Research Article, J Womens Health Issue Care Vol: 12 Issue: 3
Examining the Relationship between Pregnancy Intention and Adverse Maternal Outcomes
Chi Son Kim*, Takiyah Mitchell, Lauren Page, Shweta Karki and Josette Hartnett
Department of Obstetrics and Gynecology, Stamford Hospital, Stamford, United States
*Corresponding Author: Chi Son Kim
Department of Obstetrics and Gynecology,
Stamford Hospital,
Stamford,
United States;
E-mail: ckim6@stamhealth.org
Received date: 13 March, 2023, Manuscript No. JWHIC-23-91517;
Editor assigned date: 16 March, 2023, PreQC No. JWHIC-23-91517 (PQ);
Reviewed date: 30 March, 2023, QC No. JWHIC-23-91517;
Revised date: 10 May, 2023, Manuscript No. JWHIC-23-91517 (R);
Published date: 07 June, 2023, DOI: 10.4172/2325-9795.1000442
Citation:Kim CS, Mitchell T, Page L, Karki S, Hartnett J (2023) Examining the Relationship between Pregnancy Intention and Adverse Maternal Outcomes. J Womens Health Issue Care 12:3.
Abstract
Introduction: To investigate an association between pregnancy intention and maternal adverse outcomes, specifically postpartum depression.
Methods: Retrospective cohort study of 1105 pregnant patients between January 2015 to December 2017 who presented for prenatal care at optimus clinic (federally qualified health center). Inclusion criteria included singleton pregnancies and documented prenatal visit. Multifetal gestations, elective terminations and anyone with history of cervical insufficiency, pre-term delivery and/or premature rupture of membranes were excluded. The primary outcome is postpartum depression determined by Edinburgh postnatal depression scale at the six week postpartum visit. Secondary outcomes include incidence of development of hypertensive disorders in pregnancy, diabetes in pregnancy, contraception initiation postpartum and neonatal outcomes measured by Apgar scores and Neonatal Intensive Care Unit (NICU) admission.
Results: 56.6% of patients classified their pregnancy as unintended and 43.4% classified their pregnancy as intended. There was no significant difference found between the groups related to incidence of postpartum depression (p=0.07). No significant differences were found for secondary objectives studied including neonatal outcomes such as NICU admission or Apgar scores. Initiation of postpartum contraception was found to be significant, with the intended pregnancy cohort more likely to use postpartum contraception (89.2%, p=0.04).
Conclusion: More patients with unintended pregnancy screened positive for postpartum depression (68.6%) compared to those with intended pregnancies (31.2%, p=0.07). This can be considered clinically significant given present rates of unintended pregnancies in the United States and increasing focus on mental health issues such as postpartum depression. Pregnancy intention may an additional indicator for healthcare professionals to highlight interventions, tailor access to supportive services throughout pregnancy and postpartum to reduce postpartum depression.
Keywords: Pregnancy intention, Postpartum depression, Maternal morbidity, Postpartum contraception, Maternal outcome
Introduction
An unintended pregnancy can be either mistimed, such as when a pregnancy occurs earlier than desired or not desired at all. In 2011, 45% of pregnancies in the United States (US) were considered unintended, with 27% of pregnancies reported as being wanted later and 18% not desired. Studies have linked unintended pregnancies with maternal behaviors such as delayed entry into prenatal care smoking during pregnancy and delay or early cessation of breastfeeding. Adverse neonatal health outcomes have been extensively studied. However, data is limited on the maternal effects of an unintended pregnancy. Of the studies that have examined maternal health outcomes related to pregnancy intention, psychological distress is cited as a significant risk factor [1].
According to the Center for Disease Control and Prevention (CDCP), postpartum depression is experienced by 10%-15% of patient’s nationwide. Data from the Pregnancy Risk Assessment Monitoring System (PRAMS) for 2017 reported a national average of 12.5% postpartum depression, with the rate of postpartum depression in the state of Connecticut being similar at 12.7%. Postpartum depression has profound impact on the health and well-being of mother and child. For mothers, issues related to alcohol and illicit drug use and persistent depression and anxiety beyond the postpartum period can also be present. We planned to expand the literature available on examining the relationship between unintended. Pregnancies and maternal outcome of postpartum depression. We hypothesize higher rates of postpartum depression in patients with unintended pregnancy compared to intended/planned pregnancies [2].
Materials and Methods
Prior to study initiation, a waiver of informed consent was requested and approved by the Stamford hospital’s institutional review board of record. Data was retrospectively collected from January 1st, 2015 to December 21st, 2017 for all prenatal and postpartum visits at the Optimus health care clinic in Stamford, Connecticut. The Optimus clinic is a Federally Qualified Health Center (FQHC) that provides a range of services including Obstetrics and Gynecology (OB/GYN) to uninsured and low income patients in the community. Services are provided by nurse practitioners, family medicine and OB/GYN residents with the supervising attending physicians. Patients of all ages presenting with a singleton pregnancy were included if at least one prenatal care visit was documented. If multiple initial prenatal visits were present, the first prenatal visit was used for the study.
Patients were excluded from the study if the pregnancy was terminated or if there was no documentation of pregnancy intention at initial prenatal visit as they could not be categorized into a cohort. Patients with a history of cervical insufficiency, Pre-term Delivery (PTD) or Premature Rupture of Membranes (PROM) were also excluded as these are known associated factors that increase risk of adverse pregnancy outcomes. Demographic and other data points of interest were retrospectively extracted from the initial prenatal visit record including age, gestational age at presentation, gravity and parity, race, ethnicity, employment, marital status, Body Mass Index (BMI), total number of prenatal visits, toxic habits such as tobacco/ alcohol/illicit drug use and historical contraceptive use.
The primary objective of this study was to investigate if higher rates of postpartum depression were diagnosed among persons who identified their pregnancies as unintended compared to those who identified as intended/planned pregnancies. Secondary objectives were to evaluate other areas of maternal morbidity including development of gestational diabetes, hypertensive disorders in pregnancy, fetal/ neonatal outcomes, initiation and continuation of prenatal care, contraception initiation postpartum, incidence of subsequent short interval pregnancy and composite outcome measures that include CDC’s 21 indicators of severe maternal morbidity that are classified as unintended outcomes that result in significant consequences to a woman’s health, including death [3].
Statistical analysis for this research was conducted using SPSS version 28.0. Pregnancy intention cohorts were divided into “unintended” and “intended/planned” groups. This was established through chart review for documentation at the initial obstetric visit if the patient considered the pregnancy as planned or unplanned. There was no standardization of how the question was asked by the healthcare professional. Descriptive analyses were conducted between pregnancy intention groups (unintended, intended/planned) using the Chi-square test of the association for categorical variables and group ttest for continuous variables. Pregnancy outcomes for the variables of depression (based on a stratified Edinburgh Postnatal Depression Scale (EPDS) score less than nine or nine or greater, gestational diabetes, hypertensive diagnosis, postpartum contraceptive use and Neonatal Intensive Care Unit (NICU) admission were analyzed using Chi-square tests.
To measure our primary objective of postpartum depression, the EPDS was utilized which is a commonly used, validated, multilingual, ten item depression screening tool based on the participant reflecting on the past seven days. It is completed at the patient’s six week postpartum visit. At Optimus, a cutoff score greater than nine is considered a positive screen for depression at which further management options would be discussed. A score greater than eleven however would trigger a referral to behavioral health for more specialized discussion however clinical judgment should always be used including when scores don’t meet the recommended cutoff. EPDS scores were collected from participant’s medical record chart if the visit was attended and the score was documented.
An omnibus p-value of 0.05 was used for the determination of statistical significance for all tests. There were no corrections applied to the data for multiple comparisons as this research was exploratory in nature. No missing value imputation methods were used because data could not be assumed to be missing at random or completely at random and the MAR and MCA are assumptions that could not be validated [4].
Results
Of 1,105 patients seen at Optimus clinic during the study period, 801 patients met the inclusion criteria with 304 patients excluded based on exclusion criteria or absence of documentation of pregnancy intention at the initial OB visit (Figure 1). 56.6% (n=453) classified their pregnancy as unintended and 43.4% (n=348) were identified as intended/planned.
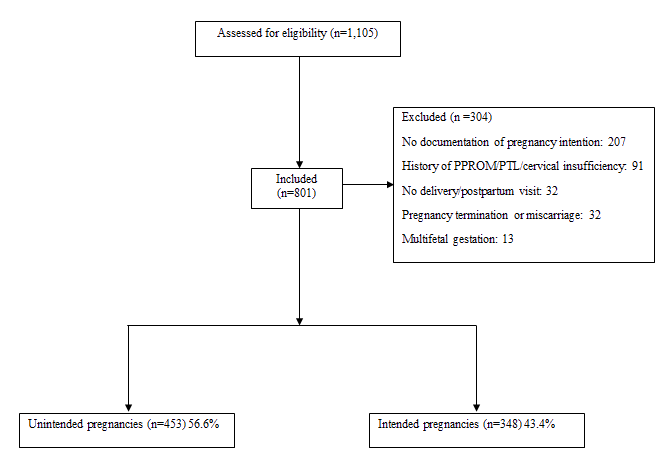
Figure 1: Flow chart of study participants.
Most of our population identified themselves as of white race and of hispanic and/or latinx ethnicity. Differences were observed between the study groups for age at initial prenatal visit, with the mean age being higher at 30 years old in intended cohort versus 28 years old in the unintended pregnancy cohort (p=0.002). Another difference was seen related to marital status, with 26.3% of patients in the unintended pregnancy cohort being married compared to 44.8% (p<0.001) in the intended pregnancy cohort. Participants who were employed were less likely to have unintended pregnancies (34.7%), compared to those who were unemployed (65.3%, p=0.01) [5]. A difference was also found related to gestational age at presentation of the initial prenatal visit (p=0.0003) with 12 weeks being the mean gestational age among those with intended pregnancies as compared to 14 weeks among those with unintended pregnancies. A higher percentage of patients reported use of pre-conception contraception in the unintended pregnancy group (43.4%) compared to 26.7% in the intended pregnancy cohort (p=0.007). On further breakdown, oral contraceptive pills (42.5%) followed by condom use (34.3%; p=0.003) were used for patients describing their pregnancy as unintended (Table 1).
Race
White324 (93.1%)421 (92.9%)0.001African American6 (1.7%)26 (5.7%)Asian11 (3.2%)4 (0.9%)Others7 (2%)2 (0.4%)Marital status
Single89 (25.6%)200 (44.2%)<0.0001Relationship98 (28.2%)124 (27.4%)Married156 (44.8%)119 (26.3%)Divorces2 (0.6%)7 (1.6%)Others3 (0.9%)3 (0.7%)Education
Primary school80 (30.3%)101 (28.9%)0.13High school116 (43.9%)184 (52.6%)Some college30 (11.4%)29 (8.3%)College degree38 (14.4%)35 (10%)Post-bachelor01 (0.3%)Currently employed
Yes113 (44.5%)119 (34.7%)0.02No141 (55.5%)224 (65.3%)Pre-conception contraceptive use
Yes28 (26.7%)56 (43.4%)0.007No77 (73.3%)73 (56.6%)Pre-conception contraceptive type
OCPs12 (36.4%)31 (42.5%)0.003*Nexplanon3 (9.1%)1 (1.4%) Depo3 (9.1%)8 (11%) IUD7 (21.2%)4 (5.5%) Condoms3 (9.1%)25 (34.3%) Others5 (15.2%)4 (5.5%) Gestational age at initial OB visit (weeks)12.55 (5.54%)14.11 (6.39%)0.0003Note: BMI: Body Mass Index; OCPs: Oral Contraceptive Pills; IUD: Intrauterine Device; OB: Obstetric; Data are mean ± SD or n (%); *Fisher’s test
Table 1: Demographic Characteristics.
No significant differences were found between intended and unintended groups for postpartum depression (p=0.07) using the EPDS tool. No significant differences were found for secondary objectives including incidence of hypertensive disorders in pregnancy, gestational diabetes or cesarean delivery. There were also no significant differences for neonatal outcomes including NICU admission or infant Apgar scores (Table 2).
Note: EPDS: Edinburgh Postnatal Depression Scale; PP: Postpartum; NSVD: Normal Spontaneous Vaginal Delivery; NICU: Neonatal Intensive Care Unit; Data presented as n (%) or SD
Table 2: Adverse maternal and neonatal outcomes based on pregnancy intention.
There was a significant difference found in the initiation of postpartum contraception use. Those with intended pregnancies were more likely to use post-partum contraception (89.2%) compared to patients with unintended pregnancies (83.8%, p=0.04).
Discussion
Though not reaching statistical significance, we found more patients with unintended pregnancy screen positive for postpartum depression compared to those with intended pregnancy. Given the present rates of unintended pregnancies along with the rising focus on the importance of maternal health, including mental health, exploring this area with attempts to fill in the knowledge is pivotal. However, many prospective cohort studies exploring this topic have had inconsistent findings associating pregnancy intention and postpartum depression. This is due to multiple factors such as study design, differences in ascertaining pregnancy intention and measuring postpartum depression, small sample sizes and inability to control for confounding factors [6].
Like other cohort studies, the current study found no association between pregnancy intention and postpartum depression. Looking at the use of the EPDS, our institution used the cutoff score of nine, at which time options are discussed with the patient including expectant management and following up on symptoms at a closer visit, an immediate referral to behavioral health/clinic therapist and/or the initiation of pharmacotherapy. Cut off scores similarly vary among the literature, however a recent meta-analysis reported that sensitivity and specificity to detect major depression in postpartum patients was greater for a cutoff value of 12 or higher. Using the EPDS was also dependent on whether patients were present at their six week postpartum visit, which as many as 40% of patients do not attend [7-9].
There was a statistically significant difference found between the cohorts and the initiation of postpartum contraception use with patients presenting with an intended pregnancy using contraception at a higher rate than those with unplanned pregnancies. Potential knowledge deficits and misperceptions surrounding contraceptive methods has been cited to be a major barrier to initiation as well as continuation. This highlights the importance of continued conversation of family planning and contraception options throughout prenatal care and not just at the six week postpartum visit of which the patient may or may not attend [10-12].
There were several limitations to this study. First, the population of the study was found to be homogenous with demographics showing predominantly caucasian race and hispanic ethnicity. Although the cohorts were based on pregnancy intention, we used a convenience sample, which could lead to potential bias towards or away from the null. Additionally, the total sample size included a review of over 1,000 patient charts but the effect size needed to power the study wasn’t met which could have led to a type II error. A general limitation can be found in the literature regarding the complicated processes on reporting pregnancy intention. In our study, the questioning of if this pregnancy was planned or unplanned/unintended lead to a dichotomous “yes” or “no”. There was no standardization in which this question was raised by healthcare professionals in the clinic and requires robust longitudinal research to aid healthcare professionals and FQHCs nationwide. Lastly, though postpartum depression most commonly occurs within six weeks after childbirth, this was not a longitudinal study. Lack of long term follow up may have misclassified patients who develop postpartum depression beyond the initial six week time frame used by the current study [13,14].
Future investigations should focus on using a more standardized approach to reporting pregnancy intention at the initial prenatal visit. There is the London Measure of Unplanned Pregnancy (LUMP) which is a psychometrically validated measure of the degree of intention/ planning of a current or recent pregnancy and categorizes pregnancy intention into “planned”, “ambivalent”, “unplanned”. It was found in recent follow up studies to be reliable and valid in US English and Spanish translation for studying pregnancy intention.
Conclusion
In our study, more patients who screened positive for postpartum depression characterized their pregnancy as unintended. Implementation of nationwide family planning services publicly funded through Title X has been estimated to have reduced unintended pregnancy rates by 35% and resulted in net public savings of up to $10.5 billion. However this still translates to about 2.8 million unintended pregnancies. An association between pregnancy intention and maternal pregnancy outcomes would provide evidence to support ways to improve postpartum contraception use with aims to continue to decrease rates of unintended pregnancies and short interval pregnancies. Measures such as introducing immediate postpartum long-acting reversible contraception and providing access to birth control method options prior to discharge from birthing centers or hospitals after delivery should continue to be supported by policymakers. Pregnancy intention should be considered an important influencer of maternal morbidity and mortality. Its impact may not be immediate, but our study supports examining more long term outcomes related to maternal health, including mental health.
Disclosure
Chi Son Kim is a non paid trainer for Merck Nexplanon®.
Funding
No funding for this research project.
Acknowledgement
No potential conflicts of interest; this is not industry sponsored research.
Author’s Contribution
The authors thank Thomas E. Wasser, PhD, Med, CIM, for his contribution to this study.
References
- Finer LB, Zolna MR (2016) Declines in unintended pregnancy in the United States, 2008-2011. N Engl J Med 9: 843-852.
[Crossref] [Google Scholar] [PubMed]
- Quinn DA, Sileanu FE, Zhao X, Mor MK, Judge-Golden C, et al. (2020) History of unintended pregnancy and patterns of contraceptive use among racial and ethnic minority women veterans. Am J Obstet Gynecol 4: 564-571.
[Crossref] [Google Scholar] [PubMed]
- Dibaba Y, Fantahun M, Hindin MJ (2013) The effects of pregnancy intention on the use of antenatal care services: Systematic review and meta-analysis. Reprod Health 10: 1-9.
[Crossref] [Google Scholar] [PubMed]
- Cheng D, Schwarz EB, Douglas E, Horon I (2009) Unintended pregnancy and associated maternal preconception, prenatal and postpartum behaviors. Contraception 79: 194-8.
[Crossref] [Google Scholar] [PubMed]
- de La Rochebrochard E, Joshi H (2013) Children born after unplanned pregnancies and cognitive development at 3 years: Social differentials in the United Kingdom millennium cohort. Am J Epidemiol 6: 910-920.
[Crossref] [Google Scholar] [PubMed]
- Hall JA, Benton L, Copas A, Stephenson J (2017) Pregnancy intention and pregnancy outcome: Systematic review and meta-analysis. Matern Child Health 21: 670-704.
[Crossref] [Google Scholar] [PubMed]
- Barton K, Redshaw M, Quigley MA, Carson C (2017) Unplanned pregnancy and subsequent psychological distress in partnered women: A cross-sectional study of the role of relationship quality and wider social support. BMC Pregnancy Childbirth 17: 1-9.
[Crossref] [Google Scholar] [PubMed]
- Bahk J, Yun SC, Kim YM, Khang YH (2015) Impact of unintended pregnancy on maternal mental health: A causal analysis using follow up data of the Panel Study on Korean Children (PSKC). BMC Pregnancy Childbirth 1: 1-2.
[Crossref] [Google Scholar] [PubMed]
- Pearlstein T, Howard M, Salisbury A, Zlotnick C (2009) Postpartum depression. Am J Obstet Gynecol 4: 357-64.
[Crossref] [Google Scholar] [PubMed]
- Slomian J, Honvo G, Emonts P, Reginster JY, Bruyere O (2019) Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Women's Health 15: 14-28.
[Crossref] [Google Scholar] [PubMed]
- Abajobir AA, Maravilla JC, Alati R, Najman JM (2016) A systematic review and meta-analysis of the association between unintended pregnancy and perinatal depression. J Affect Disord 192: 56-63.
[Crossref] [Google Scholar] [PubMed]
- Jiang M, Mishu MM, Lu D, Yin X (2018) A case control study of risk factors and neonatal outcomes of preterm birth. Taiwan J Obstet Gynecol 57: 814-818.
[Crossref] [Google Scholar] [PubMed]
- Kilpatrick SK, Ecker JL (2016) American college of obstetricians and gynecologists. Severe maternal morbidity: Screening and review. Am J Obstet Gynecol 215: 17-22.
[Crossref] [Google Scholar] [PubMed]
- Gibson J, McKenzieâ?ÂMcHarg K, Shakespeare J, Price J, Gray R (2009) A systematic review of studies validating the edinburgh postnatal depression scale in antepartum and postpartum women. Acta Psychiatrica Scandinavica 119: 350-364.
[Crossref] [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi 



