Case Report, J Womens Health Vol: 13 Issue: 3
Invasive Cornual Mole in a Pre-Menopausal Woman: About a Case and the Review of Literature
Ould Dedda*, Hassine Houjaj, MH Alami, Filali A and Bezad R
1Department of Molecular Embryology, Osaka Women’s and Children’s Hospital, Osaka, Japan
*Corresponding Author: Ould Dedda,
Department of Molecular Embryology, Osaka
Children’s Women’s and Hospital, Osaka, Japan
E-mail: nobitaniyan19@gmail.com
Received date: 17 April, 2024, Manuscript No. JWHIC-24-132413;
Editor assigned date: 19 April, 2024, PreQC No. JWHIC-24-132413 (PQ);
Reviewed date: 03 May, 2024, QC No. JWHIC-24-132413;
Revised date: 10 May, 2024, Manuscript No. JWHIC-24-132413 (R);
Published date: 17 May, 2024 DOI: 10.4172/2325-9795.1000497.
Citation: Dedda O, Houjaj H, Alami MH, Filali A, Bezad R (2024) Invasive Cornual Mole in a Pre-Menopausal Woman: About a Case and the Review of Literature. J Womens Health 13:3.
Abstract
Cornual pregnancy is a rare form of ectopic pregnancy and only 2% to 4% of ectopic pregnancies develop in the cornual region of the uterus. Cornual pregnancy is one of the most dangerous types of ectopic pregnancy with a mortality rate of 2.0%-2.5%. Hydatidiform mole is a common form of gestational trophoblastic disease. The incidence of complete hydatidiform moles is approximately 1 to 3 per 1,000 pregnancies. An invasive hydatidiform mole can occur following a molar pregnancy and the incidence is 1 in 15,000 pregnancies.
We report one of the rarest pathologies: A patient suffering from an invasive cornual mole which remains extremely rare in a woman in pre-menopause. Although in the world literature the occurrence of gestational trophoblastic disease is generally in women of childbearing age, the diagnosis of invasive mole should always be considered. Hysterectomy remains a radical option available in a woman in peri-menopause, which was the therapeutic decision in our patient after a negative extension assessment with simple operative consequences.
Keywords: Ectopic Pregnancy (EUG); Gestational Trophoblastic Disease (GTD); Abnormal proliferation; Choriocarcinoma; Hydatiform
Introduction
Ectopic Pregnancy (EUG) represents 1%-3% of pregnancies [1]. Cornual location, defined by the implantation of a gestational sac in the horn of a uterus, occurs in 2% of cases [2]. Gestational Trophoblastic Disease (GTD) is a term used to refer to a group of pregnancy-related tumors and is characterized by abnormal proliferation of the trophoblastic layer of the placenta.
GTD typically occurs in women of childbearing age (between 13 and 49 years) and is one of the few curable malignancies, even in advanced stages of the disease and with widespread metastases. Choriocarcinoma and invasive hydatiform mole respond well to chemotherapy. Low-risk tumors are treated with single-agent chemotherapy, while high-risk tumors are treated with combination chemotherapy [3,4].
The main risk factors for GTD include pregnancies under 15 and over 45 years of age, the presence of spontaneous abortion or a hydatidiform mole in previous pregnancies in the medical history, vitamin A deficiency, ethnicity and environmental factors, prolonged use of oral contraceptives and paternal factors in particular. It is a gynecological disease rather rarely observed in the postmenopausal period [5,6]. Hysterectomy, although rare nowadays, can constitute a primary treatment for women with non-metastatic GTD if the patient does not want a pregnancy [7]. In the literature, few cases of invasive mole in perimenopause have been reported to date.
We report the case of a 50 year old woman in pre-menopause, B+, without ATCD, G4P2
• G1: EV/VH for SFA in 2005, from BDPM.
• G2: EV/VB in 2009, from BDPM.
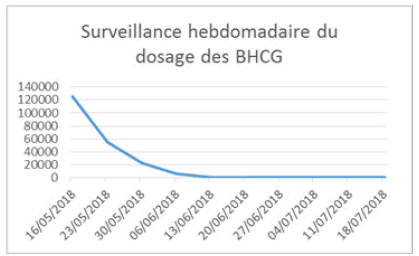
• G3: Hydatidiform mole in 2018 (at 45 years old) followed up in training, initial B-HCG of 05/09/2018 (before aspiration): 125,316 mIU/ml.
• Echo: Heterogeneous honeycomb image (68/43 mm) no lutein cyst. No signs of myometrial invasion.
• Extension assessment: Normal, FIGO prognostic score for gestational trophoblastic tumors at 11 (i.e. high risk) without the presence of metastases.
Suction two times
• 10/05/2018: Anapath-complete hydatidiform mole, absence of malignant lesion,
• 05/25/2018: For retention of 39*28 mm (Echo of 05/23/2018), Weekly monitoring of HCG with negativation of HCG on 3 values in 7 weeks, Follow-up for 01 and half years,
• Last HCG on 03/10/2019: Negative, the patient did not have effective contraception (condoms) (Figure 1).
Consulted externally for SUA type of menometrorrhagia for 02 months and exaggeration of the sympathetic signs of pregnancy and pelvic pain is addressed to the training for pec of a GA.
• Echo: Clear egg of 6SA+4 days, Patient was admitted to the GA circuit with control echoes, hospitalized on 03/30/2023 for aspiration.
• In the operating room on 03/31/2023: Attempt at echo-guided aspiration using a Karman cannula not bringing back any trophoblast with sensation of hard formation intrauterine is stopping the aspiration.
• HCG on 03/31/2023: 23228 mIU/ml.
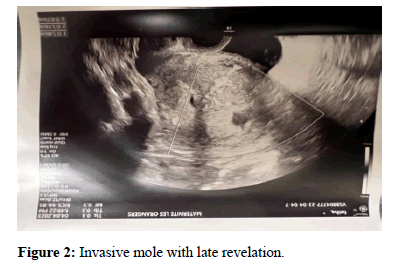
• Pelvic ultrasound: Vascularized right cornual myometrial lesion with a necrotic site.
• Ovaries: Not seen,
• HCG control from 04/05/2023; 22267,
• Extension assessment+BPO+Cardio opinion; requested (Figure 2),
• D c to mention,
• C horiocarcinoma,
• Implantation site tumor.
Results and Discussion
Cornual pregnancy is a rare form of ectopic pregnancy and only 2%-4% of ectopic pregnancies develop in the cornual region of the uterus. Cornual pregnancy is one of the most dangerous types of ectopic pregnancy with a mortality rate of 2.0%-2.5% [8]. Due to the abundant blood supply to the corneal region and the thinning of the myometrium, severe hemorrhage and even death sometimes occurred due to rupture of the cornea. Its management is not standardized and often guided by the clinical situation. The treatment requires an evacuation of the pregnancy and turbinate hemostasis if necessary [9].
Hydatidiform mole is a common form of gestational trophoblastic disease. The incidence of complete hydatidiform moles is approximately 1 to 3 per 1,000 pregnancies. An invasive hydatidiform mole can occur following a molar pregnancy and the incidence is 1 in 15,000 pregnancies [10,11]. In the world literature, the occurrence of GTD in women over 50 years old is rare. Rabczynski et al., reported a case of CHM in a 59 year old woman [12]. Fouchardiere et al., found an invasive hydatidiform mole in a 51 year old postmenopausal patient [13].
In the study by Tsukamoto et al., 20 cases of gestational trophoblastic disease in women aged 50 years or older were reported [14]. The lesions were seven moles hydatiform (35%), eight invasive moles (40%) and five choriocarcinomas (25%). However, none of the patients with hydatidiform mole were postmenopausal. They suggest that due to the high rate (56.3%) of malignant sequelae after evacuation of molars, primary hysterectomy for the treatment of hydatidiform mole in this age group is recommended [15].
Ultrasound is the most sensitive method for the complete diagnosis of molar pregnancy. It is possible to see the characteristic vesicular appearance which is the result of hydropic degeneration of the chorionic villi and semi and complete hyperplasia. Practitioners used the term cornual pregnancy to refer to gestations that occur near the uterine horn, which is the junction of the oviduct and uterus [16].
The appearance of a hydatidiform mole associated with an ectopic pregnancy is a very rare situation. Fewer than 300 cases of ectopic molar pregnancies have been reported, of which 10% involved the uterine horn [17]. Hwang et al., had previously reported a rare case of molar cornual ectopic pregnancy, which was successfully treated by the combination of laparoscopic cornuostomy and systemic treatment with methotrexate [18]. Invasive cornual hydatidiform mole is extremely rare. If Oskovi et al., had previously reported a case of invasive molar pregnancy in the rudimentary uterine horn [19,20].
Treatment for both cases all consisted of rudimentary resection of the horns. In our case, there was no congenital uterine anomaly. To the best of our knowledge, a single case of cornual hydatidiform mole invasive into an anatomically normal uterus has been reported [21]. Due to the rarity of the disease, the management of invasive cornual hydatidiform mole is not defined and is guided solely by the presenting disease. Future studies still need to confirm whether monochemotherapy could be the only management option for invasive hydatidiform mole.
Cornual pregnancy
In our case, abnormal uterine bleeding and severe anemia appeared. Abnormal uterine bleeding can be caused by the rich blood supply in the uterine horn and the strong invasive capacity of trophoblasts. Suction curettage, chemotherapy and hysterectomy can be applied in the treatment of MTG. The patient's age and desire for fertility as well as postmolar resistance are important when choosing the treatment modality. Monitoring serum HCG levels is important in post-treatment follow-up [22,23].
Cornual pregnancy is one of the most dangerous types of ectopic pregnancy with a mortality rate of 2.0%-2.5% [8]. In our patient a decision for scheduled hysterectomy after negative extension assessment was carried out with simple type consequences. Although gestational trophoblastic disease is rare in peri-menopausal women, the diagnosis of hydatidiform mole should be considered when evaluating postmenopausal patients.
Conclusion
In conclusion, in this study, we report one of the rarest pathologies. A patient suffering from an invasive cornual mole which remains extremely rare in a woman in pre-menopause. Although in the world literature the occurrence of gestational trophoblastic disease is generally in women of childbearing age, the diagnosis of invasive mole should always be considered. Hysterectomy remains a radical option available for a woman in peri-menopause.
References
- Benifla JL, Fernandez H, Sebban E, Darai E, Frydman R, et al. (1996) Alternative to surgery of treatment of unruptured interstitial pregnancy: 15 cases of medical treatment. Eur J Obstet Gynecol Reprod Biol
[Crossref] [Google Scholar] [Pubmed]
- Lau S, Tulandi T (1999) Conservative medical and surgical management of interstitial ectopic pregnancy. Fertil Steril 72(2): 207-215.
[Crossref] [Google Scholar] [Pubmed]
- Berkowitz RS, Goldstein DP (2013) Current advances in the management of gestational trophoblastic disease. Gynecol Oncol 128(1): 3–5.
[Crossref] [Google Scholar] [Pubmed]
- Deng L, Zhang J, Wu T, Lawrie TA (2013) Combination chemotherapy for primary treatment of gestational trophoblastic tumors with high risk. Cochrane Database System Rev 2013(1): CD005196.
[Crossref] [Google Scholar] [Pubmed]
- Palmer JR (1994) Advances in the epidemiology of gestational trophoblastic disease. J Reprod Med 39:155-62.
[Pubmed]
- Berkowitz RS, Goldstein DP (1981) Pathogenesis of gestational trophoblastics neoplasms. Pathobiol Ann 11: 391-411.
[Pubmed]
- Horowitz NS, Goldstein DP, Berkowitz RS (2009) Management of gestational trophoblastic neoplasia. Semin Oncol 36(2):181-189.
[Crossref] [Google Scholar] [Pubmed]
- Xiang Y, Yang X, Du J, Song H (2000) The role of hysterectomy in the therapy of gestational trophoblastic tumor. Chin Med Sci J 15(1): 45-48.
[Google Scholar] [Pubmed]
- Faraj R, Steel M (2007) Management of cornual (interstitial) pregnancy. Obstet Gynecological 9(4): 249-255.
- Prenaud C, Scherier S, Malgras B (2017) Management of a cornual ectopic pregnancy. J Visc Surg 154(6): 467-468.
[Crossref]
- Aminimoghaddam S, Maghsoudnia A (2017) Unusual presentation of a mole invasive: A case report. J Reprod Infertile 18(1): 205-209.
[Google Scholar] [Pubmed]
- Rabczynski J, Kochman A, Prudlak E, Lewandowski M (2000) Hydatidiform mole in a 59-year-old woman: Report of a case. Ginekol Pol 71(3):152–154.
- Fouchardiere A, Cassignol A, Benkiran L, Rudigoz RC, Gougeon A, et al. (2003) Hydatidiform mole invasive in postmenopausal women. Ann Pathol 23(5): 443–446.
- Tsukamoto N, Iwasaka T, Kashimura Y, Uchino H, Kashimura M, et al. (1985) Gestational trophoblastic disease in women aged 50 or over. Gynecol Oncol 20(1): 53-61.
[Crossref] [Google Scholar] [Pubmed]
- Fine C, Bundy AL, Berkowitz RS, Boswell SB, Berezin AF, et al. (1989) Sonographic diagnosis of partial hydatidiform mole. Obstet Gynecol 73(3): 414-418.
[Google Scholar] [Pubmed]
- Finlinson AR, Bollig KJ, Schust DJ (2020) Differentiate pregnancies near the utero-tubal junction (angular, cornual and interstitial): Review and recommendations. Fertil Res Pract 6:8.
[Crossref] [Google Scholar] [Pubmed]
- López CL, Lopes V, Resende FR (2018) Gestational trophoblastic neoplasia after ectopic molar pregnancy: Clinical, diagnostic and therapeutic aspects.
[Crossref] [Google Scholar] [Pubmed]
- Hwang JH, Lee JK, Lee NW (2010) Molar ectopic pregnancy in the uterine cornus. J Minim Invasive Gynecol 17: 239-41.
[Crossref] [Google Scholar] [Pubmed]
- Si Manfei, Li P, Yuan Z, Ma H, Cui B, et al. (2017) An unexpected invasive hydatidiform mole in a rudimentary uterine horn: A case report. Oncol Lett 14(3): 2808-2812.
[Google Scholar] [Pubmed]
- Oskovi KZ, Şirvan AL, Topçu HO (2018) Invasive molar pregnancy in rudimentary uterine horn. J Exp Ther Oncol 12(3): 207-210.
[Google Scholar] [Pubmed]
- Khlifi A, Mkhinini I, Yaacoubi MT, Khairi H (2016) A cornual invasive hydatiform mole: A literature review. Med J Armed Forces India 72:
- Goldstein DP, Berkowitz RS (1995) Proflactic chemotherapy of pregnancy complete molar pregnancy. Semin Oncol 22(2): 157-160.
[Google Scholar] [Pubmed]
- Kim DS, Moon H, Kim KT, Moon YJ, Hwang YY (1986) Effects of prophylactic chemotherapy for persistent trophoblastic disease in patients with a complete hydatidiform mole. Obstet Gynecol 67(5): 690–694.
[Crossref] [Google Scholar] [Pubmed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi