disord 335: 120–128.
[Crossref] [Google Scholar] [PubMed]
- Lunghi C, Zongo A, Tardif I, Demers E, Diendere JDR, et al. (2021) Depression but not non-persistence to antidiabetic drugs is associated with mortality in type 2 diabetes: A nested case-control study. Diabetes Res Clin Pract 171.
[Crossref] [Google Scholar] [PubMed]
- Saifuddin M, Selim S, Uddin M, Mahbub M, Hasan ABM, et al. (2017) To study the prevalence of comorbid depression among patients with type 2 diabetes mellitus in Bangladesh. Endocr Pract 23: 63.
- Sodhi B, Malik M, Agarwal P, Basu S (2023) The prevalence and predictors of depression and disability in older adults and elderly patients with diabetes in India: Cross-sectional analysis from the longitudinal study on ageing. Diabetes Metab Syndr 17: 102765.
[Crossref] [Google Scholar] [PubMed]
- Takeshima T, Nakamura Y, Iwasaki K, Hiroi S, Uda A, et al. (2016) Comorbidity of depression and type 2 diabetes: A retrospective Japanese claims database analysis. Value in Health 19: A665.
- Vyas A, Patel K, Agha K, Sasidharan N, Sultan W, et al. (2021) Rising burden of cardiovascular disease risk factors and acute cardiac events in young adults with comorbid depression: A comparison of two nationwide US cohorts hospitalized 10-years apart. Circulation 144: 101755.
- Diderichsen F, Andersen I (2019) The syndemics of diabetes and depression in Brazil–An epidemiological analysis. SSM Popul Health 7: 100318.
[Crossref] [Google Scholar] [PubMed]
- Monaghan M, Mara CA, Kichler JC, Westen SC, Rawlinson A, et al. (2021) Multisite examination of depression screening scores and correlates among adolescents and young adults with type 2 diabetes. Can J Diabetes 45: 411–416.
[Crossref] [Google Scholar] [PubMed]
- Baechle C, Stahl-Pehe A, Castillo K, Lange K, Holl RW, et al. (2022) Course of screening-based depression in young adults with a long type 1 diabetes duration: Prevalence and transition probabilities–A cohort study. Diabetes Res Clin Pract 185.
[Crossref] [Google Scholar] [PubMed]
- Nefs G, Hendrieckx C, Reddy P, Browne JL, Bot M, et al. (2019) Comorbid elevated symptoms of anxiety and depression in adults with type 1 or type 2 diabetes: Results from the International Diabetes MILES Study. J Diabetes and Complications 33: 523–529.
[Crossref] [Google Scholar] [PubMed]
- Kalra G, Gill S, Tang TS (2020) Depression and diabetes distress in South Asian adults living in low and middle-income countries: A scoping review. Can J Diabetes 44: 521-529.
[Crossref] [Google Scholar] [PubMed]
- Majumdar S, Sinha B, Dastidar BG, Gangopadhyay KK, Ghoshal S, et al. (2021) Assessing prevalence and predictors of depression in type 2 Diabetes Mellitus (DM) patients–The DEPDIAB study. Diabetes Res Clin Pract 178: 108980.
[Crossref] [Google Scholar] [PubMed]
- Naskar S, Victor R, Nath K (2017) Depression in diabetes mellitus—A comprehensive systematic review of literature from an Indian perspective. Asian J Psychiatr 27: 85–100.
[Crossref] [Google Scholar] [PubMed]
- Patra S, Patro BK, Mangaraj M, Sahoo SS (2020) Screening for depression in diabetes in an Indian primary care setting: Is depression related to perceived quality of life? Prim Care Diabetes 14: 709–713.
[Crossref] [Google Scholar] [PubMed]
- Ogunsakin RE, Olugbara OO, Moyo S, Israel C (2021). Meta-analysis of studies on depression prevalence among diabetes mellitus patients in Africa. Heliyon 7: e07085.
[Crossref] [Google Scholar] [PubMed]
- Valladares-Garrido MJ, Soriano-Moreno AN, Rodrigo-Gallardo PK, Moncada-Mapelli E, Pacheco-Mendoza J, et al. (2020) Depression among Peruvian adults with hypertension and diabetes: Analysis of a national survey. Diabetes Metab Syndr 14: 141–146.
[Crossref] [Google Scholar] [PubMed]
- Diderichsen F, Andersen I, Mathisen J (2021) Depression and diabetes: The role of syndemics in the social inequality of disability. J Affect Disord Rep 6: 100211.
[Crossref]
- Mendenhall E, Kohrt BA, Norris SA, Ndetei D, Prabhakaran D (2017) Non-communicable disease syndemics: Poverty, depression, and diabetes among low-income populations. Lancet 389: 951-963.
[Crossref] [Google Scholar] [PubMed]
- Farooqi A, Khunti K, Abner S, Gillies C, Morriss R, et al. (2019) Comorbid depression and risk of cardiac events and cardiac mortality in people with diabetes: A systematic review and meta-analysis. Diabetes Res Clin Pract 156: 107816.
[Crossref] [Google Scholar] [PubMed]
- Ahola AJ, Radzeviciene L, Zaharenko L, Bulum T, Skrebinska S, et al. (2020) Association between symptoms of depression, diabetes complications and vascular risk factors in four European cohorts of individuals with type 1 diabetes–InterDiane Consortium. Diabetes Res Clin Pract 170: 108495.
[Crossref] [Google Scholar] [PubMed]
- Huang Y, Su Y, Chen H, Liu H, Hu J (2021) Serum levels of CRP are associated with depression in a middle-aged and elderly population with diabetes mellitus: A diabetes mellitus-stratified analysis in a population-based study. J Affect Disord 281: 351–357.
[Crossref] [Google Scholar] [PubMed]
- Morgese MG, Schiavone S, Trabace L (2017) Emerging role of amyloid beta in stress response: Implication for depression and diabetes. Eur J Pharmacol 817: 22–29.
[Crossref] [Google Scholar] [PubMed]
- Yang Y, Xie B, Ju C, Jin H, Ye X, et al. (2019) The association of decreased serum GDNF level with hyperglycemia and depression in type 2 diabetes mellitus. Endocr Pract 25: 951–965.
[Crossref] [Google Scholar] [PubMed]
- Barengolts E (2019) Double dipper: Comorbid depression and diabetes, from a biomarker to treatment. Should endocrinologists be educated to be at the forefront of depression treatment. Endocr Pract 25: 968-970.
[Crossref] [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi