Research Article, J Surg Clin Pract Vol: 3 Issue: 1
Evaluation of Cost-Effectiveness of Laparoscopic Ventral and Incisional Hernia Repair Service in a District General Hospital
Nehemiah Samuel1, Qaiser Jalal1*, Victoria Proctor2, Fayyaz Ali Khan Mazari3 and Muhammad Hanif Shiwani2
1Northern General Hospital, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom
2Barnsley Hospital NHS Foundation Trust, United Kingdom
3University Hospital Southampton NHS Foundation Trust, United Kingdom
*Corresponding Author : Qaiser Jalal
Hepatopancreaticobiliary Unit Northern
General Hospital, Sheffield Teaching
Hospitals NHS Foundation Trust
Sheffield, United Kingdom
E-mail: drque71@hotmail.com
Received: September 14, 2018 Accepted: July 15, 2019 Published: July 29, 2019
Citation: Samuel N, Jalal Q, Proctor V, Mazari FAK, Shiwani MH (2018) Evaluation of Cost-Effectiveness of Laparoscopic Ventral and Incisional Hernia Repair Service in a District General Hospital. J Surg Clin Pract 2:3. doi: 10.4172/JSCP.1000118
Abstract
Background: Laparoscopic repair of ventral and incisional hernias (LRVIH) is a safe technique. This study explores the clinical and cost effectiveness of providing this service in a district general hospital.
Methods: This prospective single-centre, single-surgeon study included consecutive patients who underwent LRVIH over 6years. Demographics, surgery details and follow-up data were recorded. Costs and income were calculated from NHS payment by result (PBR) tariffs. Intergroup analysis was performed for hernia type, width class and size.
Results: 101patients with median age of 57years (interquartile range IQR 46 to 67years) and median body mass index of 32.0 kg/m2 (IQR27.7 to 35.6kg/m2) underwent repairs for 21(20.8%) primary ventral, 65(64.4%) incisional and 15(14.8%) recurrent hernias. 20(19.8%) patients had multiple abdominal wall defects at surgery. Median defect size was 25cm2 (IQR 12 to 86cm2), with epigastrium being the commonest site. Median operating time was 70minutes (IQR 60 to 110 minutes). 22(21.8%) patients had day-case surgery and overall median length of hospital stay was 1.5 bed days (IQR 1.0 to 2.0 bed days). 4(4.0%) had conversion to open procedure. 22(21.8%)
patients had complications (9 seromas, 2 haematomas, 5 respiratory complications, 7 prolonged postoperative pain) but only 2(2.0%) patients needed re-operations for adhesive small bowel obstruction. Median cost of repair was £1567.92 (IQR £1343.04 to £1991.00) and hospital income per procedure was £1747.00 (IQR £1163.00 to 2534.00), with median income of £-1.92 (IQR £-278.25 to £542.16). Laparoscopic repair was cost neutral on all intergroup analyses.
Conclusion: This study demonstrates that LRVIH is safe and cost-effective for all hernia types and sizes. Laparoscopic repair of small hernias can provide a good training opportunity for surgeons without increasing the costs.
Keywords: Ventral hernia; Incisional hernia, laparoscopic repair; Cost effectiveness
Keywords
Ventral hernia; Incisional hernia; Laparoscopic repair; Cost effectiveness
Introduction
Ventral hernias are congenital or acquired defects of the anterior abdominal wall [1]. Congenital ventral hernias are frequently epigastric, paraumbilical or umbilical defects while acquired hernias are usually incisional. Although a large proportion of ventral hernia patients are asymptomatic, a significant majority presents with a range of complaints like abdominal discomfort, visible lump, bulge, poor cosmesis, recurrent abdominal pain, gastrointestinal obstruction, strangulation and intestinal perforation [2,3]. The methods of repair of ventral hernia have always divided the surgeons [4,5]. Studies have reported good outcomes with open and laparoscopic repair of ventral and incisional hernias [6]. More recent studies have shown that laparoscopic approach of ventral hernia repair is at least as effective, if not superior to the open approach with added advantage of shorter operating times, hospital stay and possibly lower incidence of wound infections [1,6-8]. Another reported advantage of the laparoscopic method is that it allows reliable identification of all abdominal wall defects which may not be detected clinically, thus having the potential for reducing recurrence rates [2,9]. These factors have led to an increase in the use of laparoscopic repair methods. Despite the growing practice, there is still not enough evidence regarding the cost implications of laparoscopic method of repair [1,3,7-11]. This study was designed to assess the clinical and cost implications of introducing laparoscopic repair of ventral and incisional hernias (LRVIH) in a district general hospital in the United Kingdom (UK).
Materials and Methods
Study design and patient selection
This was a prospective observational study of consecutive patients who underwent LRVIH at a busy district general hospital from January 2009 to August 2015. The study was approved by the hospital governance and service review board. All patients were under the care of a single consultant surgeon with expertise in laparoscopic hernia repair. Patients were seen first in the outpatient clinic and had a detailed history and physical examination. Demographics, risk factors and examination findings were recorded. The site and size of all hernias was recorded and classified according to the system recommended by the European Hernia Society (EHS) [12]. All patients were offered the choice of having laparoscopic or open repair of their hernias. Patients who opted to have laparoscopic repair were included in the study. All operations were performed by the same surgeon under general anaesthesia. Choice of laparoscopic equipment, mesh, tracking device and sutures was at surgeon’s discretion. The duration of surgery and length of post-operative stay in hospital was also recorded. Patients were reviewed in follow up clinic at six weeks, six months and one year after surgery. Complication and recurrence rates were recorded to assess clinical effectiveness of the technique and used as outcome measures. Complications were classified according to the Clavien – Dindo complication grading system [13]. Recurrence of hernia was regarded as failure of procedure and was not included in the complication grading.
Cost analysis
Procedure specific costs were calculated for laparoscopic hernia repair for all patients. Standard tariffs including costs for overheads and consumables were obtained from the finance department of the hospital for theatre time (£577 per hour) and for hospital stay (£154 per day). Individual costs for each patient were then calculated by multiplying these tariffs with actual theatre time used and time spent in hospital. The cost of mesh and mechanical tacking device (£250 per unit) used in each case was then added to calculate the total cost of procedure borne by the hospital for each individual patient. Indirect costs like time off work, clinic visits, and travel and carer costs were excluded. Income was calculated using the Health Resource Group (HRG) codes and the associated National Health Service Payment by results (NHS – PBR) tariffs. These comprise a fixed price payment system currently used in the National Health Service (NHS) in the United Kingdom (UK). The system does not allow any risk adjustment for observable cost drivers such as age, gender and risk factors. However, there is some adjustment available for additional bed days; size of hernia and co-morbidities but the relationship is not linear (10).
HRG codes were obtained for each patients and tariff for each code was multiplied by the applicable market forces factor (also specified according to each individual region in NHS – PBR system) to calculate the total income per procedure. Net profit or loss was calculated by subtracting the total costs from the total income for each individual procedure.
Statistical analysis
Data was collected on source documents specifically designed for the study. Statistical analysis was performed using  23.0 (IBM Corporation, Armonk, USA). Continuous variables were represented as median with interquartile range (IQR) while categorical variables were represented as percentage (%) with actual number (N). Inter-group comparisons were performed based on the type of hernia, the width and surface area of the hernia defect. Comparison of continuous variables was performed using non-parametric tests (Mann Whitney U test/Kruskal Wallis ANOVA) while categorical variables were compared using Chi-square test or linear by linear association in case of more than two categories. Level of significance was set at 0.05. “Test minimisation approach” was used to limit the total number of statistical comparisons. Statistical testing was only performed if there was a 10% difference observed between the groups for the categorical variables and for a 20% difference between groups for continuous variables.
23.0 (IBM Corporation, Armonk, USA). Continuous variables were represented as median with interquartile range (IQR) while categorical variables were represented as percentage (%) with actual number (N). Inter-group comparisons were performed based on the type of hernia, the width and surface area of the hernia defect. Comparison of continuous variables was performed using non-parametric tests (Mann Whitney U test/Kruskal Wallis ANOVA) while categorical variables were compared using Chi-square test or linear by linear association in case of more than two categories. Level of significance was set at 0.05. “Test minimisation approach” was used to limit the total number of statistical comparisons. Statistical testing was only performed if there was a 10% difference observed between the groups for the categorical variables and for a 20% difference between groups for continuous variables.
Results
Demographics
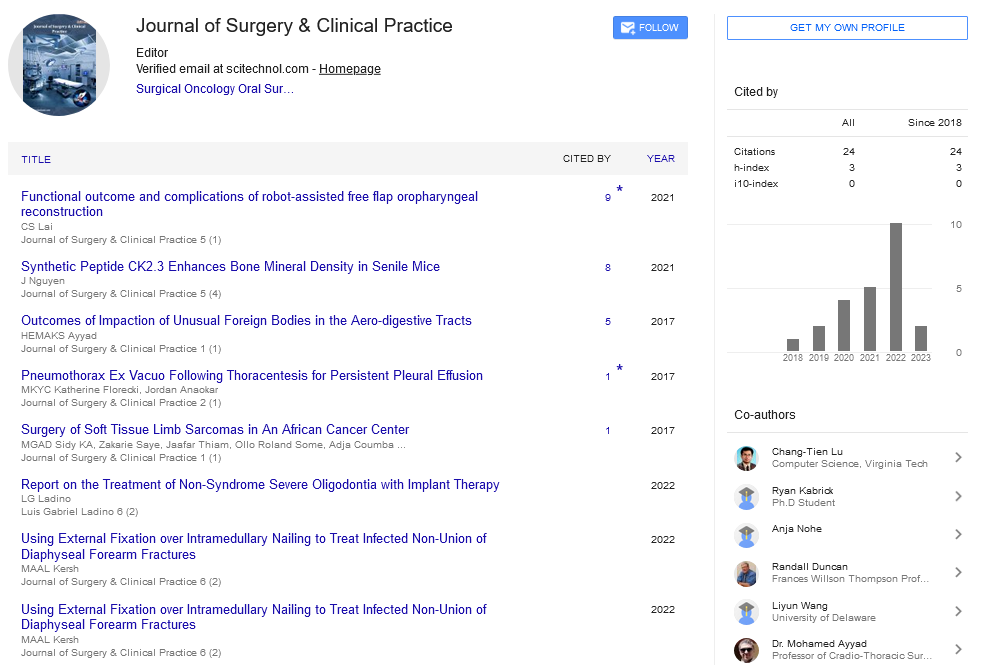
101 patients underwent laparoscopic repair of their ventral or incisional hernias and were included in the study. Median age was 57 years (IQR 46 to 67 years). There was an equal representation of both genders (male 51, female 50). Most patients were non-smokers (N=63) with median body mass index of 32.0 (IQR 27.7 to 35.6). The demographic details are summarised in Table 1.
| Parameter | Median/Number | IQR/Percentage | |
|---|---|---|---|
| Age (years) | 57 | 46 to 67 | |
| Weight (kilograms) | 89.9 | 77.0 to 99.2 | |
| Body mass index (kilograms/metre2) | 32 | 27.7 to 35.6 | |
| Gender | Male | 51 | 50.50% |
| Female | 50 | 49.50% | |
| Smoking status | Non-smoker | 63 | 62.40% |
| Ex-smoker | 23 | 22.80% | |
| Smoker | 15 | 14.90% | |
| ASA Grade | 1 | 26 | 25.70% |
| 2 | 60 | 59.40% | |
| 3 | 15 | 14.90% | |
| Hernia Parameters | |||
| Hernia type | Primary ventral | 21 | 20.80% |
| Incisional | 65 | 64.40% | |
| Recurrent hernia | 15 | 14.90% | |
| Recurrent incisional hernia | 11 | 10.90% | |
| Number of defects | 1 | 81 | 80.20% |
| 2 | 10 | 9.90% | |
| 3 | 3 | 3.00% | |
| 4 or more | 7 | 6.90% | |
| Defect size (cm2) | 25 | 12.0 to 86.0 | |
| Size based | groups < 25 cm2 | 51 | 50.50% |
| > 25 cm2 | 43 | 42.60% | |
| Missing data | 7 | 6.90% | |
| European Hernia Society Classification | |||
| Midline | M1 (Subxiphoid) | 4 | 4.00% |
| M2 (Epigastric) | 39 | 38.60% | |
| M3 (Umbilical) | 33 | 32.70% | |
| M4 (Infraumbilical) | 9 | 8.90% | |
| M5 (Suprapubic) | 3 | 3.00% | |
| Lateral | L1 (Subcostal) | 0 | 0.00% |
| L2 (Flank) | 1 | 1.00% | |
| L3 (Iliac) | 3 | 3.00% | |
| L4 (Lumbar) | 0 | 0.00% | |
| Mixed | M2 M3 | 4 | 4.00% |
| M3 M4 | 1 | 1.00% | |
| M3 L2 | 1 | 1.00% | |
| Missing data | 3 | 3.00% | |
| Width | W1 (<4 cm) | 29 | 28.70% |
| W2 (4 to 10 cm) | 46 | 45.50% | |
| W3 (>10 cm) | 23 | 22.80% | |
| Missing data | 3 | 3.00% | |
This table represents the demographics and hernia parameters for study participants. IQR: Interquartile Range; ASA: American Society of Anaesthesiologists
Table 1: Demographics and hernia parameters for study participants.
Hernia parameters
Two third of patients had incisional hernia (N=65). 15 patients had recurrent hernias while 11 patients had recurrent incisional hernias. 94% (N=93) had a midline hernia and 20% (N=20) had more than one abdominal wall defect at the time of surgery. Epigastrium was the most common site. Median defect size was 25 square centimetres. The detailed hernia parameters according to the EHS classification are summarised in Table 1.
Operative parameters and outcomes
The median operating time was 70 minutes (IQR 60 to 110 minutes). 102 meshes were used with one patient requiring two meshes for complete coverage.  (Ethicon Incorporated, Somerville, New Jersey, USA) was the commonest mesh used in 68.3% (N=69) of cases. Other meshes used included
(Ethicon Incorporated, Somerville, New Jersey, USA) was the commonest mesh used in 68.3% (N=69) of cases. Other meshes used included  (Ethicon Incorporated, Somerville, New Jersey, USA) and
(Ethicon Incorporated, Somerville, New Jersey, USA) and  (Ethicon Incorporated, Somerville, New Jersey, USA). A single disposable tacking device was used in all cases. 4.0% (N=4) had the laparoscopic operation converted to open surgery due to extensive adhesions. Median hospital stay was 1.5 days. 21.8% (N=22) of patients had their procedure as a day case and another 33.7% (N=34) of patients stayed in hospital for one night only (Table 2). 21.8% (N=22) patients experienced post-operative complications with most patients experiencing minor complications only that did not require any surgical intervention. 2 patients required surgery for small bowel obstruction due to adhesions in the postoperative period (1 laparotomy, 1 laparoscopy). 5.9% (N=6) had a recurrence of hernia during the 12 months follow up (Table 3).
(Ethicon Incorporated, Somerville, New Jersey, USA). A single disposable tacking device was used in all cases. 4.0% (N=4) had the laparoscopic operation converted to open surgery due to extensive adhesions. Median hospital stay was 1.5 days. 21.8% (N=22) of patients had their procedure as a day case and another 33.7% (N=34) of patients stayed in hospital for one night only (Table 2). 21.8% (N=22) patients experienced post-operative complications with most patients experiencing minor complications only that did not require any surgical intervention. 2 patients required surgery for small bowel obstruction due to adhesions in the postoperative period (1 laparotomy, 1 laparoscopy). 5.9% (N=6) had a recurrence of hernia during the 12 months follow up (Table 3).
| Parameter | Median (IQR)/N (%) | Unit cost (£) | |
|---|---|---|---|
| Operating time (minutes) | 70.0 (60.0 to 110.0) | 577.00 per hour | |
| Tacking device | 101 (100.0%) | 250 | |
| Hospital stay (days) | 1.5 (1.0 to 2.0) | 154 per day | |
| Day case procedure | 22 (21.8%) | - | |
| Mesh used | |||
| PROCEEDâ | 15 × 15 cm | 41 (40.2%) | 290 |
| 15 × 20 cm | 19 (18.6%) | 481 | |
| 20 × 25 cm | 6 (5.9%) | 735 | |
| 20 × 30 cm | 1 (1.0%) | 825 | |
| 25 × 35 cm | 2 (2.0%) | 1174 | |
| 30×× 30 cm | 1 (1.0%) | 1174 | |
| PHYSIOMESHâ | 12 × 15 cm | 13 (12.7%) | 309 |
| 15 × 20 cm | 13 (12.7%) | 422 | |
| 20 × 30 cm | 5 (4.9%) | 825 | |
| ULTRAPROâ | 15 × 15 cm | 1 (1.0%) | 290 |
This table represents the operative parameters for the study participants. IQR: Interquartile Range; N: Number; £: Pound Sterling
Table 2: Operative parameters for study participants.
| Complication | Number of patients (%) | Clavien – Dindo complication grade |
|---|---|---|
| Any complication | 22 (21.8%) | - |
| Haematoma | 2 (2.0%) | Grade 1 |
| Seroma | 9 (8.9%) | |
| Acute urinary retention | 2 (2.0%) | |
| Slow recovery | 1 (1.0%) | |
| Prolonged postoperative pain | 7 (6.9%) | |
| Respiratory complications | 5 (4.9%) | Grade 2 |
| Wound infection requiring antibiotics | 1 (1.0%) | |
| Postoperative ileus | 1 (1.0%) | |
| Small bowel obstruction requiring surgery | 2 (2.0%) | Grade 3 |
| Recurrence of hernia | 6 (5.9%) | - |
| This table represents the complications and recurrence rates observed in the study participants. | ||
Table 3: Complication and recurrence rates for study participants.
Economic outcomes
The median cost per procedure was £1567.92 (IQR £1343.04 to £1991.00). The median income per procedure for the hospital was £1747.00 (IQR £1163.00 to 2534.00). Overall, the procedures were cost neutral with median net income of £-1.92 (IQR £-278.25 to £542.16).
Inter-group analysis
Three Inter-group analyses were performed based on the type of hernia, the width categories as defined in the European Hernia Society (EHS) classification (Table 1) and the size of the hernia defect. Analysis based on location of hernia was not performed due to multiple sub categories and small sample sizes.
Analysis based on hernia type: There were no differences between the groups for age, gender, body mass index (BMI) or smoking status. There was a significant difference in ASA grade with a higher proportion of ASA1 patients in primary ventral hernia group. Also, the defect size, operative duration and cost per procedure were significantly higher in incisional and recurrent incisional hernia groups. There were no differences between groups for hospital stay, income per procedure or net income (Table 4).
| Parameter | Hernia type | P value | |||
|---|---|---|---|---|---|
| Primary ventral (N=21) |
Incisional hernia (N=65) |
Recurrent hernia (N=15) |
0.001 | ||
| ASA grade | 1 | 13 (61.9%) | 13 (20.0%) | 0 (0.0%) | |
| 2 | 7 (33.3%) | 42 (64.6%) | 11 (73.3%) | ||
| 3 | 1 (4.8%) | 10 (15.4%) | 4 (26.7%) | ||
| Defect size (cm2) | 12.5 (9.0 to 25.0) | 27.5 (16.0 to 120.0) | 42 (12.0 to 96.0) | 0.013 | |
| Operative duration (minutes) | 60 (40.0 to 75.0) | 70 (60.0 to 120.0) | 65 (55.0 to 150.0) | 0.034 | |
| Hospital stay (days) | 1 (1.0 to 2.0) | 1.5 (0.5 to 2.0) | 2 (1.0 to 4.0) | 0.346 | |
| Cost per procedure (£) | 1425.00 (1178.29 to 1597.33) | 1713.50 (1412.58 to 2142.79) | 1616.00 (1425.00 to 2191.50) | 0.023 | |
| Income per procedure (£) | 1415.00 (1163.00 to 1705.00) | 1747.00 (1163.00 to 2534.00) | 1663.00 (1415.00 to 2534.00) | 0.131 | |
| Net income to hospital (£) | 65.33 (-236.21 to 607.70) | 46.17 (-295.87 to 553.50) | -50.5 (-453.00 to 76.92) | 0.422 | |
This table represents the Inter-group analysis based on the type of hernia. P values are significant at 0.05 level. Significant comparisons are represented in bold. N: Number; ASA: American Society of Anaesthesiologists; £: Pound Sterling
Table 4: Inter-group analysis based on hernia type.
Analysis based on EHS width category: There was no difference between groups for age, gender, BMI, smoking status and ASA grade. There were some differences between groups for the type of hernia with primary ventral hernia more common in the W1 group and incisional hernias more common in the W2 and W3 groups. W3 hernias were significantly larger than other groups with a longer operative time, cost and income per procedure as compared to the other groups. However, there was no difference in hospital stay or net income to hospital (Table 5).
| Parameter | EHS width category | P value | |||
|---|---|---|---|---|---|
| W1 (N=29) |
W2 (N=46) |
W3 (N=23) |
|||
| Hernia type | Primary ventral | 12 (41.4%) | 7 (15.2%) | 1 (4.3%) | 0.012 |
| Incisional | 14 (48.3%) | 31 (67.4%) | 19 (82.6%) | ||
| Recurrent | 3 (10.3%) | 8 (17.4%) | 3 (13.0%) | ||
| Defect size (cm2) | 9 (4.0 to 9.0) | 25 (20.0 to 43.7) | 160 (120.0 to 271.5) | 0.001 | |
| Operative duration (minutes) | 70 (60.0 to 90.0) | 60 (55.0 to 90.0) | 115 (75.0 to 120.0) | 0.002 | |
| Hospital stay (days) | 1.5 (1.0 to 2.0) | 1 (0.5 to 2.0) | 1.5 (1.0 to 6.0) | 0.18 | |
| Cost per procedure (£) | 1462.00 (1386.50 to 1828.50) | 1425.00 (1206.50 to 1729.69) | 1980.00 (1760.25 to 3063.00) | 0.001 | |
| Income per procedure (£) | 1415.00 (1289.00 to 1630.00) | 1539.00 (1163.00 to 2534.00) | 2534.00 (2484.00 to 2931.00) | 0.001 | |
| Net income to hospital (£) | -18.08 (-280.25 to 235.04) | 22.12 (-268.00 to 540.50) | 55.5 (-529.00 to 765.50) | 0.761 | |
This table represents the Inter-group analysis based on the European Hernia Society width categories. P values at significant at 0.05 level. Significant comparisons are highlighted in bold. EHS: European Hernia Society; W1: Hernia Defect Width <4 cm; W2: Hernia Defect Width 4 -10 cm; W3: Hernia Defect Width >10 cm; £ - Pound Sterling
Table 5: Inter-group analysis based on European Hernia Society width category.
Analysis based on median defect size: The median size of defect observed in the study (25 cm2) was used to divide the patients into two groups namely patients with hernia size less then and more than 25 cm2 respectively. Patients in the <25 cm2 group were younger and fit with more primary ventral hernias as compared to those with the larger hernia sizes. There were no differences in gender, BMI and smoking status. Patients in the >25 cm2 group had significantly longer operative times, hospital stay, cost and income per procedure.
However, there was no difference between group in the net income to hospital (Table 6).
| Parameter | Hernia size | P value | ||
|---|---|---|---|---|
| < 25 cm2 (N=51) | > 25 cm2 (N=43) | |||
| Age (years) | 53 (44 to 64) | 62 (51 to 69) | 0.022 | |
| ASA grade | 1 | 18 (35.3%) | 6 (14.0%) | 0.009 |
| 2 | 30 (58.8%) | 27 (62.8%) | ||
| 3 | 3 (5.9%) | 10 (23.3%) | ||
| Hernia type | Primary ventral | 16 (31.4%) | 4 (9.3%) | 0.021 |
| Incisional | 30 (58.8%) | 30 (69.8%) | ||
| Recurrent | 5 (9.8%) | 9 (20.9%) | ||
| Defect size (cm2) | 12 (9.0 to 25.0) | 108 (42.0 to 160.0) | 0.001 | |
| Operative duration (minutes) | 60 (55.0 to 80.0) | 90 (60.0 to 120.0) | 0.001 | |
| Hospital stay (days) | 1 (0.5 to 2.0) | 1.5 (1.0 to 3.0) | 0.047 | |
| Cost per procedure (£) | 1425 (1194.00 to 1616.00) | 1854.92 (1558.17 to 2383.00) | 0.001 | |
| Income per procedure (£) | 1415 (1163.00 to 1747.00) | 2534 (1747.00 to 2931.00) | 0.001 | |
| Net income to hospital (£) | -10 (-185.00 to 463.50) | 30.35 (-453.00 to 765.50) | 0.448 | |
This table represents the Inter-group comparison based on the size of hernia defect. P values are significant at 0.05 level. Significant comparisons are represented in bold. N: Number; £: Pound Sterling
Table 6: Inter-group analysis based on size of hernia defect.
Discussion
This study demonstrates that introduction of laparoscopic repair of ventral and incisional hernias as a new service is clinically safe and cost neutral in a district general hospital setting. It also raises a few interesting questions regarding the indications, outcomes and costs of laparoscopic repair in clinical practice. Despite the wide spread application of laparoscopic ventral and incisional hernia repairs, little has been published regarding some fundamental issue like indication and contraindications of this technique. Majority of experience surgeons would regard pain, limitation of daily activities, progressive enlargement, incarceration, respiratory dysfunction, young age and cosmetic complains as the indication for repair. The relative contraindications include asymptomatic hernias, significant comorbidity, obesity, old age, large size, non-progression, loss of abdominal wall and small hernia [3]. This study challenges a few of these assumptions. All patients in this study were referred to the surgical outpatient clinic for consideration of hernia repair by their family doctors in the primary care setting or from other surgical specialists. “Walk in” surgical consultations were not available for patients at this hospital. Therefore, all patients who were referred and had an incisional hernia were offered treatment with the assumption that patients who were asymptomatic or unfit for intervention were filtered out in the primary care setting. Also, the patient population in this study had a relatively high median weight and body mass index (BMI), however, the clinical outcomes were comparable to the early experiences reported by other institutions [14-16]. There was a higher proportion of incisional and recurrent hernias as compared to primary ventral hernias. The reported incidence of incisional hernia ranges from 3% to 20% occurring in approximately 10% of patients with uncomplicated wounds and 20%-25% patients with complicated wounds [2,7]. Around 600,000 patients undergo abdominal surgery in the UK each year, thus making 18,000 to 120,000 patients susceptible to the development of incisional hernia annually. This explains the higher representation of this hernia type in the study cohort. Also, the size of hernia defects varied hugely in this study. As subjective measurement of size and site of hernia by individual surgeons can differ significantly, using the European Hernia Society (EHS) system to classify the hernias made it more objective and easy to stratify the different hernia types based on location and size [12]. It also provided the investigators with a sound basis for planning intervention and for performing meaningful comparisons between groups. It also adds to the generalisability of this study to day-to-day practice in different setups and populations, and increases its reproducibility in other institutions locally and internationally.
The operating time in this study is similar to other studies [8,17,18]. A decrease in operative duration was observed over the time of the study indicating the learning curve. However, the numbers were small to perform a meaningful analysis. The duration of hospital stay in this study was also comparable to previous studies that have reported inpatient stay ranging from 1 to 5.7 days [8,17]. Interestingly, there was a trend towards longer hospital stay in patients with larger incisional or recurrent hernias as compared to patients with small sized primary ventral hernias. This is not a unique finding and the lack of significance may be a consequence of small sample size [19]. However, it can be argued that the difference between these groups would be much more pronounced if they were undergoing open repair of their hernias.
Therefore, it is likely that the laparoscopic method of repair may have an impact on reducing the hospital stay for these patients as shown in previous studies [19,20]. A definitive conclusion cannot be reached in this study due to the absence of a comparative arm of open repair of hernias.
Seroma was the most common complication. The seroma rates observed were similar to the previously reported seroma formation rates of 11% to 17% [8,17,21]. It is not unexpected as a significant number of patients in this study had large hernias. Interestingly none of these patients required any further intervention and the seromas settled with conservative management. Postoperative pain was the second most commonly encountered immediate complication which was resolved by adjustment of analgesics and use of neuromodulators in some cases. Again, the incidence of pain in this study was similar to the figures reported in previous studies [20,22]. Also, it is well reported that there is no significant difference in postoperative wound pain between laparoscopic and open repair methods for these hernias [1,18,20,23,24]. Overall complication rates were also in line with the published literature [25,26]. Serious complications occurred in only 2% of patients who made a full recovery. This provides good evidence on the clinical safety of the laparoscopic repair procedure. Recurrence rates at one year are relatively low in this study. Recurrence rates of 3% to 18% have been reported in the previous studies [18,23,25,27]. These results are very encouraging and support the clinical effectiveness of this type of repair.
Cost analysis results in this study also answer some interesting questions. It has been argued in the past that laparoscopic repair of small ventral and incisional hernias is expensive [28,29]. Some surgeons reserve the laparoscopic repair for large, recurrent and multiple hernias [30]. This study demonstrated that laparoscopic repair of small and large, ventral and incisional hernias is cost neutral. Even in fixed payment systems like the NHS, this form of repair is still cost effective in all ventral hernia types and sizes. It is likely that the procedures would be more profitable for the hospitals in insurance based health care systems as the chargeable tariffs are relatively higher. The study identifies the need for increasing the tariff payments for smaller hernias. Furthermore, cost neutrality of these procedures can also support the argument for the training of surgeons in these procedures. Small primary ventral and incisional hernias provide an excellent opportunity to train new surgeons and to refine newly acquired skills in laparoscopic hernia repair. It also helps to prepare the surgeons for handling more difficult, complex and large hernias. The study has shown that repair of larger hernias is more time consuming as compared to the smaller ones. However, in the absence of the practice opportunity provided by the smaller hernias, these procedures are likely to take even longer. One has to say that this study was not designed to investigate this particular aspect, but logical extrapolation of its results support this argument.
The study has some inherent limitations. It is a single centre, single surgeon study. There is no comparative arm for open hernia repair. The follow-up period is relatively short, and the cost effectiveness analysis is limited to immediate costs related directly to the operative procedure only. However, it provides useful evidence for establishment of new laparoscopic hernia repair service and also provides basis for designing a comparative trial with appropriate cost utility analysis. The follow up arrangements in this study are reflective of the current clinical practice as long-term follow-up are no longer performed for hernia repairs as most of the care commissioning groups do not support continuing follow-ups routinely.
Conclusion
Laparoscopic ventral and incisional hernia repair is a safe and cost neutral procedure. Laparoscopic repair of small hernias can provide a good training opportunity for surgeons without increasing the costs. Laparoscopic repair of larger hernias incurs additional costs but brings in extra income to make it cost effective for hospitals to provide these services.
References
- Sajid MS, Bokhari SA, Mallick AS, Cheek E, Baig MK (2009) Laparoscopic versus open repair of incisional/ventral hernia: A meta-analysis. Am J Surg 197: 64-72.
- Kingsnorth A, Banerjea A, Bhargava A (2009) Incisional hernia repair – laparoscopic or open surgery? Ann R Coll Surg Engl 91: 631-636.
- Nieuwenhuizen J, Kleinrensink GJ, Hop WC, Jeekel J, Lange JF (2008) Indications for incisional hernia repair: An international questionnaire among hernia surgeons. Hernia 12: 223-225.
- Veenendaal N, Poelman M, Bonjer J (2015) Controversies in laparoscopic ventral hernia repair. Minerva Chir 70: 481-492.
- Pawlak M, Bury K, Smietanski M (2015) The management of abdominal wall hernias – in search of consensus. Wideochir Inne Tech Maloinwazyjne 10: 49-56.
- Silecchia G, Campanile FC, Sanchez L, Ceccarelli G, Antinori A, et al. (2015) Laparoscopic ventral/incisional hernia repair: Updated Consensus Development Conference based guidelines. Surg Endosc 29: 2463-2484.
- Olmi S, Scaini A, Cesana GC, Erba L, Croce E (2007) Laparoscopic versus open incisional hernia repair: An open randomized controlled study. Surg Endosc 21: 555-559.
- Forbes SS, Eskicioglu C, McLeod RS, Okrainec A (2009) Meta-analysis of randomized controlled trials comparing open and laparoscopic ventral and incisional hernia repair with mesh. Br J Surg 96: 851-858.
- Salvilla SA, Thusu S, Panesar SS (2012) Analysing the benefits of laparoscopic hernia repair compared to open repair: A meta-analysis of observational studies. J Minim Access Surg 8: 111-117.
- Poulose BK, Shelton J, Phillips S, Moore D, Nealon W, et al. (2012) Epidemiology and cost of ventral hernia repair: Making the case for hernia research. Hernia 16: 179-183.
- Bower C, Roth JS (2013) Economics of abdominal wall reconstruction. Surg Clin North Am 93: 1241-1253.
- Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, et al. (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13: 407-414.
- Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240: 205-213.
- Bamehriz F, Birch DW (2004) The feasibility of adopting laparoscopic incisional hernia repair in general surgery practice: Early outcomes in an unselected series of patients. Surg Laparosc Endosc Percutan Tech 14: 207-209.
- Varghese TK, Denham DW, Dawes LG, Murayama KM, Prystowsky JB, et al. (2002) Laparoscopic ventral hernia repair: An initial institutional experience. J Surg Res 105: 115-118.
- Ferrarese AG, Martino V, Enrico S, Falcone A, Catalano S, et al. (2013) Laparoscopic repair of wound defects in the elderly: Our experience of 5 years. BMC Surg 13: S23.
- Pham CT, Perera CL, Watkin DS, Maddern GJ (2009) Laparoscopic ventral hernia repair: A systematic review. Surg Endosc 23: 4-15.
- Nardi M, Millo P, Brachet Contul R, Lorusso R, Usai A, et al. (2017) Laparoscopic ventral hernia repair with composite mesh: Analysis of risk factors for recurrence in 185 patients with 5 years follow-up. Int J Surg 40: 38-44.
- Butler AR, Frelich MJ, Gould JC, Goldblatt MI (2014) Laparoscopic hernia complexity predicts operative time and length of stay. Hernia 18: 791-796.
- Wormer BA, Walters AL, Bradley JF, Williams KB, Tsirline VB, et al. (2013) Does ventral hernia defect length, width, or area predict postoperative quality of life? Answers from a prospective, international study. J Surg Res 184: 169-177.
- Tsimoyiannis EC, Siakas P, Glantzounis G, Koulas S, Mavridou P, et al.(2001) Seroma in laparoscopic ventral hernioplasty. Surg Laparosc Endosc Percutan Tech 11: 317-321.
- Berger D (2014) Diagnostics and therapy of chronic pain following hernia operation. Chirurg 85: 117-120.
- Eker HH, Hansson BM, Buunen M, Janssen IM, Pierik RE, et al. (2013) Laparoscopic vs. open incisional hernia repair: A randomized clinical trial. JAMA Surg 14: 259-263.
- Sauerland S, Walgenbach M, Habermalz B, Seiler CM, Miserez M (2011) Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev 3: Cd007781.
- Itani KM, Hur K, Kim LT, Anthony T, Berger DH, et al. (2010) Comparison of laparoscopic and open repair with mesh for the treatment of ventral incisional hernia: A randomized trial. Arch Surg 145: 322-328.
- Mann CD, Luther A, Hart C, Finch JG (2015) Laparoscopic incisional and ventral hernia repair in a district general hospital. Ann R Coll Surg Engl 97: 22-26.
- Helgstrand F, Rosenberg J, Kehlet H, Jorgensen LN, Bisgaard T (2013) Nationwide prospective study of outcomes after elective incisional hernia repair. J Am Coll Surg 216: 217-228.
- Cuccurullo D, Piccoli M, Agresta F, Magnone S, Corcione F, et al. (2013) Laparoscopic ventral incisional hernia repair: Evidence-based guidelines of the first Italian Consensus Conference. Hernia 17: 557-566.
- Overhaus M, Schaudienst CB, Nohl Y, Vilz TO, Hirner A, et al. (2011) Cost-effectiveness of hernia repair : IPOM versus open sublay mesh technique. Chirurg 82: 813-819.
- Arteaga-Gonzalez I, Martin-Malagon A, Fernandez EM, Carrillo-Pallares A (2010) Which patients benefit most from laparoscopic ventral hernia repair? A comparative study. Surg Laparosc Endosc Percutan Tech 20: 391-394.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi