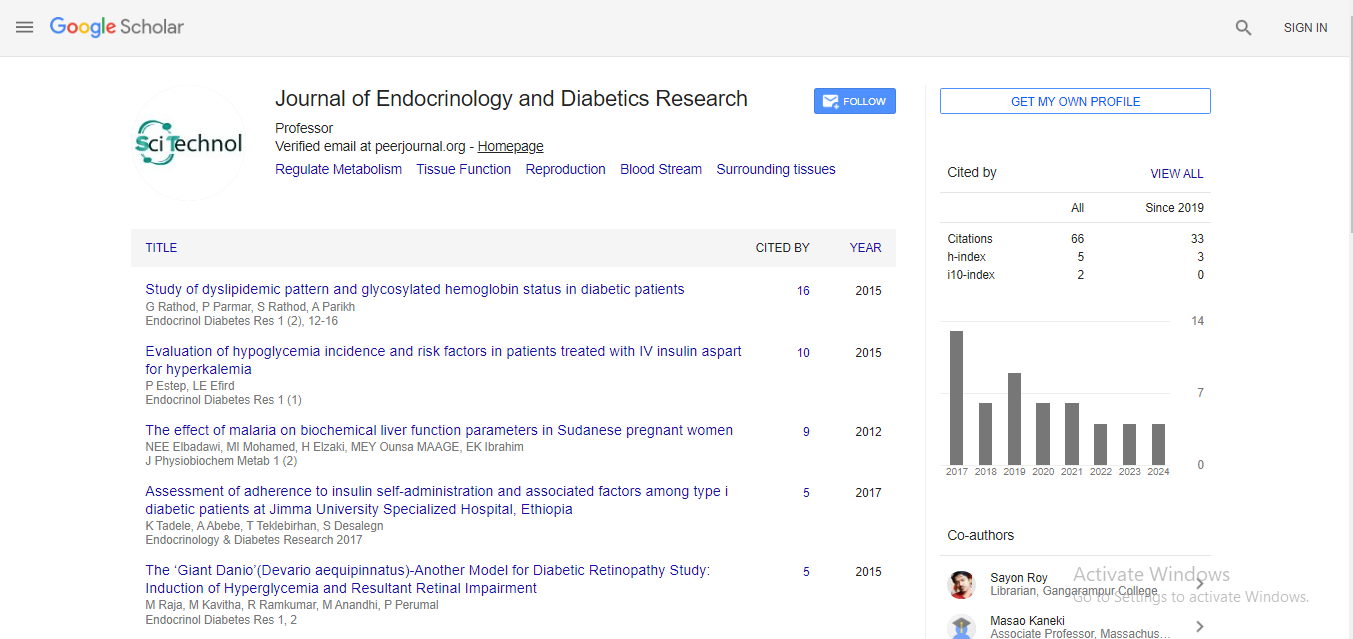
Case Report, Endocrinol Diabetes Res Vol: 7 Issue: 2
Euglycemic Diabetic Ketoacidosis in a Patient with SARS-COV-2 Infection, a Stress Induced Complication or a Coronavirus Related Complication?
Sempastian Filippas-Ntekouan 1*, Angelos Liontos2 , Fotios Barkas2 , Theodora Maniatopoulou2 , Revekka Konstantopoulou2 , Theodora Dimitriou2 , Georgia Manthou2and Haralampos Milionis21 Department of Internal Medicine, University Hospital of Ioannina, Ioannina, Greece
2 Department of Infectious Diseases, University Hospital of Ioannina, Ioannina, Greece
*Corresponding Author : Sempastian Filippas-Ntekouan
Department of Internal Medicine, University Hospital of Ioannina, Ioannina, Stavrou Niarchou Av, Greece, 45 500
Tel: 0030 6979743692;
Email: sebastienfilippas@gmail.com
Received Date:January 30, 2020; Accepted Date:February 17, 2021; Published Date:February 22, 2021
Citation:Filippas-Ntekouan S, Liontos A, Barkas F, Maniatopoulou T, Konstantopoulou R, et al. (2021) Euglycemic Diabetic Ketoacidosis in a Patient with SARS-COV-2 Infection, a Stress Induced Complication or a Coronavirus Related Complication? Endocrinol Diabetes Res 7:2.
Abstract
Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infections have affected millions of persons around the globe since first described in December 2019. Coronavirus Disease (COVID-19) is primarily a respiratory tract infection and in severe cases may lead to pneumonia, acute respiratory distress syndrome and death. Diabetes mellitus comprises a serious comorbidity that has been associated with increased risk of adverse outcomes. In these patients, COVID-19 has been associated with increased risk of ketosis and ketoacidosis which is a life-threatening complication. Herein, we describe a case of a SARS-CoV-2 positive patient presenting with symptomatic euglycemic ketoacidosis soon after the initiation of a Sodium-Glucose Co-Transporter-2 (SGLT-2) inhibitor. Clinicians should be alert for diabetic ketoacidosis as a consequence of COVID-19 in the context of diabetes since early diagnosis and treatment may favorably affect outcome.
Keywords: COVID-19; SARS-COV-2; Ketoacidosis; Diabetes mellitus; Sodium-Glucose Co-Transporter-2 (SGLT-2) inhibitor
Introduction
Severe Acute Respiratory Syndrome Coronavirus 2 (SARSCoV-2) infections has transformed into pandemic after the first case of Coronavirus Disease (COVID-19) was identified in December 2019 in Wuhan [1]. COVID-19 poses a high risk of mortality and morbidity in specific groups of people, including those older than 65 years or people with underlying medical conditions like heart disease, lung disease, diabetes, and chronic kidney disease [2]. Diabetes comprises a serious comorbidity that increases the risk of adverse outcomes in patients with COVID-19. In these patients, clinicians should be alerted to identify and appropriate treat hyperglycemic complications, including Diabetic Ketoacidosis (DKA) and hyperosmolar status. DKA is characterized by elevated blood glucose levels greater than 250 mg/dl, arterial pH<7.30, and increased serum ketone levels (i.e. >3 mmol/L) [3]. On the other hand euglycemic ketoacidosis presents with near normal glucose levels (i.e. <250 mg/dl) and is considered a rare, but severe adverse event of Sodium-Glucose Co Transporter 2 (SGLT-2) inhibitors [4]. Herein, we report a case of SGLT-2 associated euglycemic ketoacidosis precipitated by SARS-COV-2 infection.
Case Report
An 83-year-old was transferred to the emergency department of our hospital due to a decline in the level of consciousness, drowsiness and reduced food and fluid intake. His medical history included a long-standing type 2 diabetes mellitus (>20 years), benign prostate hyperplasia, arterial hypertension, and new onset dementia. His medications included simvastatin 40 mg, valsartan 160 mg, amlodipine 5 mg, donepezil, metformin 1 gr bid, vildagliptin 100 mg qd, gliclazide 30 mg qd. Several days prior to admission, empagliflozin 25 mg qd was added to his medications. Upon admission, vital signs were as follows: blood pressure 137/70 mmHg, 78 beats per minute, SpO2 90%, Temperature 36.2°C. Physical examination was unremarkable except for difficulty in naming his close relatives. An arterial blood gas analysis revealed metabolic acidosis with increased anion gap serum ketone levels were 5.7 mmol/L (Table 1); blood glucose was 180 mg/dL (10 mmol/L). Euglycemic DKA associated with an SGLT-2 inhibitor was a provisional diagnosis and treatment was started accordingly. Despite the absence of contact history, a RT-PCR for SARS-COV-2 was obtained which was positive, while a chest x-ray showed evidence of bilateral pulmonary infiltrates. He was transferred to the Infectious Diseases Unit and treatment protocols for COVID-19 and ketoacidosis were instituted. Of note, insulin autoantibodies were positive. The patient remained stable, without any need for supplemental oxygen. Mental status improved; acidosis gradually resolved. The patient was discharged home on day 15 of hospitalization.
| Day 1 | Day 2 | Day 3 | Day 4 | Day 8 | Day 12 | Day 15 | |
|---|---|---|---|---|---|---|---|
| pH | 7.09 | 7.39 | 7.37 | 7.34 | 7.41 | 7.42 | 7.43 |
| pCO2 mmHg | 13 | 23 | 28 | 26 | 18 | 22 | 30 |
| HCO3 (mmol/L) | 8 | 17 | 18 | 17 | 16 | 18 | 21 |
| pO2 mmHg | 83 | 68 | 74 | 96 | 107 | 71 | 80 |
| Lactate (mmol/L) | 2.1 | 1.4 | 1.6 | 1.2 | 0.9 | 0.9 | 1.3 |
| AG | 23 | 7 | 7 | 9 | 9 | 9 | 10 |
| Ketones (mmol/L) | 5.9 | 1.2 | 0.6 | ||||
| WBC (/mm3) | 15.730 | 10850 | 9410 | 7720 | 10360 | 11020 | 7480 |
| Lymphocytes | 1573 | 1160 | 1590 | 1500 | 1700 | 1740 | 1800 |
| Urea (mg/dL) | 80 | 78 | 63 | 38 | 10 | 27 | 28 |
| Creatinine (mg/dL) | 1.07 | 0.91 | 0.79 | 0.62 | 0.59 | 0.65 | 0.52 |
| CRP (mg/dL) | 99 | 67 | 57 | 28 | 24 | 11 | 11 |
| Feritin (mg/dL) | 307 | 519 | 295 | ||||
| LDH (IU/dL) | 266 | 317 | 618 | 313 | 355 | 292 | 211 |
Table 1. Laboratory data during patient’s hospitalization.
Discussion
Diabetic ketoacidosis is a recognized and extremely rare complication of treatment with SGLT-2 inhibitors [5]. Common precipitating factors of SGLT2-associated DKA include fasting, dietary modifications, inter current illnesses (such as serious infections, pancreatitis, cerebrovascular accidents, acute coronary events), surgical stress, insulin insufficiency, inappropriate reduction of insulin dosing and inappropriate management of SGLT2 in the ‘periprocedural period’ (e.g. colonoscopy). It may present with elevated, normal or near-normal glucose levels, a condition called euglycemic DKA [6]. To our knowledge, this is the first reported case of empagliflozin-associated euglycemic DKA precipitated by SARSCOV-2 infection with positive anti-insulin autoantibodies. COVID-19 is notoriously known for its serious pulmonary manifestations including pneumonia and Acute Respiratory Distress Syndrome (ARDS) which are the main causes of morbidity and mortality in COVID-19 patients. Beside the lung predilection of SARS-COV-2, several extra pulmonary manifestations have been recognized. DKA has been described in patients with COVID-19 in various settings (Table 2). These include case reports denoting new onset DKA in patients with type 2 diabetes [7,8], absence of autoantibodies in insulin dependent diabetes [9] and increased mortality nearing 50% [10]. Of note, euglycemic ketoacidosis has been reported in a COVID-19 patient with gestational diabetes [11]. Euglycemic ketoacidosis in patients receiving SGLT-2 has also been recently described in various clinical settings [12-15]. Finally, DKA has been reported in a patient with acute pancreatitis due to SARS-COV-2 [16] and in a child with multisystem inflammatory syndrome precipitated by SARS-COV-2 infection [17]. Although not fully elucidated, the proposed underlying mechanisms of COVID-19-induced ketosis and ketoacidosis involve (Figure 1):
| Author | Type of study | Number of patients | Type of diabetes | SGLT-2 inhibitor use | Outcome | Reference |
|---|---|---|---|---|---|---|
| Croft et al | Case series | 5 | Type 2 | no | 1 deceased | [7] |
| Li et al | Retrospective cohort | 658 | Type 1 and type 2 and non-DM | - | 9/42 ketosis patients deceased | [8] |
| Hollstein et al | Case report | 1 | No | no | Discharged | [9] |
| Pal et al | Systematic review | 110 | Type 2 (77%), new-onset((10%) | 7/110 | 45% deceased | [10] |
| Smati et al | Case report | 1 | Gestational | no | Discharged | [11] |
| Batista et al | Case report | 1 | type 2 DM | yes | Discharged | [12] |
| Palermo et al | Case series | 2 | Type 2 (one) and new-onset(one) | yes (1) | Discharged | [13] |
| Oriot et al | Case report | 1 | Type 1 | yes | Discharged | [14] |
| Fang et al | Case report | 1 | Type2 | yes | Discharged | [15] |
| Tollard et al | Case report | 1 | New-onset diabetes along with acute pancreatitis | no | Deceased | [16] |
| Naguib et al | Case report | 1 | New-onset diabetes(8years of age) | no | Discharged | [17] |
Table 2. Studies in patients with COVID-19 and DKA
1. Production of stress hormones is intensified during COVID-19 due to cytokine storm’’ leading to increased peripheral lipolysis, a raised glucagon to insulin ratio and thus hepatic ketone production,
SARS-COV-2 enters human cells by spiked glycoprotein binding to the Angiotensin Converting Enzyme (ACE)-2 receptors on human cell membranes, in the lungs as well as in a number of extra pulmonary tissues, including pancreatic beta cells [18,19]. The latter has been proposed to cause cell injury and death, and consequently reduced function of beta cells on the islets of Langerhans. These factors may account for the development of ketoacidosis in patients with type 2 diabetes and the development of new onset diabetes mellitus in previously healthy persons.
Immune dysregulation and production of insulin dependent diabetes related autoantibodies could also play a role in the development of both new onset diabetes and diabetic ketoacidosis in patients with COVID-19. This could be the case in our patient who tested positive for anti-insulin autoantibodies.
All in all, COVID-19 has been associated with numerous extra pulmonary manifestations, including new onset diabetes as well as DKA in otherwise previously healthy or stable patients with type 2 diabetes. The presence of high anion gap metabolic acidosis in COVID-19 patients with diabetes mellitus type 1 or type 2 should alert physicians to emergency treatment. Prior treatment with a SGLT-2 inhibitor could be a precipitating factor of euglycemic DKA and should be discontinued.
References
- Zheng, Z., et al., Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J Infect, 2020. 81(2): p. e16-e25.
- Jordan, R.E., P. Adab, and K.K. Cheng, Covid-19: risk factors for severe disease and death. Bmj, 2020. 368: p. m1198.
- Wei, Y., et al., Clinical characteristics and outcomes of patients with diabetic ketoacidosis of different severity. Medicine (Baltimore), 2020. 99(45): p. e22838.
- Musso, G., et al., Diabetic ketoacidosis with SGLT2 inhibitors. Bmj, 2020. 371: p. m4147.
- Meyer, E.J. and G. Gabb, SGLT2 Inhibitor-Associated Euglycemic Diabetic Ketoacidosis: A South Australian Clinical Case Series and Australian Spontaneous Adverse Event Notifications. 2018. 41(4): p. e47-e49.
- Meyer, E.J., et al., Periprocedural Euglycemic Diabetic Ketoacidosis Associated With Sodium-Glucose Cotransporter 2 Inhibitor Therapy During Colonoscopy. Diabetes Care, 2020.
- Croft, A., et al., First-time Diabetic Ketoacidosis in Type 2 Diabetics With Covid-19 Infection: A Novel Case Series. J Emerg Med, 2020.
- Li, J., et al., COVID-19 infection may cause ketosis and ketoacidosis. 2020.
- Hollstein, T., et al., Autoantibody-negative insulin-dependent diabetes mellitus after SARS-CoV-2 infection: a case report. 2020.
- Pal, R., et al., Clinical profile and outcomes in COVID-19 patients with diabetic ketoacidosis: A systematic review of literature. Diabetes Metab Syndr, 2020. 14(6): p. 1563-1569.
- Smati, S., et al., Euglycaemic ketoacidosis during gestational diabetes with concomitant COVID-19 infection. Diabetes Metab, 2020.
- Batista, D.V., C. Vieira, and T.A. Costa, COVID-19-associated euglycemic diabetic ketoacidosis in a patient with type 2 diabetes on SGLT2 inhibitor: a case report. 2020: p. 1-4.
- Palermo, N.E., A.R. Sadhu, and M.E. McDonnell, Diabetic Ketoacidosis in COVID-19: Unique Concerns and Considerations. J Clin Endocrinol Metab, 2020. 105(8).
- Oriot, P. and M.P. Hermans, Euglycemic diabetic ketoacidosis in a patient with type 1 diabetes and SARS-CoV-2 pneumonia: case report and review of the literature. Acta Clin Belg, 2020: p. 1-5.
- Fang, J., M. Genco, and R.N. Caskey, COVID-19 Precipitating Euglycaemic Diabetic Ketoacidosis with SGLT2 Inhibitor Use. Eur J Case Rep Intern Med, 2020. 7(11): p. 001943.
- Tollard, C., et al., An inaugural diabetic ketoacidosis with acute pancreatitis during COVID-19. 2020: p. 1-3.
- Naguib, M.N., J.K. Raymond, and A.P. Vidmar, New onset diabetes with diabetic ketoacidosis in a child with multisystem inflammatory syndrome due to COVID-19. J Pediatr Endocrinol Metab, 2020.
- Hoffmann, M., et al., SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell, 2020. 181(2): p. 271-280.e8.
- Yang, J.K., et al., Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes.Acta Diabetol, 2010. 47(3): p. 193-9.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi