Mini Review, J Appl Bioinforma Comput Biol Vol: 12 Issue: 2
Interactions of Glycrhizzin with the Peri-Implant Microbiome, an Analysis of Molecular Mechanisms using In Silico Validation Tools
Karthickraj S1, Sahana Selvaganesh1* and Thiyaneswaran N2
1Department of Implantology, Saveetha University, Chennai, India
2Department of Prosthodontics and Implantology, Saveetha University, Chennai, India
*Corresponding Author: Sahana Selvaganesh
Department of Implantology, Saveetha University, Chennai, India
Tel: 9444964693
E-mail: sahanaselvaganesh@gmail.com
Received date: 08 November, 2022, Manuscript No. JABCB-23-79270;
Editor assigned date: 11 November, 2022, PreQC No. JABCB-23-79270 (PQ);
Reviewed date: 25 November, 2022, QC No. JABCB-23-79270;
Revised date: 08 February, 2023, Manuscript No. JABCB-23-79270 (R);
Published date: 15 February, 2023, DOI: 10.4172/2329-9533.1000257
Citation: Karthickraj S, Selvaganesh S, Thiyaneswaran N (2023) Interactions of Glycrhizzin with the Peri-Implant Microbiome, an Analysis of Molecular Mechanisms using In Silico Validation Tools. J Appl Bioinforma Comput Biol 12:2.
Abstract
Dental implants are almost replacing all the tooth supported fixed prothesis as it involves extra two teeth for replacing a single tooth which are missing. The survival rates of implants are also about 96.4% to 99% over a period of 10 years. The primary concern is the healing period which is quite longer than fixed prosthesis and maintenance is also a major concern for the survival of the implant. It has been observed that patients who have multiple implants, when they lost one implant due to peri implant disease the risk of losing the other implants due to the same cause increases multifold times. This study is to evaluate whether the use of glycyrrhizin will have any impact on the peri implantitis causing microbes and relate with the medications that can be used in the near future.
Keywords: Peri-implant; Staphylococcus aureus; Tannerella forsythia; Bacteroides fragilis
Introduction
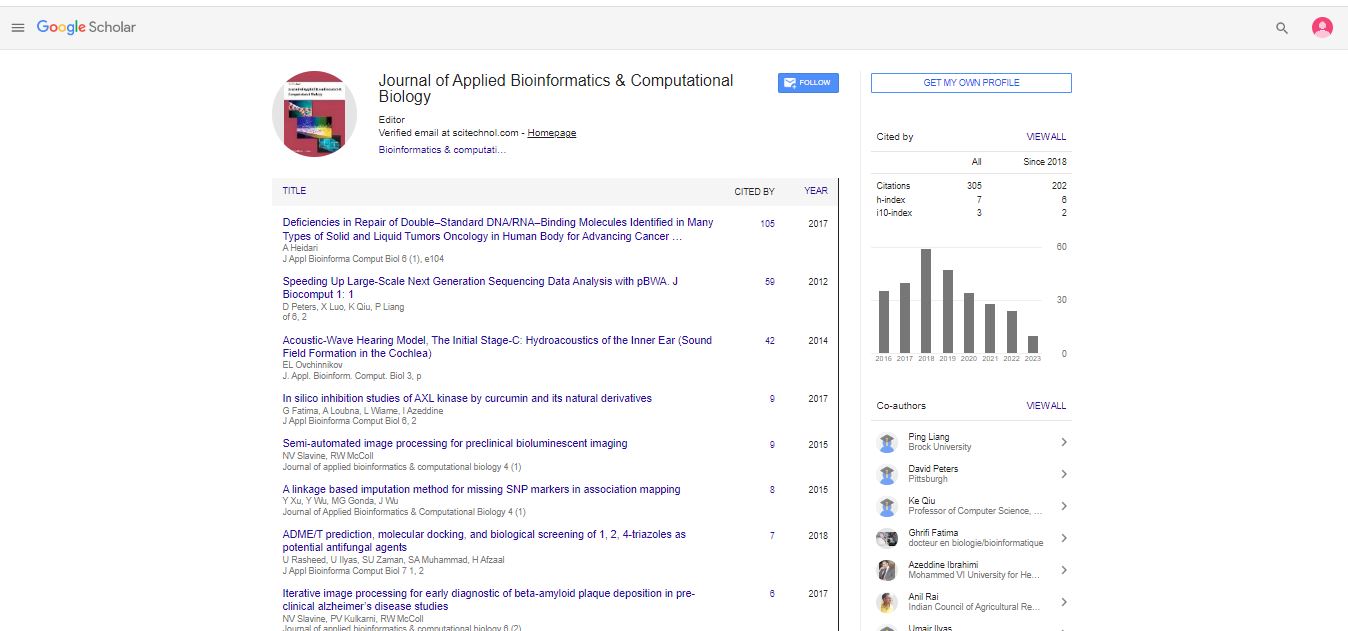
This study is mainly find that the microbes will against certain Aggregatibacter actinomycetemcomitans (D7S-1), Centipeda periodontii (ATCC 35019), Campylobacter gracilis (RM3268), Fusobacterium nucleatum (ATCC 25586), Slackia exigua (ATCC 700122), Prevotella intermedia (ATCC 700821), Tannerella forsythia (ATCC 43037), Staphylococcus aureus (NCTC8325), Bacteroides fragilis (ATCC25285) and their interactions with glycyrrhizin are evaluated using STITCH v.5 and the virulence properties of the interacting proteins were deduced using VICMpred and virulentpred software [1]. The given bacterial strains were included in the STITCH database and analysis was done using a user defined query [2].
Literature Review
Prediction of bacterial protein and metal oxide interactions
STITCH database (Version 5) is an open source platform with an exhaustive collection of data about interactions both physical and functional associations made possible by computational prediction of interactions from primary databases Szklarczyk D, et al. the repertoire of proteins which interacts with A. actinomycetemcomitans (D7S-1), B. fragilis (ATCC 25285), C. gracilis (RM 3268), F. nucleatum (ATCC 10953), P. gingivalis (ATCC 33277), T. denticola (ATCC 35405), S. exigua (ATCC700122) and T. forsythia (ATCC 43037) [3].
Prediction of subcellular localization of the virulent protein
Subcellular localization of proteins helps in the identification of drug targets and could serve as a potential target for new medicines, cell surface proteins are of great interest as they can be used as novel drug targets [4]. Gneg-mPLoc is an algorithm that assigns a probable localization site to a protein from an amino acid sequence provided [5].
The STITCH v5 tool was used to evaluate the interaction between the microbe and element of interest, the protein target derivatives of the reactions were further processed with algorithms of VICMpred and virulentpred to categorize the outcomes as virulent and avirulent. Glycyrrhizin as a molecule was found to react with proteins involved with cellular metabolism, and cellular processes [6-8]. It is interesting to observe that the element of interest also interacted with virulence factors of the peri-implant pathogens the most common interactions involved enzymes glutaminase, glutamine synthetase, and superoxide group of enzymes which are primarily involved in nitrogen metabolism and, enzymes involved in free radical production [9]. In addition to these predictions, the subcellular localization of the ten virulent factors and epitope analysis was also carried out and most of the proteins targeted were found to be present at the cytoplasmperiplasm compartment [10].
Discussion
A cause and effect relationship between peri-implant biofilms and peri-implant mucositis has been observed, the microflora on initial examination was thought to be similar to that of periodontitis more specifically the red complex bacteria, initial colonization of peri-implant surfaces by bacteria can occur in a matter of 2 weeks and reports state that there is a difference in the total bacterial count between implants affected by the disease compared to that of healthy peri-implant tissue and the microflora is distinct than that of periodontitis [11-14]. More recently due to improved sample processing techniques investigations revealed that the peri-implant biofilm is a complex ecosystem comprised of mixed, rather variable and in most cases dominated by gram negative anaerobic bacteria, based on available evidences the most common species found to be present are Porphyromonas gingivalis, Tannerella forsythia, Treponema denticola, Aggregatibacter actinomycetemcomitans, Prevotella intermedia, Fusobacterium nucleatum, Campylobacter species, and Bacteroides species, thus these strains were considered for this study. No metal or metal alloy is completely inert in vivo because of constant contact with tissues, body fluids which in turn acts as a source for electrochemical interactions and, mechanical loading of the implant leads to loss of ions by friction and electrochemical exchange, this process is referred to as bio tribocorrosion, it has also been suggested that long standing accumulation of biofilms and mechanical strain causes implant surfaces to deteriorate and the ability to implant surface to re- passivate also tends to reduce as the inflammatory response and mechanical wear persists [15]. Presence of high levels of dissolved titanium was detected in submucosal plaque around implants when compared to intervention free sites, thus indicating an association between Ti dissolution and peri-implantitis [16]. The oxide corrosion products were found in newly formed trabecular bone and peri-implant vasculature and systemically distributed, the oxide particles tend to be cytotoxic having an effect on the cells of immunity and it has been noted that smaller the particle size greater the toxicity, this particle also has an influence on host immunity causing activation of macrophage and consequently IL-1 β release the cascade of events leads to osteoclastogenesis and osteolysis. Other workers have observed peri-implantitis to be present in situations where the microbial threat is removed or under control through frequent supportive measures, there is evidence which proposes that titanium oxide debris causes immune-modulatory changes which bring about degenerative changes in osseous and periodontal tissues, this is because of the fact that immune cells around the implant that is the polymorphonuclear neutrophils, macrophages and monocytes recognize the implant as a foreign body, and release various signalling molecules such as reactive oxygen species, IL-8, TNF α, IL-6, IL-4, IL-10 which in turn affect the osteogenic capacity of the osteoblasts that adhere to that material surface, it has been proposed that surfaces roughness of the implant has a significant immunomodulatory effects and that the macrophages tended to polarise towards a classical M1 phenotype which upon activation are known to secrete high levels of proinflammatory cytokines [17]. However it is interesting to note that TiO2 has a continuous photocatalytic antimicrobial activity against pathogens, this metal oxide alone or in combination with other metals like silver, copper or zinc is shown to have antimicrobial property and the same has been explored to a lesser extent [18]. In the present study we observe a good number of interactions between TiO2 and common peri-implant pathogens the target was mostly enzymes involved in cellular nitrogen metabolism which in turn brings about alteration in protein synthesis hindering the ability of bacteria cause virulence, thus it can be taken that titanium modifies peri-implant microbiome and has potential antibacterial activity much light has to be shed on this aspect and the same would be clinically useful in management of peri-implant disease by modifying implant surfaces or and we can deduce that peri-implantitis is a complex disorder which has multifactorial causation, and more experimental exploration on this aspect to be carried out to produce effective treatment outcomes [19].
Conclusion
Peri-implantitis is one of the major concern which influences the success rate of dental implants, however effective the treatment plan be the occurrence of this inflammatory disease is unavoidable at times, from this observation we draw to a conclusion that glycyrrhizin indeed undergoes degenerative changes and has the potential to modify the peri implant micro flora by interacting with the their metabolic processes and could potentially increase the auto immune response that one could expect.
Author Contributions
First author (Karthickraj S) performed the analysis and interpretation and wrote the manuscript. Second author (Sahana Selvaganesh) contributed to conception, data design, analysis, interpretation and critically revised the manuscript. Third author (Thiyaneswaran N) critically reviewed the manuscript. All the authors have discussed results and revised the manuscript.
Conflict of Interest
The authors declare no conflict of interest, financial or otherwise.
References
- Moraschini V, Poubel LD, Ferreira VF, dos Sp Barboza E (2015) Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: A systematic review. Int J Oral Maxillofac Surg 44:377-388.
[Crossref] [Google Scholar] [PubMed]
- Van Velzen FJ, Ofec R, Schulten EA, Ten Bruggenkate CM (2015) 10-year survival rate and the incidence of peri-implant disease of 374 titanium dental implants with a SLA surface: A prospective cohort study in 177 fully and partially edentulous patients. Clin Oral Implants Res 26:1121-1128.
[Crossref] [Google Scholar] [PubMed]
- Schwarz F, Derks J, Monje A, Wang HL (2018) Peri implantitis. J Clin Periodontol 45:S246-S266.
[Crossref] [Google Scholar] [PubMed]
- Mombelli A, Muller N, Cionca N (2012) The epidemiology of peri implantitis. Clin Oral Implants Res 23:67-76.
[Crossref] [Google Scholar] [PubMed]
- Hutton JE, Heath MR, Chai JY, Harnett J, Jemt T, et al. (1995) Factors related to success and failure rates at 3 year follow-up in a multicenter study of overdentures supported by branemark implants. Int J Oral Maxillofac Implants 10:33-42.
- Weyant RJ, Burt BA (1993) An assessment of survival rates and within-patient clustering of failures for endosseous oral implants. J Dent Res 72:2-8.
[Crossref] [Google Scholar] [PubMed]
- Jespersen MC, Peters B, Nielsen M, Marcatili P (2017) BepiPred-2.0: Improving sequence based B cell epitope prediction using conformational epitopes. Nucleic Acids Res 45:W24-W29.
[Crossref] [Google Scholar] [PubMed]
- Yu NY, Wagner JR, Laird MR, Melli G, Rey S, et al. (2010) PSORTb 3.0: Improved protein subcellular localization prediction with refined localization subcategories and predictive capabilities for all prokaryotes. Bioinformatics 26:1608-1615.
[Crossref] [Google Scholar] [PubMed]
- Hong-Bin Shen and Kuo-Chen Chou (2010) Gneg-mPLoc: A top-down strategy to enhance the quality of predicting subcellular localization of gram negative bacterial proteins. J Theor Biol 264:326-333.
[Crossref] [Google Scholar] [PubMed]
- Saha S, Raghava GP (2006) VICMpred: An SVM based method for the prediction of functional proteins of gram negative bacteria using amino acid patterns and composition. Genomics Proteomics Bioinformatics 4:42-47.
[Crossref] [Google Scholar] [PubMed]
- Szklarczyk D, Santos A, Von Mering C, Jensen LJ, Bork P, et al. (2016) STITCH 5: Augmenting protein chemical interaction networks with tissue and affinity data. Nucleic Acids Res 44:D380-D384.
[Crossref] [Google Scholar] [PubMed]
- Sahrmann P, Gilli F, Wiedemeier DB, Attin T, Schmidlin PR, et al. (2020) The microbiome of peri implantitis: A systematic review and meta-analysis. Microorganisms 8:661.
[Crossref] [Google Scholar] [PubMed]
- Heitz-Mayfield L, Lang NP (2010) Comparative biology of chronic and aggressive periodontitis vs. peri implantitis. Periodontol 2000 53:167-181.
[Crossref] [Google Scholar] [PubMed]
- Ata-Ali J, Candel-Marti ME, Flichy-Fernandez AJ, Penarrocha-Oltra D, Balaguer-Martinez JF, et al. (2011) Peri implantitis: Associated microbiota and treatment. Med Oral Patol Oral Cir Bucal 16:e937-e943.
[Crossref] [Google Scholar] [PubMed]
- Charalampakis G, Belibasakis GN (2015) Microbiome of peri implant infections: Lessons from conventional, molecular and metagenomic analyses. Virulence 6:183-187.
[Crossref] [Google Scholar] [PubMed]
- Daubert D, Pozhitkov A, McLean J, Kotsakis G (2018) Titanium as a modifier of the peri implant microbiome structure. Clin Implant Dent Relat Res 20:945-953.
[Crossref] [Google Scholar] [PubMed]
- Quirynen M, Vogels R, Pauwels M, Haffajee AD, Socransky SS, et al. (2005) Initial subgingival colonization of pristine pockets. J Dent Res 84:340-344.
[Crossref] [Google Scholar] [PubMed]
- Zhuang LF, Watt RM, Mattheos N, Si MS, Lai HC, et al. (2016) Periodontal and peri implant microbiota in patients with healthy and inflamed periodontal and peri implant tissues. Clin Oral Implants Res 27:13-21.
[Crossref] [Google Scholar] [PubMed]
- Tallarico M, Canullo L, Caneva M, Ozcan M (2017) Microbial colonization at the implant abutment interface and its possible influence on peri-implantitis: A systematic review and meta-analysis. J Prosthodont Res61:233-241.
[Crossref] [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi